
Surgical workflow and infection prevention and control strategies for patients with COVID-19 during the epidemic in Children’s Hospitals
Highlight box
Key findings
• As the only hospital designated to treat children with COVID-19 in Hubei Province, our hospital effectively implemented the infection prevention and control measures in surgery according to the characteristics of children.
What is known and what is new?
• As a susceptible population for respiratory infections, children are at a higher risk of infection than other groups.
• The
What is the implication, and what should change now?
• These measures ensured the safety of the surgeries and reduced the risk of infection in children and medical staff. To ensure the safety of children and medical staff and prevent the spread of the disease, the surgical workflow and management of all important aspects of the operating room should be continuously improved and refined.
Introduction
In December 2019, a sudden pandemic of Corona Virus Disease 2019 (COVID-19) (1) rapidly swept through Wuhan, Hubei Province, and as the virus spread unchecked, the outbreak spread rapidly across the country. All populations are universally susceptible to COVID-19, which is transmitted via respiratory droplets and close contact. COVID-19 also has the potential of aerosol transmission (2). As a susceptible population for respiratory infections, children are at a higher risk of infection than other groups, as they come in close contact with many infected adults in their families. The early symptoms of COVID-19 infection in children are mild, and pulmonary signs are not obvious. Thus, medical personnel should pay high attention to pediatric patients and identify, isolate, and treat them as early as possible.
On January 30, Wuhan Children’s Hospital, Tongji Medical College, Huazhong University of Science and Technology, which is the only hospital designated to treat children with COVID-19 in Hubei Province, quickly launched various emergency plans to prevent and control the epidemic. During the epidemic, under the guidance of the Technical Guidelines for the Prevention and Control of COVID-19 Infection in Medical Institutions (3), which refer to the Methods for the Surgical Management of Patients with Suspected or Confirmed COVID-19 (4), and in combination with the hospital’s COVID-19 prevention and control requirements, the Guidelines for the Management of Surgical Procedures and Infection Prevention and Control of COVID-19 in Children for Operating Rooms were initially formulated by the operating room staff at the children’s hospital. The department organized timely training on infection control to enhance the knowledge and protective awareness of the surgical staff, and preventive control measures were strictly implemented to ensure that the safety of limited duration surgeries and emergency surgeries. A total of 219 children’s COVID-19 nucleic acid test results did not available and their surgeries were completed during the epidemic. No medical or nursing staff infections and no nosocomial infections occurred as a result of these surgeries. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-463/rc).
Methods
Clinical data
Case data: from January 23 to March 7, 2020, a total of 219 pediatric surgeries were performed in our operating room, including 116 males and 103 females, aged 0–15 years. Due to the urgent condition, nucleic acid samples were taken before operation and emergency surgery was performed at the same time.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Wuhan Children’s Hospital (No. 2021R055-E01) and informed consent was taken from all the patients’ parents or legal guardians.
Workflow and infection prevention and control management
During a period of epidemic prevention and control, in principle, no elective surgeries should be scheduled. For limited duration and emergency surgeries, the operations should be performed according to normal surgical procedures after careful screening according to the symptoms and epidemiological histories of the children, and any child suspected to have COVID-19 should not undergo surgery. If a child is suspected or confirmed to have COVID-19, the case should be reported to the hospital infection department and the medical department, and the infection prevention and control norms should be strictly implemented to ensure the clear division of labor, the implementation of measures, and communication among the operating department, anesthesia department, and operating room (5). If a child who is suspected or confirmed to have COVID-19 requires surgery, the tertiary protection measures should be adopted by the surgical staff.
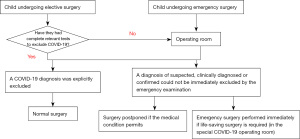
Processing flow for surgical triage
After the surgical notification order was received, a surgical tirage process was adopted (see Figure 1).
Preoperative screening
Before surgery, in addition to the routine verification, detailed inquiries should be made about the close contact history of the child undergoing surgery. After the child patient arrives at the operating room, a routine infrared temperature measurement should be taken, and relevant tests conducted, including routine blood tests, liver and kidney function tests, a 3-dimensional pulmonary CT examination, and severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) nucleic acid detection via throat swabs.
