
Analysis of scores of Symptom Checklist 90 (SCL-90) questionnaire of 182 parents of children with spinal muscular atrophy: a cross-sectional study
Introduction
Parents may experience negative emotions such as unease, fear, worry, and anxiety during parenthood due to their own problems, parent-child relationships, the family environment, and other factors (1,2). It has been reported that fathers may also develop negative feelings and fear even during the perinatal period (3). These negative emotions can be aggravated in parents of children with chronic diseases. Research has shown that parents of chronically ill children have higher anxiety and depression scores than parents of healthy children (4). For example, more mothers of children with brachial plexus injury may become depressed, but this was not related to the severity of their children’s illness. (5). Parents of children with developmental disabilities were also at higher risk for depression, and unemployed spouse, low education level, chronic diseases, children with developmental disabilities, and low income are relevant factors (6).
Spinal muscular atrophy (SMA) is an autosomal recessive disorder that causes progressive muscle weakness and atrophy due to a deletion or mutation of the survival motor neuron (SMN) gene (7,8). SMA can be divided into 5 types according to the clinical manifestations: children with type 0 typically die in the first month of life; types I–III begin in childhood and are often accompanied by multiple organ damage as the disease progresses (9); individuals with type IV often develop muscle weakness at the age of 20–30, and the life expectancy is not affected. Families with children and adolescents with SMA show high degrees of stress and strain which are associated with the severity of the disease, reduced social support and child behaviour (10). High stress levels can affect the psychiatric symptoms of parents of children with chronic diseases [such as diabetes, autism spectrum disorder (ASD)] (11,12), so high stress levels maybe also affect the psychiatric symptoms of parents of children with SMA. Attention to the psychiatric symptoms of parents of SMA children can improve the comprehensiveness of family support for SMA children, which is beneficial to the rehabilitation of SMA children. In the past, there are few studies on the psychiatric symptoms of parents of SMA children, and there is a lack of research on the psychiatric symptoms of SMA parents in China. Here, for the first time, we investigated the psychiatric symptoms of parents of children with SMA by the Symptom Checklist 90 (SCL-90) and analyzed its relevant factors (parent’s gender, household area, place of residence, education background, employment, family income, and physical condition, and so on). We present the following article in accordance with the SURGE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-464/rc).
Methods
Subjects
Parents of SMA children aged 0–18 years in a charity WeChat group sponsored by the Meier Advocacy & Support Center for SMA were enrolled as the research subjects. The inclusion criteria were as follows: (I) having a 0–18-year-old child meeting the diagnostic criteria for SMA; (II) an informed and voluntary decision to participate in the survey; and (III) being conscious and able to communicate with researchers and complete the questionnaire and test. The exclusion criteria were as follows: (I) failed to complete the questionnaire; and (II) with severe physical diseases, psychiatric disorders, and/or cognitive dysfunction. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First Hospital of Jilin University (approval No. 2017-314) and informed consent was taken from all patients’ parents or legal guardians.
Basic information questionnaire
This self-designed questionnaire contained the following items: parent’s gender, household area, place of residence, education background, employment, family income, and physical condition; SMA child’s age, living status, duration of disease, medical treatment, and rehabilitation management (including skeletal muscle management, respiratory management, and nutrition management); and rehabilitation training for parents (hospital-based regular training or non-hospital-based non-scheduled training).
Psychiatric symptoms survey tools for parents of SMA children
The SCL-90 was used for psychiatric symptoms screening among parents of SMA children. The SCL-19 is a widely used scale for epidemiological surveys of mental disorders (13,14). The scale reliability was 0.98 (15). The internal consistency reliability of the total score was 0.97 and the factor scores ranged from 0.77 to 0.86 (16). This 90-item questionnaire includes 10 factors: somatization, obsessive-compulsive symptoms, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, psychoticism, and others (mainly reflecting sleep and eating problems). Each item is graded from 1 to 5 according to the severity (none, mild, moderate, severe, and extreme). The scores of these 90 items were summed to create a total score, and the symptoms were regarded as positive when the total score exceeded 160 points. In addition, each factor was scored (factor score = total score of all items contributing to the factor/number of items contributing to the factor), and a factor score of ≥2 indicated positive symptoms. A higher factor score indicated more serious psychiatric symptoms problems.
