
Short-time mortality and severe complications of very premature infants—a multicenter retrospective cohort study from Jiangsu Province during 2019–2021
Highlight box
Key findings
• Three promising risk factors for the mortality and severe complications in premature infants, namely GA at birth, severe asphyxia, and PPHN, and their combination indicates a better diagnostic ability
What is known and what is new?
• Premature birth is a heterogeneous condition with multiple underlying causes and risk factors.GA at birth, severe neonatal asphyxia and PPHN have previously been shown to be related to premature infant.
• GA at birth was a protective factor for death and severe complications, whereas severe neonatal asphyxia and PPHN were independent risk factors for death and severe complications in very premature infants born at less than 32 weeks.
What is the implication, and what should change now?
• We have a clear understanding and direction of the prevention of premature infant mortality and severe complications, which provides a strong basis for prenatal and postnatal clinical care and life quality improvement for premature infants.
Introduction
Premature birth is a heterogeneous condition with multiple underlying causes and risk factors (1,2). Frequently, infants with a gestational age (GA) of <37 weeks at birth are defined as premature infants, <32 weeks as very premature infants, and <28 weeks as extremely premature infants (3). Approximately 1 million infants die each year as a result of premature birth, and even if they survive, many are left with serious sequelae (4).
Preterm birth is the main cause of death in children under the age of 5, accounting for about 35% of the neonatal deaths (1), in recent years, premature babies are significantly increased around the world, at the same time in the neonatal intensive care unit (Neonatal intensive care unit, NICU) hospitalized the proportion of premature babies also increased. The incidence of preterm birth worldwide is about 10.6% (1) while the rate of preterm birth in China has also increased from 5.9% in 2012 to 6.4% (2) in 2018. In the past decade, premature infant survival has significantly improved (3), but still confronted with a high risk of mortality (1) due to the lack of appropriate neonatal care in LMICs.
The management of premature infants has many dimensions, including prenatal and postnatal care, the allocation of limited health resources, quality of care, and long-term health outcomes (5,6). In recent years, beyond just improving the survival rate of premature infants, the quality of life for premature infants has also gained widespread attention. Thus, the concept of “no serious complications” is proposed, meaning that premature infants survive without any of the following serious diseases, including severe brain injury [grade III–IV intraventricular hemorrhage (IVH)], cystic periventricular leukomalacia (PVL), bronchopulmonary dysplasia (BPD), necrotizing enterocolitis (NEC), severe retinopathy of prematurity (ROP), early-onset or late-onset sepsis, and so on (7).
In the absence of effective interventions to prevent premature birth, the survival of infants born within the biological limits of viability depends on the development of perinatal care (8). Different maternal and neonatal characteristics may also influence the neonatal morbidity and mortality, including maternal age, antenatal care, insulin-dependent diabetes, hypertension, polyembryony, birth defects, infant GA, birth weight, antenatal steroids, antenatal antibiotics, caesarean section, delivery room resuscitation, pulmonary surfactant therapy, postnatal steroids and respiratory support, and so on (9-14). Since antenatal use of corticosteroids has been deemed effective in improving neonatal outcomes, the use of antenatal steroids has increased rapidly over the last decade (15,16). Meta-analyses have shown that increased continuous positive airway pressure (CPAP) and reduced intubation have a beneficial effect on reducing BPD, whereas reduced postnatal steroid use increases the risk of BPD (17).
Currently, there are few multicenter clinical studies on the correlation of risk factors and serious complications of mortality in very premature infants in China, especially in eastern China (14). In this study, we aimed to investigate the risk factors for the mortality and serious complications in very premature infants less than 32 weeks of GA, so as to guide the antenatal and postnatal care of very premature infants, which provides a clinical basis for further improving the survival rate and long-term quality of life for very premature infants. We present the following article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-83/rc).
Methods
Participants
The research was conducted retrospectively. The premature infants with a GA less than 32 weeks who were admitted to the hospital or delivered in the delivery room from 00:00, 1 January 2019 to 24:00, 31 December 2021 from 15 member hospitals of the Neonatal Intensive Care Unit (NICU) Multi-center Clinical Research Collaboration Group on breast milk quality improvement in Jiangsu Province were recruited on the day of admission, and uniformly managed according to the protocol of the intensive care unit (ICU). The premature infants with known severe congenital malformations or inherited metabolic diseases, missing data, and withdrawal of resuscitation care at birth were excluded.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Central ethics approval was obtained from the Medical Ethics Committee of Nanjing Maternity and Child Health Care Hospital [Reference No. (2018) KY-054]. In addition to the first author’s unit (Nanjing Maternity and Child Health Care Hospital), the other 14 hospitals are also informed and agreed with the study. Because only anonymous clinical information was collected, no individual informed consent was obtained.
