
Delayed subcutaneous emphysema, mediastinal emphysema and pneumothorax after tracheal intubation in a child: a case report
Introduction
Pneumothorax or subcutaneous emphysema or mediastinal emphysema after tracheal intubation is common, especially in elderly patients with an underlying tracheal disease or lung disease. However, the phenomenon of delayed after tracheal intubation is relatively rare in children. Occurrence of pneumothorax/pneumomediastinum of severe tracheal intubation–associated events was 0.2% in North American (1). In this article, we describe the development and recovery process of such a case. We present the following article in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-453/rc).
Case presentation
A 2-year-old girl (weight: 12.0 kg, height: 90.0 cm) was admitted for a 3rd interventional operation to treat retinoblastoma of the right eye, which was first diagnosed 2 months earlier. The preoperative examination revealed no obvious abnormalities. On the 2nd day after admission, supers-elective arterial chemotherapy was performed under general anesthesia.
Anesthesia was induced in theatre and the child was fully monitored. A gaseous induction with oxygen and sevoflurane was used, venous access was established, and atracurium (2.0 mg), midazolam (1.2 mg), ketamine (15 mg), etomidate (5 mg), and propofol (30 mg) were administered. Gentle mask ventilation was performed for 5 min, there was bilateral expansion and the peripheral capillary oxygen saturation (SpO2) was 100%.
The laryngoscopy view was grade 1, and endotracheal intubation (size: 4.5 and depth: 14.0 cm) was successfully completed for the 1st time. The catheter was fixed and the intermittent positive pressure ventilation (IPPV) mode was then applied with a tidal volume (VT) of 10 mL/kg, a respiratory rate (RR) of 20 breaths per minute, an inhalation/respiration ratio of 1:2, and an air/oxygen ratio of 1.1:0.6.
Sevoflurane was used to maintain anesthesia during the operation. The operation was finished 50 minutes later, and spontaneous respiration was restored after 3 minutes, the tracheal tube was removed, and the child was transported to the recovery room. The child was fully awake and returned to the ward about 40 minutes later with a blood pressure of 110/70 mmHg, a heart rate (HR) of 80 beats per minute, an RR of 18 breaths per minute, and a SpO2 of 99%.
Some 4 hour later, the child developed irritability and cyanosis after crying. Apophysis and crepitus under the local skin of the head and neck were checked. An emergency chest X-ray revealed subcutaneous gas in the bilateral neck and chest wall, and the possibility of pneumomediastinum (see Figure 1A). Oxygen was given through a nasal cannula immediately, and a 14-gauge needle was used for the subcutaneous exhaust. A further computed tomography (CT) scan showed slight inflammation in the upper lobe of the right lung and the lower lobes of both lungs, subcutaneous emphysema in the neck and bilateral chest walls, and mediastinal emphysema (see Figure 1B,1C). Changes in the child’s condition were closely observed.

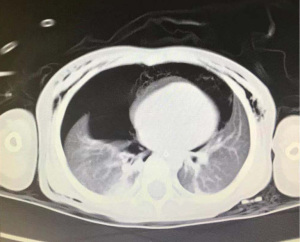
A CT performed on the 2nd day post-surgery showed that the bilateral pneumothorax and right pneumothorax were more obvious than the left pneumothorax, subcutaneous air in the neck and chest wall, pneumomediastinum, and patchy shadows scattered in both lungs (see Figure 2). The patient underwent emergency closed drainage of thoracic cavity, and a chest tube was placed on the right side without any complication. The patient also continued to receive oxygen for symptomatic treatment.
On the 3rd postoperative day, a CT showed a small amount of pneumothorax and partial atelectasis on both sides, and subcutaneous pneumatosis in the neck, mediastinum, and chest wall (see Figure 3A,3B). The drainage tube was removed on the 3rd day after thoracic closed drainage following no gas extraction for 24 h.