Survey methods
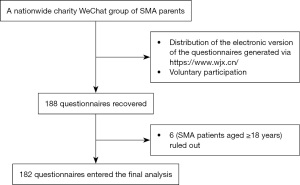
An electronic questionnaire containing basic information and SCL-90 items generated through the https://www.wjx.cn/ website was distributed to parents of SMA children aged 0–18 years in a charity WeChat group sponsored by the Meier Advocacy & Support Center for SMA during the period from August 1 to August 31, 2021. Parents voluntarily participated in the survey and completed the questionnaire forms by mobile phone or computer, which were collected through the https://www.wjx.cn/ website (Figure 1).
Statistical analysis
Statistical analysis was performed using SPSS 19.0 software package (SPSS for Windows, IMB Corp., Armonk, NY, USA). The Kolmogorov-Smirnov test was used to assess data normality. Measurement data are presented as mean ± standard deviation (SD) or median (interquartile range), and count data are expressed as frequencies or percentages. The Spearman test and single-sample t-test were used to assess data correlation/difference, and logistic binary regression was used to analyze the relevant factors of abnormal SCL-90 factors. A P value of <0.05 (two-sided) was considered significantly different.
Results
General information of SMA parents
The respondents were from 182 families in 27 provinces and municipalities. They were located in East China (32 in Shandong, 12 in Jiangsu, 14 in Anhui, 6 in Zhejiang, 9 in Fujian, and 2 in Shanghai), South China (12 in Guangdong, 1 in Guangxi), Central China (6 in Hubei, 4 in Hunan, 9 in Henan, and 6 in Jiangxi), North China (5 in Beijing, 3 in Tianjin, 6 in Hebei, and 4 in Shanxi), Northwest China (1 in Ningxia, 2 in Xinjiang, 6 in Shaanxi, and 2 in Gansu), Southwest China (8 in Sichuan, 6 in Yunnan, 2 in Guizhou, and 2 in Chongqing), and Northeast China (5 in Liaoning, 15 in Jilin, and 2 in Heilongjiang). Female respondents accounted for 84.6% (n=154) and males accounted for 15.4% (n=28). A significantly larger proportion (41.2%) of respondents were from Eastern China. The proportions were also high for respondents who were living in urban areas (63.2%), had a college degree or above (53.8%), were unemployed (52.2%), had a low income (65.4%), and were healthy (89.6%) (Table 1).
Table 1
| Variables | N (%) |
|---|---|
| Gender | |
| Male | 28 (15.4) |
| Female | 154 (84.6) |
| Household area | |
| East China | 75 (41.2) |
| South China | 13 (7.1) |
| Central China | 25 (13.7) |
| North China | 18 (9.9) |
| Northwest China | 11 (6.0) |
| Southwest China | 18 (9.9) |
| Northeast China | 22 (12.1) |
| Place of residence | |
| Urban area | 115 (63.2) |
| Non-urban area | 67 (36.8) |
| Education background | |
| High school or below | 84 (46.2) |
| College or higher | 98 (53.8) |
| Employment | |
| Unemployed | 95 (52.2) |
| Employed | 87 (47.8) |
| Monthly family income | |
| Below 10,000 yuan | 119 (65.4) |
| 10,000 yuan or more | 63 (34.6) |
| Physical condition | |
| Healthy | 163 (89.6) |
| Diseased (not mentally) | 19 (10.4) |
SMA, spinal muscular atrophy.
General information of SMA children
SMA children and adolescents were aged 7–214 months (median: 59 months). A notably high proportion of SMA children lived at home (65.9%), had a disease course of more than 1 year (52.7%), had never used drugs (61.0%), and were currently receiving rehabilitation management (56.6%). More than half (55.5%) of their parents had not received rehabilitation training (Table 2).
Table 2
| Variables | N (%) or median [IQR] |
|---|---|
| Gender | |
| Male | 95 (52.2) |
| Female | 87 (47.8) |
| Age (months) | 59.00 [34.75, 98.50] |
| Living status | |
| Home-living | 120 (65.9) |
| Enrolled in nursery or school | 62 (34.1) |
| Disease course | |
| ≤1 year | 86 (47.3) |
| >1 year | 96 (52.7) |
| Medical treatment | |
| No | 111 (61.0) |
| Yes | 71 (39.0) |
| Rehabilitation management | |
| No | 79 (43.4) |
| Yes | 103 (56.6) |
| Parents receiving rehabilitation training | |
| No | 101 (55.5) |
| Yes | 81 (44.5) |
SMA, spinal muscular atrophy; IQR, interquartile range.