If the child has a preoperative history of fever or respiratory symptoms, the child should be screened based on their contact history, a serological examination, and lung CT. If the child requiring surgery is highly suspected to have COVID-19, but the positive nucleic acid test results for the emergency condition could not be verified, the child should be treated as a patient suspected to have COVID-19.
Preoperative preparation
Environmental preparation
The surgery should be performed in a negative pressure operating room with a negative pressure value <–5 Pa. Alternatively, an operating room with independent decontamination units and a relatively independent spatial location should be selected, and the laminar flow decontamination system should be turned off intraoperatively (6). During the epidemic prevention and control period, a general operating room with a relatively independent spatial location and buffer room should be set up as an infected operating room by the department, and used as the special operating room for COVID-19. Before the operation, the items in the operating room should be streamlined, and unnecessary instruments and devices were removed. The personnel in the operating room should not be allowed to enter or leave the operating room at will. Additionally, the door of the operation room should be clearly labeled “COVID-19”.
Personnel arrangement
In the operating room, there should be 3 nurses; that is, 1 hand-washing nurse, and 2 circuit nurses. The 1st circuit nurse is responsible for the circulation of the operating room. The 2nd circuit nurse is responsible for delivering supplies and intraoperative drugs, collecting blood, other outreach work outside the auxiliary buffer area of the operating room, supervising sensory control system to ensure that all staff members are properly dressed, correctly implementing isolation techniques, and maintaining the safety of the operating room environment.
Material preparation
Protective equipment: personal protective equipment (PPE) should be provided in accordance with the tertiary protection standard. The dressing room should be equipped with scrubs, disposable surgical caps, medical protective masks, protective slippers, shoe covers, and quick-drying hand disinfectant. The buffer zone should be equipped with disposable surgical gowns, disposable medical protective gowns, goggles, protective face screens/comprehensive protectors, waterproof boot covers, waterproof shoe covers, medical gloves, surgical sterile gloves, disposable surgical caps, disposable medical surgical masks, quick-drying hand disinfectant, hand-free disinfectant, and stain avoidance paper.
Surgical instruments: all surgical supplies, including instruments and equipment, surgical consumables, indwelling needles, infusion fluids, and drugs, should be prepared based on the type of surgery. Disposable accessories and surgical gowns should be used as much as possible. Any reusable devices should be protected by disposable protective covers, and 2 electric negative pressure suction devices should be present in the operating room.
Pre-treatment room for waste preparation: there should be special bags for medical waste, chlorine disinfectant, a soaking basin for instruments, various cleaning tools, sealing tapes, and pens.
Personal protective measures: participants enter the operating room according to routine requirements
Upon arriving at the dressing room, surgical personnel should (I) disinfect their hands; (II) change their shoes; (III) employ the 7-step hand-washing technique; (IV) change their scrubs; (V) put on a disposable surgical cap; (VI) put on a medical protective mask (for which they check the tightness); (VII) put on goggles; (VIII) wear shoe covers; (IX) disinfect their hands; and (V) enter the buffer zone.
Upon arriving at the buffer zone, personnel under the operating table should: (I) disinfect their hands; (II) put on protective clothing; (III) put on a 1st layer of gloves; (IV) put on impermeable isolation clothing; (V) put on boot covers; (VI) put on shoe covers; (VII) put on a 2nd layer of gloves; (VIII) put on a protective face screen; and (IX) enter the operating room.
Upon entering the buffer zone, surgical staff at the operating table should (I) disinfect their hands; (II) put on protective clothing; (III) put on a protective face screen; (IV) put on boot covers; (V) put on shoe covers; (VI) engage in surgical hand antisepsis; (VII) put on the 1st layer of sterile gloves; (VIII) put on a sterile surgical gown; (IX) put on the 2nd layer of gloves; and (V) enter the operating room. Surgical staff should be dressed in accordance with the tertiary protection standard before entering the operating room.
