
Description of the medical services provided to children in Shanghai: a cross-sectional study of the characteristics and disparities of hospitals of different levels and types
Highlight box
Key findings
• Shanghai provides an overall superior medical service to children in China. The uneven development between the children’s hospitals and the general hospitals represents a major challenge facing Shanghai’s pediatric care system.
What is known and what is new?
• The development of the pediatric care system is uneven in China. The medical referral system has been explored for many years.
• We investigated the characteristics of the medical services provided to children in Shanghai and the disparities among hospitals of different levels and types.
What is the implication, and what should change now?
• The close link between the children’s hospitals, general hospitals, and primary/community hospitals should be strengthened to further optimize the distribution of high-quality resources and greatly improve the overall provision of pediatric medical services.
Introduction
Children are vital to China’s present and its future. Currently, it is estimated that there are 279 million children in China aged younger than 18 years, a figure which accounts for 15% of all children worldwide (1). China has been making great efforts to improve children’s health. Over the past 3 to 4 decades, there has been a significant decrease in the mortality of newborns, infants, and children aged under 5 years in China (2). With the full implementation of the 3-child policy and the increasing demand for high-level and diversified pediatric medical care, the pressures and challenges faced by pediatric medical services are also increasing. Pediatric medical resources in China are lacking, the supply of high-quality pediatric resources is low, and a large gap exists between the supply and demand of pediatric medical services. It has been reported that China has only approximately 4 pediatricians per 10,000 children (3). Further, the average educational level of pediatricians is low; indeed, it has been reported that 1/3 of pediatricians receive only 3 years of junior college training after high school (3).
The development of the pediatric care system is uneven in China (3). Shanghai, which is a well-developed region in China, has high-quality pediatric medical resources. With an area of approximately 6,340 km2, Shanghai has a permanent resident population of >24 million, including >2.4 million children aged 0–14 years (4). In 2017, 2 of 3 National Children’s Medical Centers were established in Shanghai by the National Health Commission. This strategy is conducive to optimizing the regional distribution of high-quality pediatric medical resources, exerting their radiating effect, and thus improving the development of children’s health in China (5).
According to the Shanghai Municipal Health Commission, Shanghai currently has 86 hospitals, including children’s hospitals and general hospitals of different levels, which provide pediatric medical services (Figure S1). In response to the uneven distribution and development of the hospitals providing pediatric care in the city, the Shanghai government launched a city-wide Pediatric Medical Consortium in 2016 and introduced policies dividing the metropolis into 5 clusters (i.e., the Eastern, Western, Southern, Northern, and middle clusters) to reduce the gap and strengthen the link between the children’s hospitals and general hospitals, and among the tertiary hospitals, secondary hospitals, and primary/community hospitals. This strategy was implemented earlier in Shanghai than it was in other regions in China; however, Shanghai is still facing significant prominent problems in improving a number of mechanisms, including the pediatric talent training mechanism, the incentive and competition mechanisms for pediatric medical problems, the 2-way referral mechanism, and the coordination mechanism of medical institution guarantees (e.g., the pediatric service pricing and multisectoral coordination guarantees) (5). The operation mechanisms need to be urgently improved and a close connection between the hospitals in the Pediatric Medical Consortium needs to be urgently strengthened.
We conducted this study to provide the service providers and policy makers with further insights into the field of pediatrics and provide more data to support future policy making. More specifically, we conducted this study to describe the current allocation of pediatric medical resources and the current service system in Shanghai, including its characteristics and challenges, and the current situation since the outbreak of coronavirus disease (COVID-19) in 2020, and to provide a reference to further promote the development of pediatric health care in China and realize the vision of “Healthy China 2030” (6). We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-300/rc).
Methods
Study design
The study was commissioned by the Shanghai Center for Medical Quality Control and conducted by the Children’s Hospital of Fudan University. The city-wide cross-sectional questionnaire covered all 86 hospitals with pediatric qualifications identified by the Shanghai Municipal Health Commission. The overall characteristics of the pediatric medical services in Shanghai in 2020 were described, and the differences between the children’s hospitals and general hospitals were compared. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the ethics committee of the Children’s Hospital of Fudan University (No. 2022-52) and individual consent for this retrospective analysis was waived. All the hospitals included in the study were informed and agreed with the study.