Psychiatric symptoms of SMA parents
Comparison of the SCL-90 scores of 182 SMA parents with the Chinese norms in 2018 (17) showed that the scores of somatization, depression, anxiety, fear, and sleep and eating problems were significantly higher than the national norms (P<0.05), suggesting that parents of children with SMA had a higher risk of developing somatic symptoms, depression, anxiety, fear, and sleep and eating problems than the general population (Table 3).
Table 3
| Factors | National norms (n=12,160) | SMA parents (n=182) | t | P value |
|---|---|---|---|---|
| Somatization | 1.37±0.46 | 1.56±0.80 | 3.147 | 0.002* |
| Obsessive-compulsive symptoms | 1.66±0.58 | 1.72±0.91 | 0.869 | 0.386 |
| Interpersonal sensitivity | 1.51±0.55 | 1.57±0.88 | 0.906 | 0.366 |
| Depression | 1.45±0.53 | 1.78±0.98 | 4.544 | <0.001* |
| Anxiety | 1.40±0.48 | 1.58±0.87 | 2.729 | 0.007* |
| Hostility | 1.48±0.57 | 1.58±0.83 | 1.697 | 0.091 |
| Fear | 1.23±0.39 | 1.39±0.74 | 2.985 | 0.003* |
| Paranoid ideation | 1.41±0.50 | 1.40±0.70 | −0.276 | 0.783 |
| Psychoticism | 1.34±0.44 | 1.42±0.72 | 1.539 | 0.125 |
| Sleep and eating problems | 1.51±0.58 | 1.67±0.87 | 2.488 | 0.014* |
Data are expressed as mean ± SD. *, P<0.05, compared with the 2018 national norms. SCL-90, Symptom Checklist 90; SMA, spinal muscular atrophy; SD, standard deviation.
Relevant factors of psychiatric symptoms in SMA parents
With positive and negative results of the SCL-90 factors including somatization, depression, anxiety, fear, and sleep and eating problems as the outcome categories, the Spearman test was performed to analyze the correlations between the factors in Tables 1,2 and the SCL-90 outcomes. It was found that place of residence was positively correlated with sleep and eating problems (r=0.158, P=0.033) (Table 4), while other factors showed no such correlation (P>0.05) (Tables S1-S5).
Table 4
| Place of residence | Negative, n (%) | Positive, n (%) | r | P value |
|---|---|---|---|---|
| Urban area | 89 (67.9) | 26 (51.0) | 0.158 | 0.033* |
| Non-urban area | 42 (32.1) | 25 (49.0) |
*, P<0.05. SCL-90, Symptom Checklist 90.
Considering the sample size of the present study (n=182) and the common possible relevant factors of parents’ psychiatric symptoms (e.g., social support, financial support, health status of SMA parents, status of SMA children after disease onset, and health care received by SMA children), we used somatization, depression, anxiety, fear, and sleep and eating problems of SMA parents as dependent variables (negative =0, positive =1) and the parents’ household area, place of residence, parents’ education background/employment, family income, parent’s physical condition, children’s age, children’s living status, children’s disease course, medical treatment, and rehabilitation management as covariates. A binary logistic regression model was introduced to determine whether these covariates had independent effects on these 5 abnormal SCL-90 psychiatric symptoms factors.
The categorical variables were coded as follows: household area (East China =0, South China =1, Central China =2, North China =3, Northwest =4, Southwest =5, Northeast =6), place of residence (urban =0, non-urban area =1), education background (high school and below =0, undergraduate and above =1), employment (unemployed =0, employed =1), family income (below 10,000 yuan =0, 10,000 yuan and above =1), physical condition (healthy =0, diseased =1), children’s living status (home =0, nursery or school =1), disease course (1 year and below =0, more than 1 year =1), medication (no =0, yes =1), and rehabilitation management (no =0, yes =1).