The main outcomes of enrolled infants
We recorded the survival status of enrolled infants without transfers and obtained the final outcomes of infants for whom treatment had been discontinued or had been transferred to other hospitals in 1–2 months by telephone follow-up. The primary outcome was survival without severe complications, mainly the discharged neonates still alive in the 1–2 months post-discharge follow-up. The secondary outcome referred to death or very premature infants discharged alive without serious complications. The main outcomes of very premature infants in this study are demonstrated in Figure 1.
As shown in Figure 1, [3] and [8] represent infants who had discontinued treatment and survived after discharge; [4], [5], [9], and [10] represent infants who discontinued treatment and died after discharge. They were further categorized into invalid treatment death and abandoned treatment death, based on the guardians’ attitude towards treatment during hospitalization and whether the infant had actually received positive treatment. Invalid treatment death was deemed to be caused by limited medical care, even if the guardians had not withdrawn from treatment; the abandoned treatment death occurred due to family-made decisions, whereby if the guardians had not given up, the infant could have been saved and survived according to the current medical care. The infants, who were transferred to other hospitals for treatment or discharged from hospital in an unstable condition and their guardians abandoned treatment, were visited by telephone follow-up in 1–2 months after transfer or discharge to determine the final condition. The infants who died when their condition was terminal were also classified as invalid treatment death. If contact could not be made, the case was recorded as transferred to other hospitals.
The diagnostic criteria
Survival without severe complications
This status generally refers to premature infants who survived during hospitalization and were discharged without any of the following complications: ≥ grade III IVH or PVL, ≥ stage II NEC, severe BPD, or ≥ stage III or treatment-required ROP.
Severe neonatal complications
Severe neonatal complications included the following 5 diseases with a high incidence in premature infants.
- IVH is defined as IVH associated with ventricular dilatation (grade III IVH) and parenchymal hemorrhage (large unilateral parenchymal density or large unilateral brain cyst).
- Cystic PVL (periventricular white matter echo on ultrasound).
- Bell stage II and III NEC.
- ≥ stage III according to the International Classification of Retinopathy of Prematurity (ICROP) or treated (laser coagulation, intravitreal anti-vascular endothelial growth factor, or surgical treatment) ROP, or ROP without fundus examination.
- BPD represents the oxygen uptake for at least 28 days plus ≥30% oxygen and/or mechanical ventilation support, or sustained positive airway pressure after 36 weeks.
Statistical analysis
The statistical software SPSS26.0 was used for statistical analysis. Data that conformed to a normal distribution were expressed as mean ± standard () deviation and compared between groups by t-test or analysis of variance (ANOVA); Data that did not conform to a normal distribution were expressed as interquartile range (IQR) and compared between groups by non-parametric tests. The enumeration data were expressed by rates and percentages and compared between groups using the chi-square test or Fisher’s exact test. The univariate logistic regression model was used for risk factor analysis for adverse outcomes such as death, and variables with statistically significant differences were selected and then subjected to multivariate logistic regression analysis for the independent risk factors. The Hosmer-Lemeshow test (HL test) was used to verify whether a risk prediction classification model was well calibrated. Receiver operating characteristic (ROC) curve was applied to evaluate the diagnostic value of independent risk factors. The larger the area under curve (AUC), the better the diagnostic ability. Differences were considered statistically significant when P<0.05.
Results
The total number of very premature infants less than 32 weeks of GA enrolled in the study
Among 3,200 very premature infants born at less than 32 weeks of GA, 236 cases died after families abandoned treatment, 64 cases transferred to other hospitals were lost to follow-up, and finally a total of 2,900 very premature infants were included. In the 2,900 very premature infants born at less than 32 weeks GA, 375 cases survived with severe complications (≥ grade III IVH or PVL, ≥ stage II NEC, severe BPD, ≥ stage III or treatment-required ROP), 51 died of severe complications, 83 very premature infants died in-hospital without these severe complications, or died of invalid treatment which caused their guardians to abandon treatment, and 2,391 very premature infants survived without severe complications (Figure 2).
Severe complications in different GA groups of very premature infants
According to the results in Table 1, among the 3,200 very premature infants with GA less than 32 weeks, the GA of 30–31 weeks had the lowest mortality. The proportion of survival without severe complications increased with the increase of GA at birth, whereas the proportion of survival with severe complications decreased with the increase of GA at birth.