Data collection
Structured questionnaires were developed by a panel of experts from the Center for Pediatric Clinical Quality Control of Shanghai. The questionnaire comprised 14 categories of questions about pediatric care and included open- and close-ended questions. The questions were designed to gather information about the name, address, level and type of hospitals; the pediatricians, pediatric subspecialties, pediatric medical equipment; the outpatient, emergency, and inpatient services, the types of diseases that received inpatient treatment at the hospitals; the advantages of the pediatric services, and suggestions for developments in the field of pediatrics. Examples of the questions in the questionnaire are provided in Appendix 1.
The questionnaire was conducted in November 2021. The principal of the Medical Administration Department of each hospital was required to fill in the questionnaire. The response rate was 90.7% (78/86). The general characteristics of the pediatric healthcare facilities, pediatricians, and pediatric subspecialties were described and compared between the hospitals of different levels and types, and the suggestions to further develop the Pediatrics were discussed. A general hospital, which is one of the main units of the Pediatric Medical Consortium and has significant advantages in provision of pediatric service, was classified as a children’s hospital for the purposes of the analysis.
Pediatricians and hospitals
In China, a pediatrician is defined as a physician certified by the National Health Commission of the People’s Republic of China and authorized to specialize in medical care for children (3). The information gathered on pediatricians included information about their age, gender, educational level, and professional title. Based on the hospital scale, scientific research direction, talent, and technical strength, medical hardware and equipment, the public hospitals in China are mainly divided into the following three levels: tertiary hospitals, secondary hospitals, and primary/community hospitals. According to their specialties, public hospitals are divided into general hospitals and specialized hospitals.
Statistical analysis
The continuous variables are presented as medians with ranges, and the categorical variables are expressed as frequencies. The free-text answers were collected and summarized to the main topics. Comparisons were performed using the chi-squared (χ2) test for the categorical variables. P values <0.05 were considered statistically significant. The statistical analyses were performed using SPSS 20.0 (IBM, NY, USA).
Results
General characteristics of the pediatric medical services provided in Shanghai
Distribution of pediatric healthcare facilities
In 2020, a total of 86 hospitals were providing pediatric medical services in Shanghai. These hospitals covered all 16 municipal districts, and there was a median of 5 hospitals per district (Table 1). In relation to the distribution of the hospitals, on average, there were 1.4 hospitals per 100 km2 and 3.5 hospitals per 1,000 children aged 0–14 years. In relation to the 7 central urban districts with a high population density of children (i.e., >1,000 children aged 0–14 years per km2), the hospitals were densely distributed, with an average of 14.7 hospitals per 100 km2 and 6.2 hospitals per 1,000 children aged 0–14 years. According to data from the 78 responding hospitals, the total number of authorized beds was 5,293, and there was an average of 2.2 beds per 1,000 children aged 0–14 years. The hospitals were mainly public (94.2%) and general (96.5%) hospitals. Of the public hospitals, 53.1% were tertiary hospitals, and the others were secondary hospitals. Four of the tertiary hospitals, including three children’s hospitals and one general hospital specializing in pediatrics, provided comprehensive pediatric subspecialty healthcare. Two of the hospitals were distributed in the central urban area, one in the suburbs, and one in the Pudong New Area.
