
Neutrophil-to-lymphocyte ratio as a predictor of surgical site infection in acute appendicitis
Highlight box
Key findings
• Neutrophil-to-lymphocyte ratio (NLR) has a stronger capacity to predict the development of Surgical Site Infections (SSI) than clinical, ultrasound and surgical data in children with Acute Appendicitis (AA).
• NLR has higher sensitivity and specificity than other acute-phase reactants such as leukocytes, neutrophils and CRP.
What is known and what is new?
• NLR has been reported as an inflammatory marker in different abdominal inflammatory pathologies.
• This study is the first to determine the role of NLR as a predictor of SSI in children with AA.
• NLR value at admission is the most promising predictive factor for the development of SSI in children undergoing appendectomy.
• It is an easy, simple, inexpensive, and rapid method to detect these patients.
What is the implication, and what should change now?
• Patients with high preoperative NLR are at high risk of developing SSI.
• This may facilitate its early diagnosis and treatment.
Introduction
Acute appendicitis (AA) is the most frequent surgical emergency in both adults and children (1), and like any surgical procedures, it can also be associated with different postoperative complications, such as surgical site infections (SSIs), persistent ileus or intraabdominal abscess (2). SSI is one of the most common complications, taking place in 2–5% of children who undergo inpatient surgical procedures (3,4). It has also been associated with an increased postoperative morbidity, which is a substantial additional healthcare cost, making this complication a concern for all surgical teams (5,6). Therefore, it is essential to determine SSI predictive factors in order to prevent its occurrence. A positive association has been described between some factors and the development of SSI, such as time of symptoms onset (7), ultrasound appendix diameter (8) or surgery time (9), so that increasing any of these factors also increases the risk of SSI. However, these factors all have in common a high inter-individual variability, as they greatly depend on the subjective assessment of the patient or the physician (radiologist or surgeon). In contrast, no objective parameters, such as inflammatory biomarkers easily detectable in laboratory tests, have been analysed to date in order to quantify the risk of developing postoperative SSI.
Recently, neutrophil-to-lymphocyte ratio (NLR) has been reported as an inflammatory marker in different abdominal inflammatory pathologies such as acute appendicitis (10,11). In children, NLR has recently been shown to predict the risk of peritonitis in patients with AA (12), and it is also useful for predicting the risk of developing intra-abdominal abscesses after appendectomy (13), However, the relationship of NLR and the subsequent development of SSI has not been described to date. The aim of this study is to evaluate the role of admission NLR as a predictor of SSI in children who underwent surgery for acute appendicitis. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-360/rc).
Methods
A single-center, retrospective cohort study was performed in patients with acute appendicitis, who underwent surgical treatment in our center between January 2017 and December 2020. We included all patients between 5 and 16 years with an intraoperative diagnosis of AA, who were divided into two groups depending on the development of surgical site infection during the first 30 postoperative days (SSI group and control group). Patients under 5 years were excluded due to the important physiological differences in white blood cell count up to that age (14). Other exclusion criteria were incomplete laboratory tests at admission, the absence of histological data of acute appendicitis after anatomopathological study of the appendix and patients with postoperative intra-abdominal abscess, in order to avoid possible biases.
Demographic data (gender and age), time since symptoms onset, laboratory tests at admission, appendiceal diameter measured by ultrasound, type of acute appendicitis (complicated/uncomplicated), type of appendectomy performed (open/laparoscopic), surgery time and surgical wound infections in first 30 postoperative days were analyzed. Laboratory variables were obtained from blood tests performed in the Emergency Department at the patient’s admission, which included absolute values of leukocytes, neutrophils, lymphocytes, platelets, fibrinogen, and C-reactive protein (CRP). NLR was calculated by dividing the absolute neutrophil count and the absolute lymphocyte count. Complicated appendicitis were considered as those in which perforation or purulent intra-abdominal fluid was evidenced during surgery. Surgical site infection was defined according to the U.S. Centers for Disease Control and Prevention’s criteria (15). For this study only SSIs with extra-abdominal location were considered: superficial (affecting subcutaneous cellular tissue) or deep (affecting fascia/muscle). Organ space SSIs, which involve structures deeper than fascia/muscle (intra-abdominal location) were considered as intra-abdominal abscess, and were therefore not included in this study. In our center, we perform surgical treatment of all AA, with preoperative antibiotic therapy with Amoxicillin-Clavulanic acid. Post-operative antibiotic is only continued in gangrenous appendicitis (Amoxicillin-clavulanic acid for 5 days), and in appendicitis with peritonitis (Gentamicin, Metronidazole and Amoxicillin-Clavulanic acid for 7 days). Follow-up was performed during hospitalisation in order to detect surgical site infection in the first postoperative days. Outpatient clinic follow-up was performed at 2 weeks and 30 days postoperatively to assess the surgical wound aspect. If no complications were observed, patients were discharged and follow-up was completed one month after surgery.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by institutional review board of La Paz Children’s Hospital (No. PI-5053) and individual consent for this retrospective analysis was waived due to the retrospective nature of this study, the absence of human or animal samples and the anonymous collection of analytical data.