Table 1
| Category | <26 w (N=75) | 26–27 w (N=293) | 28–29 w (N=941) | 30–31 w (N=1,591) | χ2 | P value |
|---|---|---|---|---|---|---|
| Survival with severe complications | 39 (52.00) | 90 (30.72) | 165 (17.53) | 132 (8.30) | 201.33 | <0.01 |
| Survival without severe complications | 20 (26.67) | 177 (60.41) | 752 (79.91) | 1,442 (90.63) | 337.46 | <0.01 |
| Death | 16 (21.33) | 26 (8.87) | 24 (2.55) | 17 (1.07) | 90.37 | <0.01* |
P, Person chi-square test; *, Fisher’s exact test. GA, gestational age; w, week.
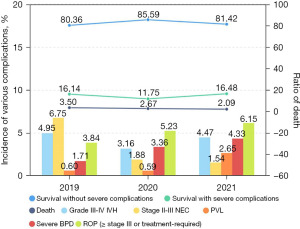
As demonstrated in Figure 3, there was no significant change in the proportion of survival without severe complications, survival with severe complications, and death during the 3-year period. The highest incidence of stage II-III NEC occurred in 2019, since when the incidence has decreased annually. In addition, the incidence of PVL, severe BPD, and ROP (≥ stage III or treatment-required) increased year by year.
The risk factors analysis for the death or severe complications in premature infants of GA <32 weeks
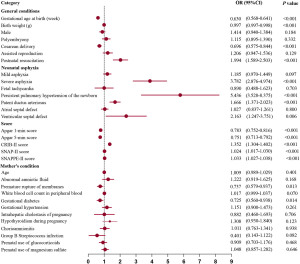
Univariate logistic regression analysis was performed for premature infants who died or experienced severe complications and those without serious complications. There were significant differences in GA, cesarean section, resuscitation therapy after birth, severe neonatal asphyxia, presence of persistent pulmonary hypertension of the newborn (PPHN), patent ductus arteriosus (PDA), ventricular septal defect (VSD), premature rupture of membranes >24 hours, and maternal gestational diabetes mellitus between premature infants with death or severe complications group and infants without serious complications group (P<0.05). In addition, 4 premature infant scores, namely Apgar score, Clinical Risk Index for Babies (CRIB)-II score, Score for Neonatal Acute Physiology (SNAP)-II score, and SNAP-II score, a statistical difference was observed between the two groups (P<0.05, Figure 4).
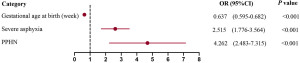
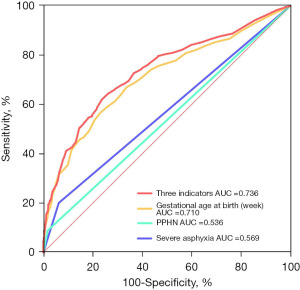
Further multivariate logistic regression analysis (forward, LR) was performed on the significant indicators from the above analysis, and the model (P=0.116) verified by HL test was selected and chosen for further analysis, suggesting that the fitting condition of the model was good. From the multivariate logistic regression score results displayed in Figure 5, we learned that GA at birth was a protective factor for death and serious complications [odds ratio (OR), 95% confidence interval (95% CI): 0.637 (0.595–0.682)], whereas the occurrence of severe neonatal asphyxia [OR (95% CI): 2.515 (1.776–3.564)] and PPHN [OR (95% CI): 4.262 (2.483–7.315)] were independent risk factors for death and serious complications in premature infants <32 weeks GA. Further, ROC curve analysis suggested that the area under the curve (AUC) was the greatest when the 3 indicators of GA at birth, severe asphyxia, and PPHN were combined (AUC =0.736, Figure 6).
Discussion
Premature infants are live born before 37 gestational weeks with poor organ function and adaptive ability (18). They often present clinically with symptoms such as bruising, apnea, lethargy, convulsions, screaming, muscle weakness, and abnormal eye rotation (19,20). In addition, other studies have confirmed that premature infants can also develop mental delays, epilepsy, visual impairment, and other symptoms (21,22). Studies have found that premature infants are prone to have brain injury, the main cause of neurodevelopmental sequelae, which is closely related to the physiological and anatomical characteristics of the developing midbrain of premature infants (23,24). There are still many uncertainties about the causes of premature birth, but in clinical history analysis, chronic diseases such as hypertensive disorders of pregnancy, polyembryony, excess amniotic fluid, heart disease, kidney diseases, liver diseases, diabetes mellitus, endocrine disorders, and so on have been identified as the main causative factors (25-28).