Table 1
| Districts | Area (km2) | Population aged 0–14 (×104) | Population density aged 0–14 (/km2) | Pediatric healthcare facilities, n | Facilities per 100 km2, n | Facilities per 1,000 children aged 0–14, n | Tertiary hospitals, n (%) | Private hospitals, n | Response to questionnaire, n (%) | Authorized beds# | Beds per 1,000 children aged 0–14#, n | Pediatricians#, n | Pediatricians per 1,000 children aged 0–14#, n | Clusters of Pediatric Medical Association |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Shanghai | 6,340.5 | 243.6 | 384 | 86 | 1.4 | 3.5 | 43 (50.0) | 5 | 78 (90.7) | 5,293 | 2.2 | 2,683 | 1.1 | 5 clusters in all |
| PD* | 1,210.4 | 59.6 | 492 | 15 | 1.2 | 2.5 | 10 (66.7) | 2 | 12 (80.0) | 1,256 | 2.1 | 625 | 1.1 | Eastern |
| HP | 20.5 | 5.7 | 2,780 | 5 | 24.4 | 8.8 | 3 (60.0) | 0 | 5 (100.0) | 74 | 1.3 | 50 | 0.9 | Middle |
| XH | 54.8 | 10.9 | 1,989 | 7 | 12.8 | 6.4 | 3 (42.9) | 2 | 6 (85.7) | 88 | 0.8 | 74 | 0.7 | Southern |
| CN | 38.3 | 6.2 | 1,619 | 1 | 2.6 | 1.6 | 1 (100.0) | 0 | 1 (100.0) | 16 | 0.3 | 20 | 0.3 | Western |
| JA | 36.9 | 9.1 | 2,466 | 6 | 16.3 | 6.6 | 4 (66.7) | 0 | 5 (83.3) | 58 | 0.6 | 62 | 0.7 | Western |
| PT* | 54.8 | 11.6 | 2,117 | 5 | 9.1 | 4.3 | 3 (60.0) | 0 | 5 (100.0) | 1,290 | 11.1 | 525 | 4.5 | Western |
| HK | 23.5 | 6.2 | 2,638 | 7 | 29.8 | 11.3 | 3 (42.9) | 1 | 7 (100.0) | 88 | 1.4 | 82 | 1.3 | Northern |
| YP* | 60.7 | 11.0 | 1,812 | 5 | 8.2 | 4.5 | 3 (60.0) | 0 | 4 (80.0) | 719 | 6.5 | 251 | 2.3 | Northern |
| MH* | 370.8 | 28.8 | 777 | 5 | 1.3 | 1.7 | 4 (90.0) | 0 | 5 (100.0) | 677 | 2.4 | 648 | 2.3 | Southern |
| BS | 271.0 | 22.4 | 827 | 8 | 3.0 | 3.6 | 3 (37.5) | 0 | 7 (87.5) | 554 | 2.5 | 93 | 0.4 | Northern |
| JD | 464.2 | 18.0 | 388 | 5 | 1.1 | 2.8 | 1 (20.0) | 0 | 4 (80.0) | 70 | 0.4 | 60 | 0.3 | Western |
| JS | 586.1 | 7.6 | 130 | 4 | 0.7 | 5.3 | 1 (25.0) | 0 | 4 (100.0) | 102 | 1.3 | 44 | 0.6 | Southern |
| SJ | 605.6 | 20.5 | 339 | 4 | 0.7 | 2.0 | 1 (25.0) | 0 | 4 (100.0) | 96 | 0.5 | 50 | 0.2 | Southern |
| QP | 670.1 | 11.3 | 169 | 3 | 0.4 | 2.7 | 1 (33.3) | 0 | 3 (100.0) | 44 | 0.4 | 30 | 0.3 | Southern |
| FX | 687.4 | 10.6 | 154 | 3 | 0.4 | 2.8 | 1 (33.3) | 0 | 3 (100.0) | 59 | 0.6 | 42 | 0.4 | Eastern |
| CM | 1,185.5 | 4.3 | 36 | 3 | 0.3 | 7.0 | 1 (33.3) | 0 | 3 (100.0) | 102 | 2.4 | 27 | 0.6 | Northern |
*, districts in which children’s hospitals are located; #, data of the 78 responding hospitals, the data of pediatricians who were retired or retired but re-employed were not included. PD, Pudong New Area; HP, Huangpu District; XH, Xuhui District; CN; Changning District; JA, Jinan District; PT, Putuo District; HK, Hongkou District; YP, Yangpu District; MH, Minhang District; BS, Baoshan District; JD, Jiading District; JS, Jinshan District; SJ, Songjiang District; QP, Qingpu District; FX, Fengxian District; CM, Chongming District.