Coordination of surgical care and prevention and control measures
Children often cry when separated from their families. To reduce cross-infection caused by virus transmission during crying, the circuit nurses should cooperate with the anesthesiologist and adopt the corresponding measures according to the situation.
Pre-anesthesia care
For children who are orally sedated in the ward before surgery and intravenously sedated before anesthesia induction, the circuit nurses must closely observe the child’s breathing, observe the child throughout the whole process, prevent the child from falling out of bed, and transfer the child to the operating room after the child is quiet.
Interoperative anesthesia care
After the child is transferred to the operation bed, the medical staff should connect the child to the monitor, closely observe any changes in vital signs and monitor the child’s body temperature using a disposable temperature probe. If a child is placed under general anesthesia, a respiratory filter should be added between the anesthesia mask and the breathing circuit. After the child loses consciousness, their mouth and nose should be covered with a double layer of wet saline gauze of a size that will not interfere with breathing or fall into the mouth. If the child has no intravenous access, the anesthesiologist should administer inhalation anesthesia, and the circuit nurse should establish intravenous access until the child falls asleep smoothly. After extubation, the child should be kept in the operating room, and should not be transferred to the PACU (5). If the anesthesiologist determines that the child has completely met the criteria for discharge from the PACU, the 2nd circuit nurse and the anesthesiologist should transfer the child to the ward through a special channel using the original transfer vehicle.
Transportation of children
A child who is suspected or confirmed to have COVID-19 should be given oxygen inhalation by nasal catheter with a medical surgical mask, and their entire body should be covered with a disposable impermeable sheet. Due to the inconvenience of wearing a mask, a neonatal incubator should be used for newborns before and after surgery. The medical staff should check oxygen saturation and closely observe the child’s face and breathing during the transfer. The transfer route should comply with the hospital’s regulations. The patient should enter and exit the operating room through special elevators and passages to avoid stopovers. The dress code for transporting personnel is as follows: medical protective masks, protective clothing, goggles or protective face screens, gloves, and shoe covers.
Prevention of surgical complications
Preoperative preparations are tedious, intraoperative operations are slow, and the operating time is relatively prolonged. The exposed time of a child should be reduced as much as possible. Medical staff should adapt a variety of warming measures to prevent intraoperative hypothermia, assess the risk of pressure sores, and strengthen the protection of the pressure site to avoid the occurrence of pressure injuries.
Avoid aerosol generation
The hand-washing nurse should closely follow the surgical steps and monitor the progress of the operation. The surgeon should operate gently, reduce negative pressure suction operations, and use electric negative pressure suction devices whenever possible. In applying electrosurgical equipment, pneumatic drills and electric drills, electrosurgical smoking devices should be used to avoid aerosol generation. Medical staff should minimize the implementation of lumpectomy, as the possibility of aerosol transmission due to pneumoperitoneum pressure leakage during lumpectomy has not been ruled out (7).
Ensuring precise operation
Tertiary PPE reduces the sensitivity of a surgeon’s vision, hearing, and touch, which affects the precision of the operation. Thus, the surgeon should slow down the operation speed. Effective communication between the medical and nursing staff should be enhanced. Each staff member should wear a label stating their identity and name on their PPE clothing to ensure a precise and smooth technical operation.
Prevention of occupational exposure
Sharp instruments should be passed by non-contact delivery during surgery to prevent the occurrence of needle-stick injuries in accordance with the principle of safe injection. A certain distance from the operating table should be maintained during surgery to avoid blood and body-fluid splashing, and protective equipment should be replaced in a timely manner if contamination occurs.
The end-processing of infected surgery
The end-processing of infected surgery should be conducted by the circuit nurses, hand-washing nurse, and the housekeeping staff in the operating room. As per the relevant provisions of the Technical Specification for Disinfection in Medical Institutions (8) and the Management of Waste in Medical Institutions during Pneumonia Epidemic with COVID-19 Infection (9), the treatment of surgical instruments, surgical specimens, operating room tables, floor and air disinfection should be performed according to the process detailed in Figure 2.

