Primary extrapulmonary multidrug-resistant tuberculosis in an immunocompetent child presenting with pleural effusion
Introduction
The resource-strained countries are facing a number of public health issues (1). The situation is really grave due to prevalence of infectious diseases like tuberculosis (TB) (1). India is a high TB burden country with a large number of TB cases and a very high number of deaths due to TB (1). The extent of TB in the pediatric age group is really alarming due to the absence of clear signs and symptoms and often late presentations (2). Moreover the ever rising cases of drug resistant TB (DR-TB) in pediatric age groups is even more startling as it requires a greater degree of suspicion to identify such cases (2). Besides, the need to start prompt treatment and the issues related to patient compliance, adverse drug reactions and high pill burden are some of the negative aspects of the pediatric TB cure (2). We herein present a case of primary extrapulmonary multidrug-resistant TB with left pleural effusion in an HIV negative girl. So far, to the best knowledge of the authors no such case has been reported in the scientific literature.
Case presentation
An 11-year-old Indian girl brought to our OPD by her parents with complaints of fever, breathlessness, cough with expectoration, pain on the left side of the chest and weight loss since one and a half month. The fever was evening rise and was not associated with chills and rigors. The cough was non blood tinged and was associated with greenish colored scanty expectoration. She also complained of difficulty in breathing on walking, running and on climbing stairs which was relieved on taking a rest and was exaggerated on lying supine. There was chest pain on the left side of the chest, which was persistent since last 1 month and was increased since last 7 days. She also had generalized weakness and weight loss of about 7 kilograms in last 2 months. Besides, she also complained of loss of appetite for 2 to 3 months. There was no history of trauma to the chest and past history and family history was non-contributory.
On examination, she was thinly built, afebrile and all other vital signs were normal. Physical examination revealed no abnormal findings. On systemic examination the dull note was found on the left hemi thorax and vocal repercussion were decreased, auscultation reveled decreased breath sounds on the left hemi thorax. There were no signs of lower extremity deep-venous thrombosis and no palpable lymph nodes. The rest of the systemic examination was within the normal limits.
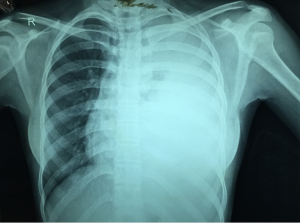
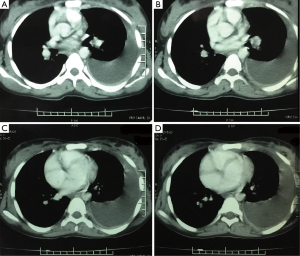
Routine laboratory work-up showed an elevated leukocyte count (12,000/mm3), erythrocyte sedimentation rate (45 mm in the first hour), and C-reactive protein (7 mg/L). Human immunodeficiency virus and viral hepatitis antigens/antibodies/DNA were not detectable in serum. Arterial blood gases showed mild hypoxemia (PO2 =89 mmHg on room air). Rest all other blood investigations were within the reference range. The acid-fast bacilli (AFB) smear of two sputum samples was negative under fluorescent microscopy. The chest radiograph (P-A view) (Figure 1) revealed a massive left sided pleural effusion with shifting of the mediastinum and trachea towards the contralateral side. The findings were confirmed on the CECT chest (Figure 2), which revealed a homogenous, non-loculated moderate to gross amount of fluid in the left pleural cavity with underlying passive lung atelectasis and extension of fluid into the lung fissure. A diagnostic thoracocentesis was performed which revealed a straw colored exudative fluid (protein 5.2 g/dL, glucose 34 mg/dL, cholesterol level 55 mg/dL, complete cell count 680/µL with 10% neutrophils and 90% lymphocytes). Pleural fluid Gram stain, AFB smears and cytology were all negative. Pleural fluid adenosine deaminase (ADA) level was 80 IU/L and lactic acid dehydrogenase (LDH) 1,837 U/L. PPD skin test (0.1 mL of PPD-RT 23, 2 TU) was strongly positive (16 mm × 18 mm induration). Thus a diagnosis of primary extrapulmonary left sided tuberculous pleural effusion was made and the patient was started on the Revised National TB Control Programmes’s Category-I antitubercular therapy (ATT) involving isoniazid (H) and rifampicin (R), pyrazinamide (Z) and ethambutol (E) based on her weight. However, considering the amount of pleural effusion, condition of the patient, no family history of TB, and high endemicity of TB in India one sample of pleural fluid was sent to the National Reference Laboratory for culture and sensitivity of Mycobacterium TB under enhanced case finding for multidrug-resistant TB (MDR-TB).
Sample grew M. TB on Lowenstein Jensen medium after 8 weeks of incubation. In line probe assay GenoType® MTBDRplus (Hain Lifescience GmbH, Nehren, Germany), the isolate, was identified as M. TB and found to be resistant to isoniazid (H) and rifampicin (R), but was sensitive to other first line drugs, that is, pyrazinamide (Z) and ethambutol (E) by Bactec Mycobacteria Growth Indicator Tube (MGIT) 960 system.
Thus, a diagnosis of primary extrapulmonary multidrug-resistant TB presenting as left sided pleural effusion was made. And her Category-I ATT was modified to Category-IV ATT after admission and initial monitoring at the state DR-TB center, involving the use of 2nd line ATT as per her weight with kanamycin, levofloxacin, cycloserine, ehionamide, PAS powder, ethambutol, and pyrazinamide. Besides, one more sample was sent for 2nd line drug sensitivity testing (DST) which showed sensitivity to all the 2nd line drugs. The patient is currently on treatment and is regularly followed-up. So far she has not complained of any adverse drug reactions due to the Category-IV drugs.