Characteristics of the pediatricians
According to the complete questionnaire data obtained from 78 hospitals, there were 2,683 pediatricians in Shanghai (Table 1). On average, the distribution of pediatricians was 42.3 pediatricians per 100 km2 and 1.1 pediatricians per 1,000 children aged 0–14 years. The pediatricians were mainly women (71.8%) and were mainly aged 40 years or younger (60.6%). In relation to their educational level, the vast majority (99.5%) of the pediatricians held a bachelor’s degree or higher, while 1,804 (67.2%) held a postgraduate degree. Residents, attending physicians, and senior/associate senior physicians accounted for 26.8%, 45.3%, and 27.9% of all pediatricians, respectively.
Workloads of pediatricians
In 2020, the total number of outpatient and emergency pediatric visits recorded in the city was approximately 8 million, with an average of 2,973 individual visits per pediatrician. The total number of pediatric inpatients exceeded 160,000, with an average hospital stay length of 5.9 days.
Pediatric subspecialties
At least 32 pediatric subspecialties were identified in the hospitals in Shanghai, covering all pediatric disciplines, including newborn, child healthcare, pediatrics, pediatric surgery, and traditional Chinese medicine.
Fever clinics
During the COVID-19 pandemic, pediatric fever clinics were also established in Shanghai. According to the data from the 45 hospitals that separately counted the number of fever outpatient visits, the number of visits exceeded 371,000 in 2020. Among the 78 hospitals for which data were collected, 52 (66.7%) had fever clinics open for 24 hours, 45 (57.7%) had independent areas for pediatric fever outpatient visits, and 43 (55.1%) had observation rooms for pediatric fever outpatient visits.
Disparities in the pediatric medical services between the children’s hospitals and general hospitals
Disparities in the distribution of pediatricians
Most pediatricians in Shanghai (66.1%) worked in the 4 children’s hospitals (Table 2). In these hospitals, there were more male than female pediatricians (31.8% vs. 21.3%, respectively; P<0.001), and more young doctors (i.e., those aged below 30 years) (20.3% vs. 12.1%, P<0.001). Most pediatricians were postgraduates and held a master’s degree or doctoral degree (79.5% vs. 43.3%, respectively; P<0.001), and the proportions of both senior/associate senior physicians and residents in the children’s hospitals were higher than those in the general hospitals (P<0.001). However, in terms of the individual outpatient and emergency visits, the situations of the pediatricians in the two types of hospitals were similar, and there were 2,891 and 3,132 visits per pediatrician, respectively.
Table 2
| Variables | Children’s hospitals (n=4) | General hospitals (n=74) | P value |
|---|---|---|---|
| Pediatrician, n (%) | 1,773 (66.1) | 910 (33.9) | |
| Average visits per pediatrician, n | 2,891 | 3,132 | |
| Gender, n (%) | <0.001 | ||
| Male | 563 (31.8) | 194 (21.3) | |
| Female | 1,210 (68.2) | 716 (78.7) | |
| Age, years, n (%) | <0.001 | ||
| <30 | 360 (20.3) | 110 (12.1) | |
| 30–40 | 837 (47.2) | 319 (35.1) | |
| >40 | 576 (32.5) | 481 (52.8) | |
| Title, n (%) | <0.001 | ||
| Senior/associate senior physician | 514 (29.0) | 235 (25.8) | |
| Attending physician | 741 (41.8) | 474 (52.1) | |
| Resident | 518 (29.2) | 201 (22.1) | |
| Educational level, n (%) | <0.001 | ||
| Doctoral degree | 544 (30.7) | 61 (6.7) | |
| Master’s degree | 866 (48.8) | 333 (36.6) | |
| Bachelor’s degree | 363 (20.5) | 503 (55.3) | |
| Other | 0 (0) | 13 (1.4) |
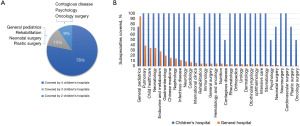
Differences in terms of pediatric subspecialties and medical equipment