Statistical analysis
Data were collected in Microsoft Excel software version 2010 (Redmond, WA, USA), and analyzed with SPSS Statistic version 22 (Chicago, IL, USA). The Kolmogorov-Smirnoff and Shapiro-Wilk tests were used to compare the distributions of numerical variables. For continuous variables normally distributed, Student t-test of independent samples was used, and were expressed as mean and standard deviation (SD). To analyze continuous data not normally distributed, Mann-Whitney test was used, and were expressed as median and interquartile range (Q1-Q3). Discrete variables were expressed as frequency (n) and percentages (%), and were analyzed by Chi square test, or Fisher’s test when the first one could not be applied. Odds ratios (OR) were calculated with 95% confidence intervals. Sensitivity and specificity analysis of the parameters evaluated for postoperative complication rate, readmission rate and prolonged admission rate were determined by the area under the curve (AUC) represented on the receiver operating characteristic (ROC) curves. Optimal cut-off values were defined as the point at which the value of “sensitivity + specificity − 1” was maximum using Youden’s index (16). The AUCs were compared using DeLong’s method (17). Diagnostic cutoff values of these markers for the prediction of SSI were based on the significance in the univariate analysis. Variables with a P value <0.05 in the univariate analysis were then entered into the multivariate analysis. All statistical calculations were performed with two tails and the statistical significance was established with a value of P<0.05. To calculate the estimated sample size in our population, with an incidence of approximately 5% of the observed event (SSI) and with an estimated error of 1%, a sample size of 1,054 individuals is required to detect significant differences.
Results
A total of 1,136 patients (710 males and 426 females) were included, with a median age at diagnosis of 10.3 years (8.1–12.8). Surgical site infection was reported in 53 patients (4.7%) during the 30-day follow-up after appendectomy (SSI group), with no demographic differences with the control group. However, time from symptom onset and ultrasound appendiceal diameter were both significantly higher in patients who developed SSI. Complicated appendicitis was observed in about 60% patients of both groups, without differences in surgical approach between them. Surgery time was statistically superior in the SSI group, with a mean of 15 minutes longer than the control group (P<0.001). Demographic data, time since symptom onset, ultrasound diameter and intraoperative findings are shown in Table 1.
Table 1
| SSI group (n=53) | Control group (n=1,083) | P value | |
|---|---|---|---|
| Gender, n (%) | 0.971 | ||
| Male | 33 (62.3) | 677 (62.5) | |
| Female | 20 (37.7) | 406 (37.5) | |
| Age (years), average (SD) | 10.9 (2.9) | 10.3 (3.3) | 0.270 |
| Time since symptom onset (hours), median [Q1–Q3] | 24 [20–48] | 18 [12–36] | 0.034 |
| Ultrasound appendiceal diameter (mm), median [Q1–Q3] | 10 [9–13.5] | 9 [8–11] | 0.010 |
| Surgical approach, n (%) | 0.631 | ||
| Open | 31 (58.5) | 669 (61.7) | |
| Laparoscopic | 22 (41.5) | 414 (38.3) | |
| Type of acute appendicitis, n (%) | 0.711 | ||
| Complicated | 31 (58.5) | 661 (61.0) | |
| Uncomplicated | 22 (41.5) | 422 (39.0) | |
| Surgery time (min); average (SD) | 62.4 (27.8) | 47.9 (19.9) | <0.001 |
SD, standard deviation; Q1-Q3, interquartile range.
