
Nursing care of a child with severe interstitial pneumonia complicated by acute rejection after lung transplantation: a case report
Highlight box
Key findings
• Anti-infection, anti-rejection, and symptomatic measures in the acute phase plays an important role in controlling disease progression and improve the prognosis in pediatric acute rejection after lung transplantation.
What is known and what is new?
• There were just over 100 lung transplant procedures performed in children in 2017 due to its high difficulty. A previous study has shown that transplant patients have a 1.5-year survival of up to 91%.
• Characteristics of acute rejection after lung transplantation in children include acute onset, rapid progression, high difficulty for nursing and frustration in communication with children.
What is the implication, and what should change now?
• Anti-infection, anti-rejection, and symptomatic measures must be administered to the patients by nurses under strict medical supervision. Monitoring of immune drugs and body fluid ensure a proper concentration and optimal effect of medicine, while management of infection prevents worsening of complications.
Introduction
Interstitial pneumonia disease (ILD) refers to a group of chronic lung disorders characterized by inflammation and fibrosis that damage alveolar units and perialveolar tissue. Currently available treatments include antifibrotic therapy, immunotherapy, and transplantation (1). In children, transplantation is of paramount importance as a lifesaving procedure. However, records show a limited number of lung transplant surgeries (just over 100) in children in 2017 owing to the significant difficulty in conducting the procedure (2). A previous study has reported a 1.5-year survival of up to 91% in transplant patients (3). According to reports of the International Society for Heart and Lung Transplantation (ISHLT), about one-third of transplant patients develop acute rejection at least once within a year (4). Acute rejection after transplantation is caused by a complex immune response following the detection of the major histocompatibility complex of donors in recipients and is commonly treated using hormone pulse and symptomatic combined therapeutic approaches. As one of the risk factors of chronic rejection, acute rejection is a leading cause of patient death (5). Therefore, early prevention of transplant rejection and monitoring of these patients is an urgent clinical challenge. Acute rejection after lung transplantation in children is relatively rare, with only reports of sporadic cases so far. Moreno et al. (6) reported a pediatric lung transplantation program involving three infants suffering from interstitial pneumonia while Shepherd et al. (7) documented the results of lung transplantation in four adults with acute interstitial pneumonia. However, these previous studies focused on treatments rather than nursing care strategies. Here, we present a case of a 10-year-old female who developed acute rejection to a double-lung transplant for interstitial pneumonia and was admitted to the pediatric department in our hospital. Following medical treatment and nursing, the patient achieved recovery and was safely discharged. The characteristics of the patient were young age and rare primary disease complicated by acute rejection. To our knowledge, this is the first case report to summarize patient characteristics and successful nursing strategies for acute rejection after lung transplantation in children with severe interstitial pneumonia, which may provide effective guidance for healthcare professionals in this field. This case report was prepared following the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-264/rc).
Case presentation
A 10-year-old female was admitted to our hospital with cough as the chief complaint for a week and fever for a day. The patient was diagnosed with interstitial pneumonia 3 months previously and underwent lung transplantation successfully under general anesthesia. Following the stabilization of her condition, the patient was discharged in August 2021. General examination showed that the patient was in clear consciousness with blood oxygen saturation of 82% when inhaling air and malnutrition. The patient presented with a flat thorax with visible surgical scar of 33 cm, with audible rough lung respiratory sound and moist rale. Accessory examination revealed thickened right ventricular septum. Imaging tests showed a small amount of bilateral pleural effusion, multiple new exudations in the transplanted double lung, and multiple swollen bilateral hilar and mediastinal lymph nodes. The diagnosis upon admission was severe pneumonia, double lung transplant status, pulmonary heart disease and severe malnutrition.