A CT examination on postoperative day 4 showed a small amount of subcutaneous gas accumulation in the neck, mediastinum, and chest wall (see Figure 4A,4B). The patient left the hospital (Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine, China), on postoperative day 7, and refuse conduction of fiberoptic bronchoscopy to determine the etiology, and no abnormality was observed in the follow-up after discharge.

All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
When performed by an experienced provider, endotracheal intubation is considered a safe and reliable method for securing an airway in the operating room, intensive care unit, and the emergency department (2). The physiology of the airway differs in pediatric and adult patients (3). Complications and adverse physiological effects [e.g., atelectasis, post-extubation stridor, failed extubation, pneumothorax, accidental extubation, nasal or perioral tissue damage, and ventilator-associated pneumonia (VAP)] of intubation with mechanical ventilation are still unavoidable problems facing anesthesia and clinical physicians (4).
Previous reports have analyzed the common causes of pneumothorax and/or subcutaneous and mediastinal emphysema after mechanical ventilation through endotracheal intubation. They include: the rupture of alveoli or bullae caused by underlying diseases secondary to mechanical ventilation (e.g., pulmonary infection and emphysema), and tracheal intubation or extubation leading to trachea and bronchus injury or rupture (5). Cervical fascia injury may be one of the causes of subcutaneous emphysema with or without pneumomediastinum and pneumothorax (6).
Chest and head and neck surgery are rare in hypopharyngeal injuries. However, cases of delayed mediastinal emphysema and subcutaneous emphysema after extubation and the further development into pneumothorax have rarely been reported, especially in children without obvious pulmonary diseases at the preoperative examination.
In this case, the child experienced multiple subcutaneous emphysema and mediastinum emphysema 4 h after anesthesia recovery and the bilateral pneumothorax 12 h later. If a tracheal intubation injury occurs, air can enter the trachea or bronchial mucosa after minimal damage, extend up to the neck, head and face along the blood vessels, larynx and deep cervical fascia spaces, causing subcutaneous emphysema, and then gradually spread to the mediastinum, resulting in mediastinal emphysema. Discomfort in children leads to irritability and crying, and increased pressure leads to parietal pleura rupture and pneumothorax. The parents in this case refused to allow the child to undergo a diagnostic bronchoscopy due to its high risk, so the cause of delayed subcutaneous emphysema, mediastinal emphysema, and pneumothorax remains uncertain.
It is very important to detect and diagnose subcutaneous emphysema and/or mediastinal emphysema and pneumothorax in patients under general anesthesia. A diagnosis can be established when the airway pressure (Paw) and postapneic end-tidal carbon dioxide pressure (PETCO2) increase, hyperventilation does not improve, SpO2 continuously declines, and at the same time, apophysis and crepitus can be touched under the skin of the neck, face and/or chest. Subcutaneous emphysema of the face and trunk following tracheal intubation should immediately trigger a diagnosis (7). Once subcutaneous emphysema is found, it is necessary to confirm whether pneumothorax and pneumopericardium is present by auscultation and chest X-ray in the operating room. Subcutaneous emphysema can usually be reabsorbed in the absence of drainage, but puncture deflating should be performed in a timely manner to treat severe or life-threatening subcutaneous emphysema of the eyes, face, or airway (8). For tension pneumothorax, the rapid removal of pleural air is the main life-saving measure. The consultation system should be actively improved and further treatment implemented according to the suggestions of specialists.
Endotracheal intubation injury cannot be completely avoided; however, some measures can reduce its incidence, including a pre-anesthetic evaluation, the selection of appropriate anesthetic equipment, especially catheters, and a skilled intubation technique. Preoperative CT or fiberoptic bronchoscopy should be actively performed in patients with a poor airway structure to clarify the airway anatomy, variation, and pathological changes. Non-invasive airway ultrasound provides a new choice for clinical assessments of airway size and can be used to predict the appropriate diameter of endotracheal and tracheostomy tubes (9,10). For patients with airway difficulties, a Macintosh or Miller laryngoscope can be used as an alternative to replace traditional intubation methods, such as video laryngoscopy or fiberoptic bronchoscopy. Noppens et al. confirmed that the success rate of the 1st intubation was higher using video laryngoscope than traditional laryngoscope (11), which can be used to easily observe the openings of the glottis.