Regarding laboratory test at admission, SSI group patients presented significantly higher counts of leukocytes, neutrophils and NLR than control group, with no differences in platelets and fibrinogen counts. Table 2 compares the laboratory values between the two groups. When performing sensitivity and specificity analysis fo SSI using the ROC curve (Figure 1), NLR was the parameter with the highest AUC of those analyzed, this difference being statistically significant. A NLR cut-off point of 9.8 was calculated for a maximum sensitivity and specificity of 77.8% and 72.7%, respectively. The results of multivariate analysis suggested that the increased NLR is an independent predictive indexes for SSI [OR 1.82 (1.13–2.73); P<0.01]. Table 3 shows AUC, cut-off points, sensitivity, specificity and multivariate analysis of the different parameters analyzed for the development of SSI after appendectomy in children.
Table 2
| SSI group (n=53)* | Control group (n=1,083)* | P value | |
|---|---|---|---|
| Leukocytes (103/µL) | 17,775 (14,700–19,730) | 14,930 (11,600–17,800) | 0.002 |
| Neutrophils (103/µL) | 15,304 (12,100–17,380) | 11,840 (8,780–14,710) | <0.001 |
| Lymphocytes (103/µL) | 7,590 (858–1,650) | 1,951 (1,265–2,390) | <0.001 |
| NLR | 12.8 (9.1–15.6) | 7.6 (4.1–10.3) | <0.001 |
| CRP (mg/L) | 80.6 (9–125) | 38.5 (1.8–50.4) | 0.011 |
| Platelets (/µL) | 289,760 (238,000–340,000) | 278,000 (236,000–322,000) | 0.582 |
| Fibrinogen (mg/dL) | 499 (388–713) | 424 (338–516) | 0.451 |
*, Medians and interquartile ranges (Q1-Q3) for each value are presented. NLR, neutrophil-to-lymphocyte ratio; CRP, C-reactive protein.
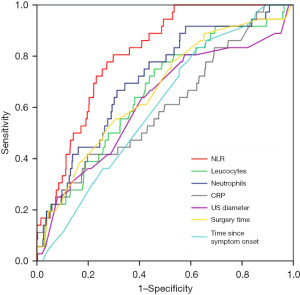
Table 3
| Sensitivity and specificity analysis (ROC curve) | Multivariate analysis | |||||||
|---|---|---|---|---|---|---|---|---|
| AUC (95% CI) | Cut-off point | Sensitivity (%) | Specificity (%) | P value | OR (95% CI) | P value | ||
| NLR | 0.808 (0.754–0.862) | 9.8 | 77.8 | 72.7 | <0.001 | 1.82 (1.13–2.73) | <0.001 | |
| Neutrophils (103/µL) | 0.711 (0.628–0.793) | 12,380 | 77.8 | 56.2 | <0.001 | 1.57 (0.98–2.68) | 0.052 | |
| Leukocytes (103/µL) | 0.660 (0.571–0.750) | 15,290 | 75.0 | 54.2 | 0.001 | 1.32 (0.84–2.45) | 0.067 | |
| CRP (mg/L) | 0.605 (0.507–0.703) | 60.5 | 38.9 | 80.3 | 0.032 | 1.15 (0.65–2.39) | 0.074 | |
| US diameter (mm) | 0.622 (0.521–0.723) | 10 | 63.9 | 59.0 | 0.013 | 1.09 (0.66–3.48) | 0.061 | |
| Surgery time (minutes) | 0.666 (0.576–0.757) | 55 | 55.6 | 69.2 | 0.001 | 1.23 (0.74–2.57) | 0.082 | |
| Time since symptom onset (hours) | 0.604 (0.523–0.685) | 18 | 83.3 | 37.2 | 0.034 | 1.12 (0.78–2.53) | 0.121 | |
AUC >0.600 and P<0.05 were accepted as significant. CI, confidence interval; ROC, receiver operating characteristic; AUC, area under the curve; NLR, neutrophil-to-lymphocyte ratio; CRP, C-reactive protein; US, ultrasound.