The results showed that none of the covariates were relevant factors of somatization and fear (P>0.05) (Table S6). Children’s age [odds ratio (OR) =1.012, P=0.014] and children’s living status (OR =0.360, P=0.031) were relevant factors for parental depression (Figure 2 and Table 5), while the remaining covariates were not correlated with depression (P>0.05) (Table S6). Rehabilitation management (OR =0.409, P=0.038) was the relevant factor of anxiety in SMA parents (Figure 3 and Table 5), while the remaining covariates were not correlated with anxiety (P>0.05) (Table S6). Place of residence (OR =2.602, P=0.017) and physical condition (OR =0.163, P=0.031) were relevant factors of parents’ sleep and eating problems (Figure 4 and Table 5), while the other covariates were not correlated with sleep and eating problems (P>0.05) (Table S6).

Table 5
| Variables | B | OR (95% CI) | P value |
|---|---|---|---|
| Depression | |||
| Age of SMA children | 0.012 | 1.012 | 0.014* |
| Living status of SMA children | −1.023 | 0.360 | 0.031* |
| Anxiety | |||
| Rehabilitation management | −0.894 | 0.409 | 0.038* |
| Sleep and eating problems | |||
| Place of residence | 0.956 | 2.602 | 0.017* |
| Physical condition | −1.812 | 0.163 | 0.031* |
*, P<0.05. B, regression coefficient; SMA, spinal muscular atrophy; OR, odds ratio; CI, confidence interval.


Discussion
SMA is clinically characterized by progressive muscle weakness and atrophy (7,8). As the disease progresses, it is often accompanied by multiple organ damage (9), which affects children’s motor function, living activities, social participation, and even mental health. A mental health survey of 155 school-age children with SMA found that the incidences of anxiety and depression were 40.0% and 25.2%, respectively, and were significantly associated with caregivers’ subjective anxiety (18). In addition, the mental health of the siblings and caregivers of SMA children can also be affected. Siblings of SMA children are 2–3 times more likely to have behavioral problems than the normal population (19). The stress scores of parents of SMA children were significantly higher than those of healthy children (10), which may lead to abnormal parental mental health. A survey of the mental health of home-living mothers of SMA patients (including adults) showed that 76% believed that the burden of caregivers was heavy, 35% were depressed, and 42% were anxious; however, only 38 respondents were mothers of children with SMA (20). Therefore, studies with larger sample sizes are warranted to investigate the psychiatric symptoms of SMA parents.
The SCL-90 was introduced into China in the 1980s and is one of the more popular self-rating scales (21). The scale reliability was 0.98 (15) and the internal consistency reliability of the total score was 0.97. The factor scores ranged from 0.77 to 0.86 (16). During the coronavirus disease 2019 (COVID-19) pandemic, a psychiatric symptoms survey using the SCL-90 scale among front-line medical staff showed that the scores of somatization, depression, anxiety, and fear were higher than normal levels. In particular, the respondents had poor sleep quality, as moderate insomnia accounted for 61.67% and severe insomnia accounted for 26.67% (13,14). The SCL-90 has a total of 90 items, with short questions and simple answers, and take a short time for the respondents. Considering the heavy workload of caring for SMA children, we used this scale to screen the psychiatric symptoms of SMA parents.
Psychiatric symptoms of SMA parents
Limited literature has described the psychiatric symptoms of SMA parents. In a German study focusing on stress and coping in parents of children and adolescents with SMA, the scores of parental environment and stress questionnaires were significantly higher in families with children and adolescents with SMA than the healthy control groups (10). A qualitative study in the United States revealed that caregivers of SMA patients suffered from insomnia and stress (22). Mothers of long-term home-living SMA patients in the Netherlands (n=48) frequently reported disturbed sleep, and the Hospital Anxiety and Depression Scale indicated that the incidence rates of depression and anxiety were 35% and 42%, respectively (20). In Malaysia, 83% (n=24) of caregivers of SMA patients complained of stress, anxiety, and depression (23). In our current study, we compared the SCL-90 scores of 182 parents in 27 provinces with the 2018 national norms in China (17) and found that the scores of depression, anxiety, and sleep and eating problems were higher than those of the general population, which was consistent with previous studies (10,20,22,23). However, the results also showed that the somatization and fear scores of the SCL-90 scale were also higher than those of the general population, which has not been reported in previous studies (10,20,22,23). Somatization is generally related to physiological-pathological factors, psychological factors, and other reactions (24-26). The increase in somatization in SMA parents may be associated with increased stress, impaired sleep, anxiety, and depression when caring for children with SMA. Fear in the SCL-90 scale is basically the same as that reflected in the traditional state of panic attacks (e.g., agoraphobia) and is related to the environmental factors and physiological-pathological factors (such as own health problems and accidental injury) that induce fear (27-29). Since 5 psychological factors increased in SMA parents, further analysis of their relevant factors was essential.