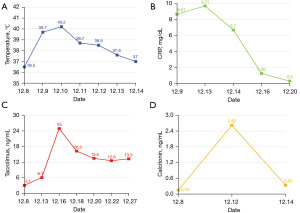
Further examinations were performed after admission and the patient was transferred to a pediatric department on December 9, 2021, presenting with high fever (39.2 ℃) with chills, CRP of 8.67 mg/dL and CT of 0.16 ng/mL. Meropenem, sulfamethoxazole, and oseltamivir phosphate were administered as anti-infection therapy and calcineurin inhibitors and antimetabolites combined with hormones in small doses used for anti-rejection therapy. On December 13, 2021, acute rejection was suspected after bronchoalveolar lavage via bronchoscopy in addition to lung tissue biopsy. Consequently, meropenem was replaced with tazocin as anti-infection therapy. In total, 120 mg of methylprednisolone was used for shock therapy, with a gradual reduction of the dose to 20 mg. On December 27, 2021, the patient had improved oxygen saturation of blood when inhaling air, with no symptoms of fever or cough. CRP was reduced to 0.30 mg/dL in balance bilateral pleural effusion was basically absorbed, and the patient was discharged.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and the declaration of Helsinki (2013 revision). Written informed consent was obtained from the patient’s parents for publication of this case report. A copy of the written consent form is available for review by the editorial office of this journal.
Nursing care
Monitoring and management of immunosuppressants
Successful lung transplantation is dependent on the efficacy of immunosuppressants (8). Administration of excessive immunosuppressant can lead to increased risk of infection in transplant patients. Therefore, flexibility and complexity of treatments and compliance of patients are of paramount significance to maximize the therapeutic effect (9). In this case, oseltamivir phosphate (mainly tacrolimus) and antimetabolites (mycophenolate mofetil) combined with hormones in small doses were administered for treatment (8). Timely observation of the blood concentration of tacrolimus and personalized therapeutic delivery is of great importance due to its susceptibility to other drugs (10). On December 18, 2021, 12.5 mg thymoglobulin was administered under medical supervision for symptomatic treatment. Following intravenous injection, thymoglobulin can cause damage to vascular walls and endothelial cells, leading to thrombophlebitis (11). Therefore, the therapeutic regimen was divided into two fractions. One-tenth of the first fraction of thymoglobulin was combined with 50 mL of saline and dripped intravenously at the rate of 25 mL/h. The rest of the drug was combined with 100 mL saline and dripped intravenously if no discomfort was experienced by the patient. The rate of dripping and amount of remaining drug were monitored every 30 minutes by the chief nurses. Considering the related literature (12), our nursing team developed a protocol for the patient that involved testing blood at 06:30, 18:30, administering drugs at 07:00, 19:00, and having meals at 08:00, 20:00. The patient was advised not to eat an hour before or after taking medicine due to the impact of fat on the absorption of tacrolimus. Consciousness, vital signs and allergic condition were closely monitored during the treatment period. Family-style nursing care was provided due to the young age and relatively poor compliance of the patient and her parents were provided extensive information on the lung transplantation procedure and encouraged to participate over the whole course of nursing. Therapeutic drugs were administered throughout the hospitalization period.
Adverse reactions and management
According to the report of the chief nurses during the MDT case discussion held shortly after admission of the patient in our hospital, the patient had stopped taking voriconazole, which could induce a significant increase in the concentration of tacrolimus after standardized preventive anti-fungal therapy within 3 months of surgery. Rejection developed due to an unsatisfactory concentration of tacrolimus resulting from a low white blood cell count and lack of timely increase in the tacrolimus dose. The target concentration of tacrolimus was adjusted to 12 to 16 ng/mL according to the condition of patient. However, the estimated concentration on December 9, 2021, was approximately 3.1 ng/mL, which was significantly lower than the target concentration. The dose of tacrolimus for long-term treatment was therefore set as 2.5 mg. The concentration measured on December 16, 2021, was 25.0 ng/mL. Consequently, the dose was adjusted to 0.5 mg, administration of tacrolimus streamlined, and cancidas replaced with voriconazole (13) for stabilizing the tacrolimus concentration to ~13 ng/mL until the patient was discharged. A summary of the treatment and events is presented in Table 1 and the outcome measures at different stages of the disease shown in Figure 1.