Discussion
This is the first study to determine the role of NLR as a predictor of SSI in children with AA. The results obtained show that NLR has a stronger capacity to predict the development of SSI than the quantitative factors studied up to now (time from symptom onset, ultrasound appendiceal diameter and surgery time) and presents a higher sensitivity and specificity than other acute-phase reactants such as leukocytes, neutrophils and CRP.
The incidence of SSI in our study was 4.7%, similar to that described by other authors (18). SSI and control groups can be considered comparable, since there were no differences in demographic data or complicated/uncomplicated appendicitis between them. Open appendectomy was the most frequent surgical approach in the two groups, with no differences in the incidence of SSI between them. These findings are in line with those reported by Brill et al., who observed no differences in SWI rate when comparing open versus laparoscopic approaches (19). SSI are associated with increased length of hospital stay as well as a 2- to 11-fold increase in the risk of mortality (20). Although most patients recover from an SSI without long-term adverse sequelae, 77% of mortality in patients with an SSI can be attributed to the infection itself (21). In addition, SSI ranks as the most costly of the hospital-acquired infections, with an annual cost estimated at $3.5 to $10 billion in the US (21). These increased costs are driven by increased length of stay, Emergency Department visits, and readmissions (22). Therefore, early detection of SSI is essential to reduce the negative impact on patients, in addition to the associated costs (23).
The relevance of this study lies in the fact that it proposes a simple way of predicting the risk of SSI after appendectomy in children from the laboratory tests at admission. NLR presents a high sensitivity and specificity for predicting the subsequent development of SSI, which reach their maximum values at the cut-off point of 9.8. These parameters determine NLR internal validity for predicting the risk of SSI, and are therefore independent of prevalence. External validity parameters such as positive and negative predictive values have not been analyzed in this study, they are dependent on the prevalence of SSI.
NLR is considered an inflammatory biomarker that has been used for the diagnosis of acute appendicitis since its first description more than 20 years ago (24), and some authors have subsequently proposed using it as a cut-off point for conservative or surgical treatment (25). In our institution we have recently analyzed the involvement of NLR as a prognostic factor in the clinical course of AA in pediatric patients. It has been reported that values higher than 8.75 were related to the presence of peritonitis, and values higher than 10.5 were related to the development of postoperative intra-abdominal abscess after appendectomy (12,13). NLR can be understood as a reflection of the systemic inflammatory activity associated with a particular local process, as in this case AA. Triggering of local inflammatory response in cecal appendix causes an increase in neutrophil proliferation mediated by growth factors on hematopoietic stem cells, and an increase in lymphocyte apoptosis mediated by tumor necrosis factor-alpha (TNF-alpha) (26). This leads to changes in blood cell components, which are typically determined by an increase in neutrophils and a decrease in lymphocytes (27). Therefore, NLR higher values are associated with more intense inflammatory disorders. In relation to this, the results of our study establish a cut-off point of 9.8 for the development of SSI, which is in between the cut-off point for peritonitis (8.75) and that for intra-abdominal abscess (10.5). Thus, admission NLR value represents the underlying inflammatory response of each patient, and allows us to predict the clinical course after surgery in each case. NLR has recently been evaluated as a predictor of SSI for other sites, such as following mesh repair of groin hernia (28), prosthetic joint infections (29) or infection after spinal decompression surgery (30). However, all these studies were conducted on adult patients, with no studies in children to date.
One of the main advantages of NLR over other acute-phase reactants is its simple determination from blood count parameters as well as its cost-effectiveness because it can be measured in almost all laboratories. Predicting risk of SSI can help pediatricians and pediatric surgeons to educate, inform, and arrange appropriate infection monitoring protocol. Identification of patients at high risk of SSI allows early start of preventive measures according to WHO Global Guidelines for the prevention of SSI (31,32). Patients and parents should be instructed and warned of the signs and symptoms of SSI before discharge, and they also can be provided with recommendation sheets or self-assessment questionnaires, which have proven to be helpful in the early diagnosis of SSI (33).