Relevant factors of the psychiatric symptoms of SMA parents
Univariate analysis
Surveys on the parents of children with chronic diseases such as intellectual disability, ASD, cerebral palsy, and type I diabetes revealed that mothers participated more in patient care and may have a greater risk of anxiety and depression than parents of unaffected children (4). In addition, a substantial proportion of mothers (76%) perceived high caregiver burden (20). In our current study, the vast majority (84.6%) of the caregivers were mothers, while fathers accounted for only 15.4%, which was consistent with previous findings. However, not only the mother’s psychiatric symptoms are affected. In our current study, somatization, depression, anxiety, fear, and sleep and eating problems were not correlated with the gender of the parents, suggesting that there was no significant difference between fathers and mothers in terms of psychiatric symptoms problems. The psychiatric symptoms of fathers of SMA children should also be of concern.
Qian et al. (22) summarized 10 thematic areas characterizing the impact of SMA on patients and their parents: (I) confronting premature death; (II) making difficult treatment choices; (III) fearing the loss of functional ability; (IV) coming to terms with lost expectations; (V) loss of sleep and stress; (VI) stigma; (VII) limitations on social activities; (VIII) independence; (IX) uncertainty and helplessness; and (X) family finances. Our self-designed questionnaire included limitations on social activities (parents’ employment and children’s living status) and family finances, whereas insomnia was reflected in the SCL-90 scale. Univariate correlation analysis revealed that non-urban residents were more likely to experience sleep and eating problems. Physical conditions, mental disorders, and psychosocial factors can induce sleep and eating problems (30-32). Compared with urban residents, non-urban residents have less access to medical resources (such as rehabilitation training places and medical insurance systems), social-environmental conditions (such as barrier-free transportation), and parent entertainment facilities. As a result, SMA parents are more likely to develop sleep and eating problems during the care of their SMA children. Our univariate analysis also showed that no other factors other than place of residence were positively correlated with the 5 abnormal psychological factors of the SCL-90 scale. We assumed that the psychiatric symptoms problems in SMA parents might be caused by multiple factors.
Multivariate analysis
In the univariate analysis, only place of residence showed a positive correlation with sleep and eating problems, while the other factors were negatively correlated. Based on previous literature, we assumed that social support, economic support, parents’ physical conditions, children’s status after illness, and medical support offered to the children might have an impact on the psychiatric symptoms of SMA parents. However, a regression analysis with a larger number of factors requires a larger sample size. The sample size of our current study was 182 cases. Therefore, after excluding 3 factors, namely parent’s gender, child’s gender, and parent rehabilitation training, the remaining 11 factors that were more likely to be correlated were used as covariates. A binary logistic regression model was introduced to determine whether these covariates had independent effects on the 5 abnormal psychological factors in the SCL-90.