In the 4 children’s hospitals, a median of 30 (range: 28–32) subspecialties was covered. Conversely, in the general hospitals, a median of only 2 (range: 1–30) subspecialties was covered. Among the 32 subspecialties, the same 25 subspecialties were provided by the 4 children’s hospitals (Figure 1A). However, none of the same subspecialty was provided by all the 74 hospitals. Indeed, even the most common subspecialty (i.e., general pediatrics) was not covered by all of the 74 general hospitals. In the general hospitals, the most common subspecialty was general pediatrics. However, other subspecialties, such as pulmonary, child health care, and neonatology subspecialties, were less common, only with a coverage of less than 40% (Figure 1B). Notably, 21 general hospitals only had 1 pediatric subspeciality of general pediatrics. In 2 of the general hospitals, pediatric subspecialties, such as ophthalmology, otorhinolaryngology, and dermatology subspecialties, were held concurrently by physicians who also treated adults. Interestingly, a few general hospitals that had no endocrinology and metabolism, pulmonary, neurology, or child health care subspecialties, had established clinics for special diseases, such as clinics for growth and development, clinics for asthma, and clinics for attention deficit hyperactivity disorder.
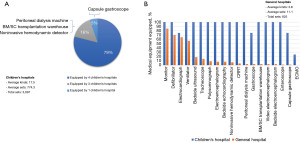
Based on the different subspecialty settings, significant differences in the configuration of pediatric proprietary equipment between the two types of hospitals were observed. The 4 children’s hospitals had many more types and sets of equipment than the general hospitals (Figure 2A,2B). In the general hospitals, the pediatric departments were mainly equipped with basic vital sign monitoring and life support equipment, such as monitors, defibrillators, electrocardiographs, and ventilators (Figure 2B).
Variance in outpatient, fever clinics, emergency, and inpatient services
The total number of pediatric outpatient and emergency visits at the 4 children’s hospitals accounted for 64.3% of the total number of pediatric visits in the city, which was 1.8 times that of the 74 general hospitals (Table 3). The total number of emergency critical illness rescues by the 4 children’s hospitals accounted for 81.2% of the total number of critical illness rescues, which was 4.3 times that of the general hospitals. All of the children’s hospitals had pediatric fever clinics that were open 24 hours and had independent areas for fever clinics. Most of the general hospitals had pediatric fever clinics, among which 80.0% were open 24 hours, and 68.3% had independent areas. The median number of rooms for fever clinics and fever outpatient observation was 5 and 10 times that of the general hospitals, respectively. The total number of pediatric inpatient visits at the 4 children’s hospitals accounted for 84.9% of the total number of pediatric inpatient visits in the city, which was 5.6 times that of the general hospitals.
Table 3
| Variables | Children’s hospitals (n=4) | General hospitals (n=74) |
|---|---|---|
| Outpatient and emergency visits, total | 5,125,992 | 2,850,256 |
| Outpatient and emergency visits, per pediatrician | 2,891 | 3,132 |
| Emergency critical illness rescue patients | 10,936 | 2,530 |
| Hospitals with fever clinics, n (%) | 4 (100.0) | 60 (81.1) |
| Open 24 hours, n (%) | 4 (100.0) | 48 (64.9) |
| With independent areas for fever clinics, n (%) | 4 (100.0) | 41 (55.4) |
| Rooms for fever clinics, median [range] | 5 [2–10] | 1 [0–1] |
| Rooms for fever outpatient observation, median [range] | 10 [0–11] | 1 [0–24] |
| Inpatient visits | 140,864 | 24,978 |
| Average length of hospital stays, day | 6.3 | 5.9* |
*, data from 51 general hospitals with inpatient visits.