Table 1
| Treatment/event | Time | Treatment plans for different periods |
|---|---|---|
| Anti-infection | Dec. 9th | Meropenem, oseltamivir phosphate granules (anti-virus), compound sulfamethoxazole tablets (to prevent pneumocystis carinii pneumonia) |
| Dec. 10th | Meropenem, sulfamethoxazole, oseltamivir phosphate | |
| Dec. 12th | Teicoplanin, mepem, sulfonamide added | |
| Dec. 14th | Mepem, targocid, cancidas, cymevene | |
| Dec. 15th | Mepem, targocid, cymevene, cancidas, zithromax | |
| Dec. 16th | Streamlined anti-infection therapy: tazocin, zithromax, voriconazole(anti-infection) | |
| Dec. 17th | Infected with mycoplasma, tazocin, voriconazole (anti-infection) | |
| Anti-rejection | Dec. 9th | Medrol, CellCept capsules, Prograf capsules, Corlentor tablets |
| Dec. 10th | Medrol, mycophenolate mofetil, tacrolimus capsules | |
| Dec. 13th | Methylprednisolone 120 mg added | |
| Dec. 15th | Methylprednisolone 80 mg for dysphoria | |
| Dec. 16th | Methylprednisolone 40 mg, thymoglobulin added | |
| Dec. 22th | Thymoglobulin combined with tacrolimus, prednisone acetate, mycophenolate mofetil | |
| Events | Dec. 9th | Fever |
| Dec. 13th | Bronchoscopy | |
| Dec. 14th | Diagnosed with acute rejection | |
| Dec. 15th | Anti-infection therapy streamlined | |
| Dec. 18th | Multiple exudation in double-lung, bilateral pleural effusion alleviated | |
| Dec. 19th | Volume of body fluid in balance, albumin 32.1 g/L, WBC 6.57×109 g/L | |
| Dec. 27th | No fever or cough, CRP 0.30 mg/dL in balance, bilateral pleural effusion absorbed, discharged |
The anti-infection and anti-rejection therapy were stopped on Dec. 17th and 22th, respectively. Dec., December; CRP, C-reactive protein; WBC, white blood cell count.
Prevention and control of infection
In lung transplant patients, removal of secretions in airways is difficult due to denervation and poor cough reflex of transplanted lung, which often leads to repeated infection of the patient. According to statistics, the incidence of infection in recipients of lung transplantation in China is up to 60% (14) and largely responsible for rehospitalization and even death of patients (15). Children are more susceptible to infection due to relative poor immunity, surgical injuries and administration of immunosuppressants (16). In this case, the patient developed fever on December 9, 2021, with the highest recorded temperature of 39.7 ℃, expectoration, CRP of 8.67 mg/mL, and CT of 0.16 ng/mL. X-ray analysis revealed a small amount of bilateral pleural effusion and multiple exudations in the transplanted double-lung (mainly the right side). Seated oxygen therapy was performed under medical supervision by chief nurses. The volume and viscosity of sputum were dynamically evaluated every 4 h and sputum suction was performed when needed. A warm sponge bath was given to the patient and the temperature examined after 30 min, with regular monitoring every four hours. Sodium bicarbonate mouthwash was administered to clean the oral cavity for prevention of infection. In response to these active prevention and control measures, the temperature of the patient returned to normal on December 14, CRP decreased to 0.30 mg/dL on December 18, bilateral pleural effusion was basically absorbed according to X-ray analysis on December 28, and interstitial-parenchymal diseases in the transplanted double-lung were significantly reduced.
Dynamic management of body fluid
Poor management of body fluid is the major cause of primary graft dysfunction (PGD) (17). Excess body fluid of the patient places extra workload on the heart while insufficient body fluid results in hypotension. Therefore, adoption of dynamic evaluation and adjustment of body fluid may improve oxygenation and recovery of lung function in patients undergoing lung transplantation (18). On December 14, the volume of body fluid in the patient within 24 h was over 600 mL, with presentation of eyelid edema. To treat this condition, furosemide (10 mg) was injected intravenously under medical supervision. On December 15, the increased volume of body fluid within 24 h was reduced to 150 mL. Urine volume and stool weight were measured using high-precision containers and pumps, respectively, by the chief nurses. The volume of daily fluid infusion was recorded in the nursing system. Vital signs and condition of electrolytes in the patient were closely monitored. The parents were informed about the susceptibility of the patients to electrolyte disturbances and potential adverse outcomes. The patient was advised to rest, elevate the pillow when sleeping to reduce swelling and take care of her eyelid. On December 16, the albumin level in the patient was reduced to 29.5 g/L, with consequent infusion of 10 g human albumin under medical supervision. Albumin was infused slowly in the first 15 min and the patient monitored for adverse reactions. The rate of infusion was conducted at 50 mL/h using a micro infusion pump to increase blood volume and maintain stable plasma colloid osmotic pressure. On December 19, the body fluid volume in the patient was in balance, albumin level increased to 32.1 g/L and white blood cell count was 6.57×109 g/L. Peripheraloxygen saturation of blood during inhalation was maintained at 96% to 98%.