For parents of children with chronic diseases such as cerebral palsy, ASD, congenital heart disease, and severe chronic diarrheal disease, concerns about their child’s future outcome, excessive family financial expenditure on treatments, prolonged care for the children, reduction of parental entertainment time, and decrease in parents’ social activities can increase parenting pressure and lead to an increased risk of depression and anxiety (4,33,34). Home-living status suggests that the severity of SMA restricts children’ exercises and impairs children’ social functions, making SMA children unable to participate in age-appropriate social activities. With the increase of age, parents’ parenting pressure might increase, thus increasing concerns about their child’s outcomes, which will easily induce depression. Thus, increasing age and home-living status of SMA children are the relevant factors of parental depression in our survey, which also suggests that improving the motor function and increasing social participation of SMA children can help reduce the risk of depression in parents. In addition, according to the clinical manifestations of SMA, home-living children are more likely to have type II or type I SMA (35). Unfortunately, since SMA was not divided into type in our current survey, it was impossible to determine the relationship between SMA type and the risk of parental depression and anxiety. In a similar study, parental and family problems were more pronounced in type I families than in type II and III families, although the “pessimistic” subscales did not differ significantly among different SMA types. In general, families with SMA types I and II experience significantly more stress than those with type III (10). Interventions such as medical treatment or rehabilitation management for children with chronic diseases may gradually stabilize the disease condition and reduce the stress of care, thus alleviating parenting pressure (36-38). Accordingly, psychiatric symptoms problems may be improved. Rehabilitation management can improve the health of individuals with SMA by increasing muscle activation and raising maximum oxygen consumption and workload (39,40). It can control or delay the onset of SMA, which can reduce parenting pressure and promote parents’ psychiatric symptoms. In our current study, we for the first time found that the lack of rehabilitation management was a relevant factor for increased anxiety in SMA parents, which is the first finding compared with previous similar studies (10,20,22,23), suggesting that rehabilitation management in SMA children can relieve or prevent anxiety in SMA parents.
Somatization is typically related to anxiety and depression. Ionescu et al. (41) found that the scores of the Hamilton Anxiety Rating Scale/Hamilton Depression Rating Scale were negatively correlated with the Somatic Symptom Disorder-B Criteria Scale (SSD-12) score, suggesting that the increase in somatization symptoms is more likely to be associated with increased anxiety and depression in SMA parents. Fear is related to environmental factors and physiological-pathological factors (27-29). However, no prominent relevant factor was found to be related to increased fear among SMA parents, which may be due to the effects of multiple factors. Modeling with a larger sample size is warranted.
The impact of place of residence on sleep and eating problems, as seen in the univariate analysis, was also confirmed in the multivariate analysis. Interestingly, parents’ physical health was another relevant factor of sleep and eating problems. It is speculated that parents pay full attention to and take care of SMA children when they are physically healthy. However, increased parenting stress induces abnormal sleep and eating problems, which require further investigations with additional information from parents of healthy children.
In conclusion, the risks of somatization, depression, anxiety, fear, and abnormal sleep and eating states notably increase in the parents of children with SMA (compared with the general population), and the psychiatric symptoms of SMA parents needs to be of concern. Early intervention and prompt rehabilitation management should be offered to improve children’ social functions, thereby improving parents’ psychiatric symptoms. The limitation of this study is that the information collection is not comprehensive (lack of SMA typing, age of parents, etc.), and the sample size needs to be expanded. In addition, studies with larger sample sizes should be conducted to further explore the relevant factors of somatization, fear, and sleep and eating problems in SMA parents, so as to optimize the psychiatric support for this population.