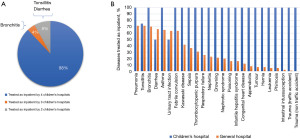
We compared the diseases that received inpatient treatments at the hospitals, and found that among the 25 diseases investigated, only 1 general hospital had treated ≥20 diseases, and 32 general hospitals had treated 10–19 diseases, of which 23 were tertiary hospitals. Notably, 21 general hospitals, of which 7 were tertiary hospitals, had no pediatric hospitalized patients. According to the questionnaire data, 88.0% of the investigated diseases received inpatient treatments in the 4 children’s hospitals (Figure 3A). Pneumonia, bronchitis, tonsillitis, asthma, diarrhea, urinary tract infection, and febrile convulsion were the most common diseases that received inpatient treatments at the general hospitals (Figure 3B). At the general hospitals, the main pediatric services provided were for asthma (32.4%) and growth and development (25.7%).
Suggestions for further developing pediatric medical services
In total, 62 (83.8%) principals of the Medical Administration Department of the general hospitals responded to the questions about the income of pediatricians, of whom 31 (50%) replied that the income of the pediatricians did not reach the average level income of that of other types of doctors at the general hospitals. Half (51.4%) of the principals of the Medical Administration Department of the general hospitals responded by providing advice or suggestions about developments in the field of pediatrics and called for greater support, increasing the income of pediatricians, and strengthening the construction of the pediatric talent echelons. The general hospitals providing pediatric care also hoped to link with the children’s hospitals to increase the talent training and learning opportunities and to improve the treatment level of common and chronic diseases in children to reflect the value of grass-roots pediatrics. Further, the results revealed that 1 of the children’s hospitals intended to strengthen multidisciplinary cooperation, establish more patient-oriented interdisciplinary approaches, deepen the combination of production, research and medicine, and jointly explore new fields and technologies for the precise diagnosis and management of difficult and severe diseases in children.
Discussion
China is facing challenges in the current pediatric care system, including those related to the uneven development of the system, the lack of appropriately trained pediatricians, and the unmet demand for pediatric care (3). Shanghai is a well-developed region in China with relatively concentrated medical resources. This study conducted the first city-wide questionnaire on medical services for children in Shanghai. Specifically, this study explored the characteristics of pediatric medical services in Shanghai in 2020 during the COVID-19 pandemic, compared the disparities between the children’s hospitals and general hospitals in terms of pediatricians, the establishment of pediatric subspecialties, the configuration of pediatric equipment, pediatric outpatient visits, and emergency and inpatient services, and collected suggestions on pediatric development to provide important data to support further improvements in medical services for children in China.
In China, the medical services available to children in Shanghai are relatively superior to other areas in China. The numbers of hospitals providing pediatric care (3.5) and the number of pediatricians (1.1) per 1,000 children aged 0–14 years in Shanghai are approximately 5.9 (0.59) and 4.8 times (0.23) the national average, respectively (3). The number of pediatricians per 1000 children aged 0–14 years in Shanghai is similar to that in Japan (0.93) (7) and approximately half that in the United States (1.9) (8). Nationally, only 1/3 of pediatricians hold a bachelor’s degree or higher. Conversely, almost all of the pediatricians (99.5%) in Shanghai held a bachelor’s degree or higher, among whom, 2/3 held a postgraduate degree.
The pediatric subspecialties are very well established in Shanghai. To prevent and control the spread of COVID-19, 24-hour fever clinics and fever outpatient observation rooms have been widely established in Shanghai. In 2020, only 2/3 of the hospitals had 24-hour fever clinics and fever outpatient observation rooms; however, as of February 2022, all of the hospitals had 24-hour fever clinics and fever outpatient observation rooms. It should be noted that there are relatively few male pediatricians in the city (28%), and the proportion of male pediatricians in Shanghai is far less than that in the United States (46%) (9). In addition, compared to those for the adult population, healthcare resources for children are still in short supply. According to statistics for 2020, the number of physicians per 1,000 adults in Shanghai was 3.3 (10), which is 3 times the number of pediatricians for children aged 0 to14 years (1.1). Thus, the pediatric care system in Shanghai needs to further increase the recruitment of pediatricians.