Personalized nutritional support
Nutritional supply is critical at each stage of lung transplantation. Failure to provide adequate nutritional support to meet the needs of the body can lead to significant adverse outcomes, including impaired immune function, delayed wound healing and reduction in endurance of respiratory muscles, affecting quality of life (19). The BMI of our patient was 12.5, with evidence of severe malnutrition and inadequate protein-energy status. Based on the related literature, the chief nurses created an individual nutrition file for the patient, including general data, dietary habits, nutritional condition, and personalized nutrition program. In this case, if the estimated demand of protein was 1.3 to 1.5 g/(kg·d) and it increased to 2.5 g/(kg·d) when experiencing severe malnutrition (20), it increased to 50 g/(kg·d) in this patient. The patient was encouraged to consume food high in nutrients and protein, including fish, eggs, and milk and her parents were advised to teach her to eat slowly to prevent choking and aspiration. TG in the patient was 2.95 mmol/L, indicative of hypercholesterolemia. Therefore, limited consumption of cholesterol, such as lard and animal organs, was recommended (19). The weight of the patient was recorded once a week. Nutritional risk screening was performed every 5 days and documented using an electronic medical record system. The nutrition program was dynamically adjusted according to the condition as well as consumption and absorption characteristics of the patient. Her parents were advised to provide a traditional Chinese medicine (TCM) diet with four ingredients as a soup mixture once a day, incorporating 10 g of coix, lotus seeds, Chinese yam, Wolfiporia extensa, 15 g of ginger, Chen Pi and Astragalus, and pork tripe or snakehead, depending on the condition of the patient. The patient gained about 3.3 pounds and her mental state improved prior to discharge.
Psychological care
Patients undergoing lung transplantation are susceptible to negative emotions, including self-abasement and depression (21). In this case, the patient was admitted to the single glass ward closest to the nurses’ station. She was allowed to watch cartoons and the parents remained with her to provide emotional support. When it was necessary to perform invasive manipulation, a reward system was established, whereby the patient was awarded prizes, such as toys, cartoons, or snacks, following the examination or treatment. Meanwhile, a psychologist offered support to the parents to reduce their psychological burden. The medical staff provided as much information on lung transplantation as possible (22). The parents additionally joined the WeChat group for lung transplant patients created by our hospital for more effective communication. Under humanistic care, the patient was able to tolerate the treatment more easily and her parents gained confidence in the therapeutic process.
Rehabilitation nursing
Nursing targets of improvement in life quality and quick adaptation to society were set for the patient due to her being of school age. Rehabilitation programs were established according to the condition of the patient by physical therapists, which encouraged sitting more frequently, trying to adopt a standing position by the bed and walking if possible, ensuring a total time of over one hour for activities. The patient could merely sit at admission but was subsequently able to walk for one hour without any discomfort. Regular training of the breathing valve was administered by the chief nurses throughout hospitalization along with breathing exercises of Zheng Shi, including stretching, back bridging and invisible bicycling. The patient was accompanied by her parents to prevent falling or collision. Regular and long-term postoperative follow-up surveys are essential for long-term survival in children undergoing transplantation (22). In this case, regular follow-up surveys were conducted by nurses in the department of lung transplantation to ensure full understanding of the condition of the patient for rehabilitation and family support. According to follow-up results, the condition of the patient was stable within 2 months and under care of her parents, she was able to perform physical tasks such as cycling, playing outdoors and shopping in supermarkets.
Discussion
Characteristics of acute rejection after lung transplantation in children with interstitial pneumonia include acute onset, rapid progression, considerable difficulty in nursing and frustration in communication. Anti-infection, anti-rejection, and symptomatic measures should be administered to patients by nurses under strict medical supervision. Monitoring and management of immune drugs and body fluid ensures administration of the appropriate concentrations of drugs to facilitate optimal effects while management of infection prevents worsening of complications. Patient quality of life can be improved with the aid of personalized and comprehensive nutrition and rehabilitation programs. The provision of psychological support to patients and their parents relieves tension and stress, thus achieving more rapid recovery. Through the use of these measures, young patients can be successfully discharged in an improved and stable condition.
Acknowledgments
We thank International Science Editing (http://www.internationalscienceediting.com) for editing this manuscript.