The use of a bougie should be avoided as much as possible during intubation, as it may penetrate deep into the distal airway, causing trauma and air leakage (12). If used, the bougie material should be chosen carefully, and close attention should be paid to the insertion depth. The pressure of the endotracheal tube cuff must be appropriate, as under-inflation will cause leakage and overinflation will cause tracheal mucosa tears or even tracheal rupture. During the intubation, excessive backward of head should be avoided. When the intubation passes through the glottis, the movement should be gentle and accurate, and the intubation should be inserted into the cavity area as far as possible to avoid scratching the laryngotracheal mucosa.
In conclusion, subcutaneous and/or mediastinal emphysema and pneumothorax due to endotracheal intubation are not uncommon. Thus, to strengthen the etiology of complications, perioperative observation and postoperative follow-up are important measures for the effective prevention, early diagnosis, and timely treatment of subcutaneous and/or mediastinal emphysema and pneumothorax, and are also conducive to ensuring the safety of patients.
Acknowledgments
We would like to thank the Neurosurgery and Anesthesiology Department of Xinhua Hospital Affiliated to Shanghai Jiaotong University School of Medicine for supporting this work.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-453/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-453/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient’s parents for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lee JH, Nuthall G, Ikeyama T, et al. Tracheal Intubation Practice and Safety Across International PICUs: A Report From National Emergency Airway Registry for Children. Pediatr Crit Care Med 2019;20:1-8. [Crossref] [PubMed]
- Cefalu JN, Williams DC, Joshi TV, et al. Pyriform Sinus Tract Injury After Traumatic Intubation With Resulting Tension Pneumothorax. Ochsner J 2020;20:222-5. [Crossref] [PubMed]
- Wani TM, Bissonnette B, Engelhardt T, et al. The pediatric airway: Historical concepts, new findings, and what matters. Int J Pediatr Otorhinolaryngol 2019;121:29-33. [Crossref] [PubMed]
- Principi T, Fraser DD, Morrison GC, et al. Complications of mechanical ventilation in the pediatric population. Pediatr Pulmonol 2011;46:452-7. [Crossref] [PubMed]
- Jo YY, Park WY, Choi E, et al. Delayed detection of subcutaneous emphysema following routine endotracheal intubation -A case report-. Korean J Anesthesiol 2010;59:220-3. [Crossref] [PubMed]
- Choung HW, Choi YJ, Kang H, et al. Four Different Reasons of Subcutaneous Emphysema With or Without Pneumomediastinum and Pneumothorax After Facial Bone Surgery. J Craniofac Surg 2022;33:e616-20. [Crossref] [PubMed]
- Boutros J, Marquette CH, Ichai C, et al. Multidisciplinary management of tracheobronchial injury. Eur Respir Rev 2022;31:210126. [Crossref] [PubMed]
- Madan K, Mehta S, Gupta N, et al. Pneumomediastinum and Extensive Subcutaneous Emphysema after Cryoprobe Transbronchial Lung Biopsy. Ann Am Thorac Soc 2016;13:2101-3. [Crossref] [PubMed]
- Daniel SJ, Bertolizio G, McHugh T. Airway ultrasound: Point of care in children-The time is now. Paediatr Anaesth 2020;30:347-52. [Crossref] [PubMed]
- Zetlaoui PJ. Ultrasonography for airway management. Anaesth Crit Care Pain Med 2021;40:100821. [Crossref] [PubMed]
- Noppens RR, Geimer S, Eisel N, et al. Endotracheal intubation using the C-MAC® video laryngoscope or the Macintosh laryngoscope: a prospective, comparative study in the ICU. Crit Care 2012;16:R103. [Crossref] [PubMed]
- Walkom A, Preece K. Buckwheat anaphylaxis in a previously non-atopic 11-year-old boy. J Paediatr Child Health 2019;55:374-5. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