In Shanghai, children’s hospitals have more medical resources than general hospitals. Two-thirds of the pediatricians in the city work in children’s hospitals; however, this figure differs to that reported in a national questionnaire of 7% (3). Notably, more male pediatricians work in the children’s hospitals than the general hospitals (31.8% vs. 21.3%). There are fewer young pediatricians at the general hospitals than the children’s hospitals, which might be related to the difficulty in recruiting and retaining young pediatricians. The median number of pediatric subspecialties at children’s hospitals (29.5) was 14 times that at general hospitals (2.0). Half of the general hospitals were tertiary hospitals; however, most of them had established a general pediatric subspecialty, with only a few of them establishing subspecialties for common diseases in children, such as pulmonary, child health care, and neonatology subspecialities. Moreover, the pediatric departments at the general hospitals had less pediatric equipment and were mainly equipped with basic vital sign monitoring and life support equipment but lacked equipment for special care. Thus, outpatient, emergency and inpatient visits and the types of diseases treated at the children’s hospitals were more complicated than those treated at the pediatric departments of the general hospitals.
Most of the pediatricians in the general hospitals specialized in pediatric internal medicine and undertake the diagnosis and treatment of common internal diseases. They are unable to deal with the other common medical problems of children in the community, such as mild trauma, burn, bone and joint dislocation, and some psychological problems. The payment for pediatricians in half of the general hospitals was low and did not reach the average income level of other employees in the hospital, and as a result, the pediatricians in the general hospitals were relatively “older”, and the sustainable development of the pediatric talent echelon was obviously hindered. Moreover, it is mainly the children’s hospitals that provide the medical care to children in Shanghai, and the professional orientation of the pediatric departments in general hospitals is not sufficiently clear, and the development of pediatric care in primary/community hospitals is weak. With the threat of children’s health problems changing from acute infectious diseases to chronic diseases, mental diseases, and developmental disorders, children’s healthcare needs are becoming more related to disease prevention and health promotion (11). Thus, it is necessary to carefully explore the development of pediatric medical services given this new situation.
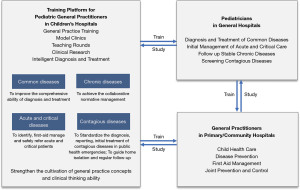
Given the overall shortage of pediatric medical resources, the coordinated development of children’s hospitals and general hospitals and the strengthening and deepening of an integrated development model for pediatric medical care are necessary to further improve the scientific use of pediatric resources and provide better high-quality and convenient medical services for children. Since the introduction of the concept of general practice in the 1980s, China has been promoting the development of general practice, but the development of community pediatrics lags behind (12). General practitioners in the primary/community hospitals have received some education and training related to pediatrics; however, their ability to provide pediatric medical care is weak (13). Thus, there is an urgent need to create a new training path for both pediatrics in the general hospitals and general practitioners in the primary/community hospitals. In our view, similar to the development of adult general practice departments in the general hospitals (14), the establishment of pediatric general practice departments in tertiary children’s hospitals may provide a talent training platform for pediatric general practitioners and promote the integration and exchange of pediatric talent training among children’s hospitals, general hospitals, and primary/community hospitals. This may also be an effective way to strengthen the development of the Pediatric Medical Consortium. By linking the children’s hospitals, general hospitals, and primary/community hospitals, the establishment of training programs for pediatric general practitioners in children’s hospitals will help to cultivate pediatric general practice concepts, promote the training of pediatric general practitioners, become a bridge for better referrals among children’s hospital, general hospitals, and primary/community hospitals, and thus better promote the health of all children (Figure 4).