The limitations of our study mainly result from its single-center and retrospective design. In addition, these results cannot be extrapolated to children under 5 years of age, because of the physiological differences in white blood cell counts observed in this group of age (14). The lymphocyte count is low during infancy and progressively increase to its highest level at 6 months of age. Subsequently there is a moderate and continuous decline in the count until approximately 9 years of age. Neutrophil count pattern changes with age in a opposite manner to that of lymphocyte count. Besides, there are two inter-sections of lymphocyte count and neutrophil count during infancy and at approximately 5 years of age, based on locally weighted regression analysis (14). For this reason, patients aged 5 years have been excluded from this study, as they have different physiological values of neutrophils and lymphocytes, and therefore cannot be compared with the values of the rest of the patients, as we would be committing a selection bias.
Although the substantial sample size of this study has allowed the detection of statistically significant differences, it is difficult to determine the existence of confounding factors affecting NLR validity. As this is the first study to analyze the relationship between NLR and SSI, it is not possible to compare the results obtained, so further prospective multicenter studies are needed to determine if standardized cut-off values for NLR can successfully predict the risk of developing SSI.
Conclusions
NLR value at admission was the most promising predictive factor for the development of SSI in children undergoing appendectomy. It is an easy, simple, inexpensive, and rapid method to detect patients at high risk for SSI and to initiate preventive measures in these selected cases.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-360/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-360/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-360/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and was approved by institutional review board of La Paz Children’s Hospital (No. PI-5053) and individual consent for this retrospective analysis was waived due to the retrospective nature of this study, the absence of human or animal samples and the anonymous collection of analytical data.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Salminen P. Acute Appendicitis Incidence-Predisposing Factors, From Microbiota to Socioeconomic Status? JAMA Surg 2020;155:338-9. [Crossref] [PubMed]
- Leung TT, Dixon E, Gill M, et al. Bowel obstruction following appendectomy: what is the true incidence? Ann Surg 2009;250:51-3. [Crossref] [PubMed]
- Casanova JF, Herruzo R, Diez J. Risk factors for surgical site infection in children. Infect Control Hosp Epidemiol 2006;27:709-15. [Crossref] [PubMed]
- Varik K, Kirsimägi U, Värimäe EA, et al. Incidence and risk factors of surgical wound infection in children: a prospective study. Scand J Surg 2010;99:162-6. [Crossref] [PubMed]
- Badia JM, Casey AL, Petrosillo N, et al. Impact of surgical site infection on healthcare costs and patient outcomes: a systematic review in six European countries. J Hosp Infect 2017;96:1-15. [Crossref] [PubMed]
- Perencevich EN, Sands KE, Cosgrove SE, et al. Health and economic impact of surgical site infections diagnosed after hospital discharge. Emerg Infect Dis 2003;9:196-203. [Crossref] [PubMed]
- Teixeira PG, Sivrikoz E, Inaba K, et al. Appendectomy timing: waiting until the next morning increases the risk of surgical site infections. Ann Surg 2012;256:538-43. [Crossref] [PubMed]
- Liang HH, Wang W, Huang MT, et al. Appendix diameter: a predictor of wound infection after laparoscopic appendectomy. Am Surg 2011;77:307-10. [Crossref] [PubMed]
- Horwitz JR, Chwals WJ, Doski JJ, et al. Pediatric wound infections: a prospective multicenter study. Ann Surg 1998;227:553-8. [Crossref] [PubMed]
- Yazici M, Ozkisacik S, Oztan MO, et al. Neutrophil/lymphocyte ratio in the diagnosis of childhood appendicitis. Turk J Pediatr 2010;52:400-3. [PubMed]