Funding: This work was supported by Administration of Traditional Chinese Medicine of Guangdong Province, China (Grant No. 20232110).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-264/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-264/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and the declaration of Helsinki (2013 revision). Written informed consent was obtained from the patient’s parents for publication of this case report. A copy of the written consent form is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Liu L, Gao J. Current status of research on interstitial lung disease complicated with lung cancer. International Journal of Respiration 2021;41:630-5.
- Benoit TM, Benden C. Pediatric lung transplantation: supply and demand. Curr Opin Organ Transplant 2019;24:324-8. [Crossref] [PubMed]
- Sullivan KM, Goldmuntz EA, Keyes-Elstein L, et al. Myeloablative Autologous Stem-Cell Transplantation for Severe Scleroderma. N Engl J Med 2018;378:35-47. [Crossref] [PubMed]
- Potestio C, Jordan D, Kachulis B. Acute postoperative management after lung transplantation. Best Pract Res Clin Anaesthesiol 2017;31:273-84. [Crossref] [PubMed]
- Xu Y, Lian Q, Chen A, et al. New progress on diagnosis and treatment of acute cellular rejection after lung transplantation. Organ Transplantation 2021;5:614-8.
- Moreno A, Maestre J, Balcells J, et al. Lung transplantation in young infants with interstitial pneumonia. Transplant Proc 2003;35:1951-3. [Crossref] [PubMed]
- Shepherd HM, Terada Y, Takahashi T, et al. Acute Interstitial Pneumonia (Hamman-Rich Syndrome) in Lung Transplantation: A Case Series. Transplant Proc 2022;54:2313-6. [Crossref] [PubMed]
- Cui X, Gong L, Hu B, et al. Immunosuppression regimens development following lung transplantation. International Journal of Respiration 2016;36:228-32.
- Shang Y, Liu H, Wang L, et al. Immunosuppressive Medication adherence in liver transplant recipients. Chinese Nursing Management 2017;17:542-7.
- Zhang Z, Zhang S, Li Z, et al. Individualized treatment of FK506 after liver transplantation. China Journal of Modern Medicine 2010;20:628-30, 633.
- Jomphe V, Lands LC, Mailhot G. Nutritional Requirements of Lung Transplant Recipients: Challenges and Considerations. Nutrients 2018;10:790. [Crossref] [PubMed]
- Xu H, Chen J, Qiu H. ICU care after lung transplantation. Chinese Journal of Critical Care & Intensive Care Medicine 2017;3:91-3. (Electronic Edition).
- Zeng F, Liang J, Lan M. Nursing care of 1 patient after combined liver and lung transplantation. Chinese Journal of Nursing 2021;56:1540-3.
- Liu Y, Tan L, Chen Q. Causes And Nursing Strategies For Complications In ICU Patients Undergoing CVC. International Journal of Nursing 2019;38:30-3.
- Alrawashdeh M, Zomak R, Dew MA, et al. Pattern and Predictors of Hospital Readmission During the First Year After Lung Transplantation. Am J Transplant 2017;17:1325-33. [Crossref] [PubMed]
- Pan H, Huang Q, Wang D, et al. Postoperative care of patients with severe primary graft dysfunction after lung transplantation. Chinese Journal of Nursing 2016;51:923-6.
- Zhong J, Yu C, Tao H, et al. Application of fluid management strategy in patients received lung transplantation. Chinese Journal of Nursing 2019;54:678-81.
- Tang Z, Yan Q, Feng L, et al. Bundles Of Nursing Strategy For Kidney Transplant Patients With Phlebitis Due To Intravenously Dripped Thymoglobulin. World Latest Medicine Information 2021;18:362-3.
- Trumbo P, Schlicker S, Yates AA, et al. Dietary reference intakes for energy, carbohydrate, fiber, fat, fatty acids, cholesterol, protein and amino acids. J Am Diet Assoc 2002;102:1621-30. [Crossref] [PubMed]
- Qiao T, Wang W, Gao P, et al. Nutritional support for lung transplant over the perioperative period. Chinese Journal of Clinical Nutrition 2018;26:22-5.
- Winterberg PD, Garro R. Long-Term Outcomes of Kidney Transplantation in Children. Pediatr Clin North Am 2019;66:269-80. [Crossref] [PubMed]
- Yang Q, Li L, Huang P, et al. Current status and prospect of follow-up for pediatric liver transplantation. International Journal of Nursing 2020;39:4022-6.