The limitations of this study need to be considered. First, maternal and child care hospitals were not included in this study; thus, the medical services provided to children in Shanghai may have been underestimated to some extent. Second, this was a retrospective study, which may have resulted in recall bias. However, much information was originated from the hospital information systems, and this should have reduced the possibility of recall bias. Third, the non-response of principals of the Medical Administration Department of the 8 hospitals may limit the generalizability of the questionnaire. The questionnaires were completed by the principals of the Medical Administration Department of each surveyed hospital. The objective questions should be quite representative based on the hospital statistics; however, some subjective questions may not represent the views and ideas of every pediatrician.
Conclusions
The provision of pediatric medical services is better in Shanghai than it is nationally. However, a number of problems still exist, including an insufficient number of pediatricians and an unbalanced distribution of medical resources. Exploring the 2-way integration of general practice construction in children’s hospitals and the development of pediatric subspecialties in general hospitals and strengthening the links among children’s hospitals, general hospitals, and community hospitals may help to predict pediatric practice patterns and thus further enhance the value of pediatric services.
Acknowledgments
Funding: The study was funded by National Key Research and Development Program of China (No. 2021ZD0113501) and Science and Technology Commission of Shanghai Municipality (No. 21511104502).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-300/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-300/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-300/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study protocol was approved by the ethics committee of the Children’s Hospital of Fudan University (No. 2022-52) and individual consent for this retrospective analysis was waived. All the hospitals included in the study were informed and agreed with the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- National Bureau of Statistics of China. What census data can tell us about children in China. 2013. Available online: https://www.unicef.cn/media/7596/file (Accessed June 10, 2022).
- National Bureau of Statistics of China. China Statistical Yearbook 2021. Available online: http://www.stats.gov.cn/tjsj/ndsj/2021/indexch.htm (Accessed June 10, 2022).
- Zhang Y, Huang L, Zhou X, et al. Characteristics and Workload of Pediatricians in China. Pediatrics 2019;144:e20183532. [Crossref] [PubMed]
- Bureau of Statistics of Shanghai. Available online: https://tjj.sh.gov.cn/tjnj/2020rktjnj/ANJ-3-01.jpg (Accessed in June 10, 2022).
- Fang L, Wu L. Analysis on development situation of pediatric medical service and pediatric medical alliance in Shanghai. Soft Science of Health 2020;34:37-41.
- The State Council of the Communist Party of China. The Central Committee of the Communist Party of China issued the outline for the Healthy China 2030 Plan [in Chinese]. Available online: http://www.gov.cn/zhengce/2016-10/25/content_5124174.htm (Accessed June 10, 2022).
- Sakai R, Wang W, Yamaguchi N, et al. The impact of Japan’s 2004 postgraduate training program on intra-prefectural distribution of pediatricians in Japan. PLoS One 2013;8:e77045. [Crossref] [PubMed]
- Goldstein MR. Availability of neonatal intensive care and neonatal mortality. N Engl J Med 2002;347:1893-5; author reply 1893-5. [Crossref] [PubMed]
- Saboor S, Naveed S, Chaudhary AM, et al. Gender and Racial Profile of the Academic Pediatric Faculty Workforce in the United States. Cureus 2022;14:e22518. [Crossref] [PubMed]
- Bureau of Statistics of Shanghai. Available online: http://tjj.sh.gov.cn/tjnj/nj21.htm?d1=2021tjnj/ZBHTML/C0050.htm (Accessed in June 10, 2022).
- Palfrey JS, Tonniges TF, Green M, et al. Introduction: Addressing the millennial morbidity--the context of community pediatrics. Pediatrics 2005;115:1121-3. [Crossref] [PubMed]
- Chen C, Peng Q, Shi J, et al. Developing community pediatrics in China: Necessity, Feasibility, and Recommendations derived from the US training system for community pediatricians. Chinese General Practice 2021;24:2472-6.
- Yao M, Qi J, Chi C, et al. Research of general practitioners’ reception of children and related training in community health service centers in Beijing. Chinese General Practice 2016;19:313-6.
- Song S, Zhang Q, Tan W, et al. Analysis on the significance and current situation of establishing general practice department in general hospitals. Chongqing Medicine 2021;50:2143-5.
(English Language Editor: L. Huleatt)