Acknowledgments
Funding: This study was supported by the 6th Youth Fund of The First Hospital of Jilin University (No. 01000880001).
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-464/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-464/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-464/coif). All authors report that this study was supported by the 6th Youth Fund of The First Hospital of Jilin University (No. 01000880001). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the First Hospital of Jilin University (approval No. 2017-314) and informed consent was taken from all patients’ parents or legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eibach RP, Mock SE. Idealizing parenthood to rationalize parental investments. Psychol Sci 2011;22:203-8. [Crossref] [PubMed]
- Zhang Z, Tang Y, Chen X, et al. Development and Reliability and Validity Test to the Parenting Stress Questionnaire for Two-Child Mothers. Front Psychol 2022;13:850479. [Crossref] [PubMed]
- Baldwin S, Malone M, Sandall J, et al. Mental health and wellbeing during the transition to fatherhood: a systematic review of first time fathers' experiences. JBI Database System Rev Implement Rep 2018;16:2118-91. [Crossref] [PubMed]
- Cohn LN, Pechlivanoglou P, Lee Y, et al. Health Outcomes of Parents of Children with Chronic Illness: A Systematic Review and Meta-Analysis. J Pediatr 2020;218:166-177.e2. [Crossref] [PubMed]
- Karadavut KI, Uneri SO. Burnout, depression and anxiety levels in mothers of infants with brachial plexus injury and the effects of recovery on mothers' mental health. Eur J Obstet Gynecol Reprod Biol 2011;157:43-7. [Crossref] [PubMed]
- Gallagher S, Hannigan A. Depression and chronic health conditions in parents of children with and without developmental disabilities: the growing up in Ireland cohort study. Res Dev Disabil 2014;35:448-54. [Crossref] [PubMed]
- Mercuri E, Finkel RS, Muntoni F, et al. Diagnosis and management of spinal muscular atrophy: Part 1: Recommendations for diagnosis, rehabilitation, orthopedic and nutritional care. Neuromuscul Disord 2018;28:103-15. [Crossref] [PubMed]
- Day JW, Finkel RS, Chiriboga CA, et al. Onasemnogene abeparvovec gene therapy for symptomatic infantile-onset spinal muscular atrophy in patients with two copies of SMN2 (STR1VE): an open-label, single-arm, multicentre, phase 3 trial. Lancet Neurol 2021;20:284-93. [Crossref] [PubMed]
- Darbà J. Management and current status of spinal muscular atrophy: a retrospective multicentre claims database analysis. Orphanet J Rare Dis 2020;15:8. [Crossref] [PubMed]
- von Gontard A, Rudnik-Schöneborn S, Zerres K. Stress and coping in parents of children and adolescents with spinal muscular atrophy. Klin Padiatr 2012;224:247-51. [Crossref] [PubMed]
- Cohen LA, Limbers CA. Mental health and parenting stress in mothers of children with diabetes treated in a patient-centred medical home. Fam Pract 2019;36:486-92. [Crossref] [PubMed]
- Teague SJ, Newman LK, Tonge BJ, et al. Caregiver Mental Health, Parenting Practices, and Perceptions of Child Attachment in Children with Autism Spectrum Disorder. J Autism Dev Disord 2018;48:2642-52. [Crossref] [PubMed]
- Hou T, Zhang T, Cai W, et al. Social support and mental health among health care workers during Coronavirus Disease 2019 outbreak: A moderated mediation model. PLoS One 2020;15:e0233831. [Crossref] [PubMed]
- Wu K, Wei X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight Against COVID-19 in China. Med Sci Monit Basic Res 2020;26:e924085. [Crossref] [PubMed]
- Shah SM, Jahangir M, Xu W, et al. Reliability and Validity of the Urdu Version of Psychosomatic Symptoms Scale in Pakistani Patients. Front Psychol 2022;13:861859. [Crossref] [PubMed]
- Yu Y, Wan C, Huebner ES, et al. Psychometric properties of the symptom check list 90 (SCL-90) for Chinese undergraduate students. J Ment Health 2019;28:213-9. [Crossref] [PubMed]
- Liu Y, Wu S, Li Y, et al. A survey of mental symptoms of Chinese population based on SCL-90. Chinese Mental Health Journal 2018;32:437-41.
- Yao M, Xia Y, Feng Y, et al. Anxiety and depression in school-age patients with spinal muscular atrophy: a cross-sectional study. Orphanet J Rare Dis 2021;16:385. [Crossref] [PubMed]
- Laufersweiler-Plass C, Rudnik-Schöneborn S, Zerres K, et al. Behavioural problems in children and adolescents with spinal muscular atrophy and their siblings. Dev Med Child Neurol 2003;45:44-9. [Crossref] [PubMed]