Results
A total of 219 surgeries which patients’ COVID-19 nucleic test results are not out were completed during the outbreak. The measures were strictly implemented, and the process of putting on and removing PPE was carefully executed by the medical staff. No medical staff infection or nosocomial infection occurred. No complications, such as hypothermia and stress injury, occurred in the children who underwent surgery despite the relatively long operation time. A tripartite verification system and shift handover system were carefully implemented to increase effective communication between the medical and nursing staff, and no safety incidents occurred.
Discussion
Infection prevention and control measures for children
Medical staff should carefully implement the surgical triage treatment and strictly enforce preoperative screening. In this study, most of the children with COVID-19 infection were asymptomatic or had the main symptoms of fever, a dry cough, and malaise. However, a few patients had upper respiratory symptoms, including nasal congestion and a runny nose, and some children presented with gastrointestinal symptoms, such as abdominal discomfort, nausea, vomiting, abdominal pain, and diarrhea (10). Among the completed surgeries on patients confirmed to have COVID-19, 1 patient presented with gastrointestinal symptoms as the 1st symptom (11).
All patients suspected to have COVID-19 with atypical symptoms and suspected symptoms should be subjected to the tertiary protection to reduce the risk of infection among medical personnel. For those without preoperative nucleic acid test results, the nucleic acid results should be tracked in a timely manner after surgery, and if the results are positive, the results should be reported to the Infectious Disease Department of the hospital in a timely manner, the results should be also actively provided to the same surgical staff for feedback, and the health status of the participants should be followed-up.
Children show poor compliance, so medical staff should strengthen the care and observation. Children often cry when they are separated from their families. To reduce cross-infection caused by virus transmission during crying, the anesthesiologist should sedate the child before surgery, and the circuit nurse should accompany the child throughout the procedure and closely observe the vital signs and any changes in condition. On the basis of routine nursing care, the verification system should be strictly implemented, and effective communication between medical and nursing staff should be increased to ensure the safety of all important parts in the operation.
A management mode without parental accompaniment should be adopted for children in the isolation ward. During the transportation of children, the operating room staff should strictly check the wristband and verify the information with the ward nurses, including the identity information of the child, the mode and site of the operation, the preoperative preparation, and the preoperative medication, and the operating room staff with the ward nurses should leave after verification. A fixed route should be set between the operating room and the ward, and the transportation should pass through a dedicated elevator, and a dedicated transport vehicle should be used.
Personnel training and personnel management
Any staff involved in the surgery of patients suspected or confirmed to have a COVID-19 infection should be required to undergo the standardized training and assessment. The training and assessments include: (I) the nosocomial reporting process for surgery with infected patients; (II) personal protection techniques for medical staff: protection level and the preparation of supplies, the wearing and removal process for protective clothing, the application of positive pressure hood, and disinfection methods; (III) air, surface, and floor disinfection in the operating room and the medical waste disposal process; and (IV) infected child transfer routes and procedures. Training targets include surgeons, anesthesiologists, operating room nurses, and operating room workers. Training methods include the WeChat platform, online learning and on-site training. Assessment methods include a questionnaire (WJX.cn) and an on-site assessment.
Staff members present in the operating room should be subject to temperature testing. The number of personnel participating in surgery should be strictly limited; other personnel should be prevented from entering and leaving the operating room, and visits should be refused. Any unnecessary gathering of staff members should be reduced by the reasonable arrangement of the number of staff at work according to the volume of surgery; the surgical staff should be deployed according to the time and difficulty of surgery to reduce staff handover.
Correct and effective protective measures
When a child is suspected or confirmed to have COVID-19, the child should be treated in accordance with the norms of prevention and control for the operating room. The surgery should be conducted in a special operating room for COVID-19 tertiary protection implemented, and a final disinfection should be performed after the operation and register information. Special attention should be paid to the facial protection items worn in operations with a high risk of infection, such as tracheotomy, airway foreign body removal surgery, aspiration, and other invasive operations (12). Additional tighter measures should be added to the original protection, such as the application of a full-face positive pressure hood. The movements during surgery should be gentle and cautious to avoid the splashing of blood and body fluids and minimize movements that could trigger aerosol generation. Medical personnel attending the operations should wear PPE correctly in accordance with the procedures, and the order of removal should adhere to the principle that “the first item worn should be taken off last” (7). Gentle movements and small operations should be employed during the removal of items.