Discussion
The low income countries like India are fighting very hard against the problem of infectious diseases like TB (1). TB affects all age groups and is one of the most common causes of death in 15–45-year age group (1). TB mainly affects the lungs, but the cases of extrapulmonary TB are also on the rise (3,4). The DR-TB came into limelight since the year 1990 when it became a major public health problem (4). The MDR-TB develops due to spontaneous mutations in the genes of the bacilli and it requires a really higher load of bacteria for the development of primary MDR-TB (5). Again the MDR-TB is basically a man-made problem, and is an outcome of improper or poorly administered treatment (4). The WHO in the year 2013 reported that the prevalence of primary MDR-TB in India is around 3.5%; however, this prevalence is 20.5% among previously treated cases (4). Thus the case of primary MDR-TB with only extrapulmonary involvement is a very rare form of the disease, even in the immunocompromised patients, and it requires a great deal of suspicion to diagnose such a case especially in young children (2,5). Moreover, there is a paucity of information about primary extrapulmonary MDR-TB in all age groups in the medical literature (4).
In the past primary DR-TB has been reported in the isolated cases and studies, but the same in pediatric age group with the involvement of pleura alone has not been reported (4-12). Hence we have presented the very first pediatric case of primary MDR-TB presenting as pleural effusion. Our case also differs from the case presented by Das et al. 2012, in the absence of the dissemination to any other organ and also the present case is a pediatric case (5). Besides, a study carried in the South Africa showed the presence of MDR-TB in pediatric age groups, but this study mainly involved the HIV positive cases of TB meningitis and in almost all these cases the diagnosis was made posthumously (13). Our case differs from this South African study due to the involvement of the different extrapulmonary site, i.e., pleura, with early diagnosis based on the high degree of suspicion and the HIV negative status of the case (13).
Conclusions
With the growing numbers of TB cases, especially in endemic countries a greater degree of suspicion is required to diagnose the primary MDR-TB cases and due heed should be given to the primary extrapulmonary cases. The prompt diagnosis and treatment is warranted in all the MDR-TB cases. The present case will broaden our understanding of these rare presentations of a common disease and will also serve as a tool for early diagnosis and management of primary extrapulmonary MDR-TB in the pediatric age group in the future. The role of dissemination of healthcare information to all the sections of the society about the MDR-TB and its management is essential and should be given prime importance. Furthermore, large studies related to finding the cause, early detection and possible preventive measures from the MDR-TB is warranted.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the legal guardians of the patient for publication of this case report and the accompanying images.
References
- Yadav S. A new concept in tuberculosis awareness in the low income countries. Edorium J Tuberc 2015;1:1-4.
- Piccini P, Chiappini E, Tortoli E, et al. Clinical peculiarities of tuberculosis. BMC Infect Dis 2014;14 Suppl 1:S4. [Crossref] [PubMed]
- Yadav S, Rawal G. Tubercular nodular episcleritis: a case report. J Clin Diagn Res 2015;9:ND01-2. [PubMed]
- Yadav S, Rawal G. Primary extrapulmonary multidrug-resistant tuberculosis of the sternum without HIV infection. J Clin Diagn Res 2016;10:RD01-3. [PubMed]
- Das SK, Das A, Gangopadhyay A, et al. Primary disseminated extrapulmonary multidrug resistant tuberculosis. Indian J Med Microbiol 2012;30:364-6. [Crossref] [PubMed]
- Rawat J, Sindhwani G, Dua R. Primary multi-drug resistant tubercular lymphadenitis in an HIV infected patient. Indian J Tuberc 2009;56:157-9. [PubMed]
- Asgeirsson H, Blöndal K, Blöndal T, et al. Multidrug resistant tuberculosis in Iceland--case series and review of the literature. Laeknabladid 2009;95:499-507. [PubMed]
- Sofia M, Maniscalco M, Honoré N, et al. Familial outbreak of disseminated multidrug-resistant tuberculosis and meningitis. Int J Tuberc Lung Dis 2001;5:551-8. [PubMed]
- DeVincenzo JP, Berning SE, Peloquin CA, et al. Multidrug-resistant tuberculosis meningitis: clinical problems and concentrations of second-line antituberculous medications. Ann Pharmacother 1999;33:1184-8. [Crossref] [PubMed]
- Sarkar S, Maity GN, Mukhopadhyay KK, et al. Primary multidrug resistant tuberculosis. Lung India 2007;24:97-9.
- Krishnan H, Chan KL. Multidrug resistant tuberculosis involving the clavicle, spine and ribs. Malays Orthop J 2011;5:71-4. [Crossref]
- Pawar UM, Kundnani V, Agashe V, et al. Multidrug-resistant tuberculosis of the spine--is it the beginning of the end? A study of twenty-five culture proven multidrug-resistant tuberculosis spine patients. Spine (Phila Pa 1976) 2009;34:E806-10. [Crossref] [PubMed]
- Padayatchi N, Bamber S, Dawood H, et al. Multidrug-resistant tuberculous meningitis in children in Durban, South Africa. Pediatr Infect Dis J 2006;25:147-50. [Crossref] [PubMed]