- Celik B, Nalcacioglu H, Ozcatal M, et al. Role of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in identifying complicated appendicitis in the pediatric emergency department. Ulus Travma Acil Cerrahi Derg 2019;25:222-8. [PubMed]
- Delgado-Miguel C, Muñoz-Serrano AJ, Barrena S, et al. Neutrophil-to-lymphocyte ratio as a predictor of peritonitis in acute appendicitis in children. Cir Pediatr 2019;32:185-9. [PubMed]
- Delgado-Miguel C, Muñoz-Serrano AJ, Núñez V, et al. Neutropthil-to-Lymphocyte Ratio as a Predictor of Postsurgical Intraabdominal Abscess in Children Operated for Acute Appendicitis. Front Pediatr 2019;7:424. [Crossref] [PubMed]
- Li K, Peng YG, Yan RH, et al. Age-dependent changes of total and differential white blood cell counts in children. Chin Med J (Engl) 2020;133:1900-7. [Crossref] [PubMed]
- CDC/NHSN Procedure-associated Module. Surgical Site Infection (SSI) Event. Accessed July 25, 2021 Available online: https://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf
- Fluss R, Faraggi D, Reiser B. Estimation of the Youden Index and its associated cutoff point. Biom J 2005;47:458-72. [Crossref] [PubMed]
- DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988;44:837-45. [Crossref] [PubMed]
- Siribumrungwong B, Chantip A, Noorit P, et al. Comparison of Superficial Surgical Site Infection Between Delayed Primary Versus Primary Wound Closure in Complicated Appendicitis: A Randomized Controlled Trial. Ann Surg 2018;267:631-7. [Crossref] [PubMed]
- Brill A, Ghosh K, Gunnarsson C, et al. The effects of laparoscopic cholecystectomy, hysterectomy, and appendectomy on nosocomial infection risks. Surg Endosc 2008;22:1112-8. [Crossref] [PubMed]
- Anderson DJ, Podgorny K, Berríos-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol 2014;35:605-27. [Crossref] [PubMed]
- Magill SS, Edwards JR, Bamberg W, et al. Multistate pointprevalence survey of health care-associated infections. N Engl J Med 2014;370:1198e1208
- Fry DE. The economic costs of surgical site infection. Surg Infect (Larchmt) 2002;3:S37-43. [Crossref] [PubMed]
- Andersson AE, Bergh I, Karlsson J, Nilsson K. Patients’ experiences of acquiring a deep surgical site infection: an interview study. Am J Infect Control 2010;38:711-7. [Crossref] [PubMed]
- Goodman DA, Goodman CB, Monk JS. Use of the neutrophil:lymphocyte ratio in the diagnosis of appendicitis. Am Surg 1995;61:257-9. [PubMed]
- Shimizu T, Ishizuka M, Kubota K. A lower neutrophil to lymphocyte ratio is closely associated with catarrhal appendicitis versus severe appendicitis. Surg Today 2016;46:84-9. [Crossref] [PubMed]
- Zahorec R. Ratio of neutrophil to lymphocyte counts: rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy 2001;102:5-14. [PubMed]
- de Jager CP, van Wijk PT, Mathoera RB, et al. Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care 2010;14:R192. [Crossref] [PubMed]
- Zhuo Y, Cai D, Chen J, et al. Pre-surgical peripheral blood inflammation markers predict surgical site infection following mesh repair of groin hernia. Medicine (Baltimore) 2021;100:e25007. [Crossref] [PubMed]
- Zhao G, Chen J, Wang J, et al. Predictive values of the postoperative neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and lymphocyte-to-monocyte ratio for the diagnosis of early periprosthetic joint infections: a preliminary study. J Orthop Surg Res 2020;15:571. [Crossref] [PubMed]
- Inose H, Kobayashi Y, Yuasa M, et al. Postoperative lymphocyte percentage and neutrophil-lymphocyte ratio are useful markers for the early prediction of surgical site infection in spinal decompression surgery. J Orthop Surg (Hong Kong) 2020;28:2309499020918402. [Crossref] [PubMed]
- Allegranzi B, Zayed B, Bischoff P, et al. New WHO recommendations on intraoperative and postoperative measures for surgical site infection prevention: an evidence-based global perspective. Lancet Infect Dis 2016;16:e288-303. [Crossref] [PubMed]
- Ling ML, Apisarnthanarak A, Abbas A, et al. APSIC guidelines for the prevention of surgical site infections. Antimicrob Resist Infect Control 2019;8:174. [Crossref] [PubMed]
- Pham JC, Ashton MJ, Kimata C, et al. Surgical site infection: comparing surgeon versus patient self-report. J Surg Res 2016;202:95-102. [Crossref] [PubMed]