COVID-19 pneumonia is fierce, and requires a rapid response. The personnel underwent rapid training and corresponding procedures were developed quickly. However, a great deal of content was covered in a brief period, many medical personnel must be present in the operating room, and the compliance of medical staff differs. To ensure the safety of children and medical staff and prevent the spread of the disease, the surgical workflow and management of all important aspects of the operating room should be continuously improved and refined.
Conclusions
As a special group, children are susceptible to COVID-19, and should receive special attention. As the only hospital designated to treat children with COVID-19 in Hubei Province, our hospital effectively implemented the infection prevention and control measures in surgery according to the characteristics of children. These measures ensured the safety of the surgeries and reduced the risk of infection in children and medical staff.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-463/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-463/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-463/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Wuhan Children’s Hospital (No. 2021R055-E01) and informed consent was taken from all patients’ parents or legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus The species and its viruses-a statement of the Coronavirus Study Group. bioRxiv, 2020:2020-2022. DOI:
10.1101/2020.02.07.937862 .10.1101/2020.02.07.937862 - Office of National Health Commission & State Administration of Traditional Chinese Medicine. Diagnosis and Treatment Protocol for Novel Coronavirus Pneumonia (Trial version 6) [EB/OL]. (2020-02-18). Available online: http://www.nhc.gov.cn/yzygj/s7653p/202002/8334a8326dd94d329df351d7da8aefc2.shtml.
- General Office of the National Health Commission. Technical Guidelines for Prevention and Control of Novel Coronavirus Infections in Medical Institutions (First Edition) [EB/OL]. (2020-01-22). Available online: https://www.nhc.gov.cn/yzygj/s7659/202001/b91fdab7c304431eb082d67847d27e14.shtml.
- Sun Y. Surgical management methods for patients with suspected or confirmed novel coronavirus pneumonia. Chinese Journal of Modern Nursing 2020;1016-8.
- Pediatric Anesthesiology Group of Anesthesiology branch of Chinese Medical Association, Youth Committee of Anesthesiology branch of Chinese Medical Association. Norms related to pediatric anesthesia during the epidemic of novel coronavirus pneumonia. Chinese Journal of Anesthesiology 2020;40:281-6.
- Chang H, Bie F, Wang L, et al. Suggestion for Infection Prevention and Control in the Operating Room for Patients with Suspected or Confirmed Coronavirus Disease 2019. Chinese Journal of Clinical Infections Diseases 2020;13:E005.
- Chinese Nursing Association Operating Room Professional Committee. Infection Prevention and Control in the Operating Room for Patients with Suspected or Confirmed Coronavirus Disease 2019: An Expert Consensus.
- National Health Commission. Regulation of Disinfection Technique in Healthcare Settings [EB/OL]. (2012-04-17) Available online: https://www.nhc.gov.cn/wjw/s9496/201204/54510.shtml.
- General Office of the National Health Commission. Waste management in medical institutions during the pneumonia outbreak of novel coronavirus infection [EB/OL]. (2020-01-28). Available online: https://www.nhc.gov.cn/yzygj/s7659/202001/6b7bc23a44624ab2846b127d146be758.shtml.
- Program for the Management of Suspected Exposed Persons and Close Contacts to Corona Virus Disease 2019 Infection (the second edition) [EB/OL]. (2020-01-22). Available online: https://www.nhc.gov.cn/jkj/s3577/202001/c67cfe29ecf1470e8c7fc47d3b751e88.shtml.
- Wang H, Duan X, Yan X, et al. A case of novel coronavirus infection combined with acute appendicitis in a child. Chinese Journal of Pediatric Surgery 2020;41:299-302.
- Sun Y, Hu YJ, Xiao HJ. Suggestions for emergency operation of otorhinolaryngology head and neck during the period of prevention and control of 2019 novel coronavirus. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2020;55:322-5. [PubMed]
(English Language Editor: L. Huleatt)