- Cremers CH, Fischer MJ, Kruitwagen-van Reenen ET, et al. Participation and mental well-being of mothers of home-living patients with spinal muscular atrophy. Neuromuscul Disord 2019;29:321-9. [Crossref] [PubMed]
- Dang W, Xu Y, Ji J, et al. Study of the SCL-90 Scale and Changes in the Chinese Norms. Front Psychiatry 2020;11:524395. [Crossref] [PubMed]
- Qian Y, McGraw S, Henne J, et al. Understanding the experiences and needs of individuals with Spinal Muscular Atrophy and their parents: a qualitative study. BMC Neurol 2015;15:217. [Crossref] [PubMed]
- Ch'ng GS, Koh K, Ahmad-Annuar A, et al. A mixed method study on the impact of living with spinal muscular atrophy in Malaysia from patients' and caregivers' perspectives. Orphanet J Rare Dis 2022;17:200. [Crossref] [PubMed]
- Mayou R. Somatization. Psychother Psychosom 1993;59:69-83. [Crossref] [PubMed]
- Polo-Morales A, Alcocer-Salas Á, Rodríguez-Violante M, et al. Association Between Somatization and Nonmotor Symptoms Severity in People With Parkinson Disease. J Geriatr Psychiatry Neurol 2021;34:60-5. [Crossref] [PubMed]
- Li H, Zhang Y, Wang H, et al. The Relationship Between Symptoms of Anxiety and Somatic Symptoms in Health Professionals During the Coronavirus Disease 2019 Pandemic. Neuropsychiatr Dis Treat 2020;16:3153-61. [Crossref] [PubMed]
- Puertas-Gonzalez JA, Mariño-Narvaez C, Peralta-Ramirez MI, et al. The psychological impact of the COVID-19 pandemic on pregnant women. Psychiatry Res 2021;301:113978. [Crossref] [PubMed]
- Chen LX, Ma L, Zhu YF. Mental health status and its influencing factors of nurses in geriatric department after workplace violence. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2021;39:578-82. [PubMed]
- Wroot H, Afzal AR, Forbes C, et al. Fear of cancer recurrence among survivors of childhood cancer. Psychooncology 2020;29:1132-40. [Crossref] [PubMed]
- Horwood L, Mok E, Li P, et al. Prevalence of sleep problems and sleep-related characteristics in preschool- and school-aged children with cerebral palsy. Sleep Med 2018;50:1-6. [Crossref] [PubMed]
- Horenstein A, Morrison AS, Goldin P, et al. Sleep quality and treatment of social anxiety disorder. Anxiety Stress Coping 2019;32:387-98. [Crossref] [PubMed]
- Cotter EW, Kelly NR. Stress-related eating, mindfulness, and obesity. Health Psychol 2018;37:516-25. [Crossref] [PubMed]
- Roberts SD, Kazazian V, Ford MK, et al. The association between parent stress, coping and mental health, and neurodevelopmental outcomes of infants with congenital heart disease. Clin Neuropsychol 2021;35:948-72. [Crossref] [PubMed]
- Giannakopoulos G, Margoni D, Chouliaras G, et al. Child and Parent Mental Health Problems in Pediatric Celiac Disease: A Prospective Study. J Pediatr Gastroenterol Nutr 2020;71:315-20. [Crossref] [PubMed]
- Trucco F, Ridout D, Scoto M, et al. Respiratory Trajectories in Type 2 and 3 Spinal Muscular Atrophy in the iSMAC Cohort Study. Neurology 2021;96:e587-99. [Crossref] [PubMed]
- Lin CI, Chen KL, Kuan TS, et al. Botulinum toxin injection to improve functional independence and to alleviate parenting stress in a child with advanced pantothenate kinase-associated neurodegeneration: A case report and literature review. Medicine (Baltimore) 2018;97:e10709. [Crossref] [PubMed]
- Ebrahimi E, Mirzaie H, Saeidi Borujeni M, et al. The Effect of Filial Therapy on Depressive Symptoms of Children with Cancer and Their Mother's Depression, Anxiety, and Stress: A Randomized Controlled Trial. Asian Pac J Cancer Prev 2019;20:2935-41. [Crossref] [PubMed]
- Branjerdporn N, Benfer K, Crawford E, et al. Efficacy of early interventions with active parent implementation in low-and-Middle income countries for young children with cerebral palsy to improve child development and parent mental health outcomes: a systematic review. Disabil Rehabil 2022;44:6969-83. [Crossref] [PubMed]
- Nishikawa Y, Watanabe K, Orita N, et al. Influence of hybrid assistive limb gait training on spatial muscle activation patterns in spinal muscular atrophy type III. F1000Res 2021;10:214. [Crossref] [PubMed]
- Heje K, Andersen G, Buch A, et al. High-intensity training in patients with spinal and bulbar muscular atrophy. J Neurol 2019;266:1693-7. [Crossref] [PubMed]
- Ionescu CG, Talasman AA, Badarau IA. Somatization and Sleep Quality on Patients with Comorbid Anxiety/Depression. Maedica (Bucur) 2021;16:246-54. [PubMed]
(English Language Editor: C. Betlazar-Maseh)