In a report of neonatal research network in the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the incidence of respiratory distress in neonatal respiratory distress syndrome (NRDS) was 93%, ROP 59%, PDA 46%, BPD 42%, LOS 36%, NEC 11%, PVL 3%, and grade III and IV IVH were 7% and 9%, respectively, among 8,515 very low birth weight infants (VLBWI). These complications not just increase the risk of long-term sequelae, they are also significant factors in childhood disability (29,30). During NICU treatment, the survival of premature infants and the incidence of various complications depend not only on birth weight and GA, but also on various perinatal factors and their clinical management (31,32). The routine management of very preterm infants (VPTI) after birth involves temperature, respiration, nutrition, enteral feeding, infection prevention and control, the management of complications, and so on (33). Due to different birth GA, weight, and maturity, each VPTI should fit in a personalized and continuous growth while fighting against diseases, and their prognosis is often in relation to the clinically refined management (34). Therefore, the development of refined management of premature infants in the NICU and multicentral continuous quality improvement can improve the survival rate of VPTI and reduce the incidence of severe complications and case fatality rate.
In this study, we analyzed the risk factors for death and severe complications in the recruited premature infants <32 weeks GA, and determined that GA at birth was a protective factor, and the proportion of survival with severe complications decreased with increasing GA at birth. Besides, the occurrence of severe neonatal asphyxia and PPHN were independent risk factors. The three factors have previously been shown to be related to premature infants. In a previous study on premature infants, Luo et al. constructed a multivariate logistic regression model to analyze the morbidity and mortality of premature infants in different GA and admission year groups, and they observed a higher incidence of moderate-to-severe BPD and sepsis, and the decreased incidence of sepsis and severe ROP (35). In addition, a prognostic study of 752 premature infants, Liu et al. showed that neonatal asphyxia, sepsis, shock, hypoalbuminemia, and severe anemia all could be independent risk factors for the development of NEC in VPTI (36). Other studies have also shown that PPHN as a heterogeneous disease is also a key factor in the morbidity and mortality of premature infants, which is more common in premature infants (37,38). In our study, we finally performed ROC curve analysis, and the results suggested that AUC value was the greatest when combining GA at birth, severe asphyxia and PPHN together.
Conclusions
This study identified three promising risk factors for the mortality and severe complications in premature infants, namely GA at birth, severe asphyxia, and PPHN, and their combination indicates a better diagnostic ability. Based on these results, we have a clear understanding and direction of the prevention of premature infant mortality and severe complications, which provides a strong basis for prenatal and postnatal clinical care and life quality improvement for premature infants.
Acknowledgments
The authors are grateful to Multi-center Clinical Research Collaboration Group for their suggestions and encouragement.
Funding: This work was supported by the Jiangsu Provincial Special funding in Maternal and Child Health (A multicentre cohort study of quality improvement for serious complications in preterm infants less than 32 weeks’ gestational age).
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-83/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-83/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-83/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-83/coif). The authors have no conflicts of interests to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Central ethics approval was obtained from the Medical Ethics Committee of Nanjing Maternity and Child Health Care Hospital [Reference No. (2018) KY-054]. In addition to the first author’s unit (Nanjing Maternity and Child Health Care Hospital), the other 14 hospitals are also informed and agreed with the study. Because only anonymous clinical information was collected, no individual informed consent was obtained.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ajdacic-Gross V, Vetter S, Müller M, et al. Risk factors for stuttering: a secondary analysis of a large data base. Eur Arch Psychiatry Clin Neurosci 2010;260:279-86. [Crossref] [PubMed]
- Marcellin L, Goffinet F, Azria E, et al. Association Between Endometriosis Phenotype and Preterm Birth in France. JAMA Netw Open 2022;5:e2147788. [Crossref] [PubMed]
- Jing J, Dai Y, Li Y, et al. Single-course antenatal corticosteroids is related to faster growth in very-low-birth-weight infant. BMC Pregnancy Childbirth 2021;21:50. [Crossref] [PubMed]
- Chang HH, Larson J, Blencowe H, et al. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet 2013;381:223-34. [Crossref] [PubMed]
- Beck AF, Edwards EM, Horbar JD, et al. The color of health: how racism, segregation, and inequality affect the health and well-being of preterm infants and their families. Pediatr Res 2020;87:227-34. [Crossref] [PubMed]
- Requejo J, Merialdi M, Althabe F, et al. Born too soon: care during pregnancy and childbirth to reduce preterm deliveries and improve health outcomes of the preterm baby. Reprod Health 2013;10:S4. [Crossref] [PubMed]
- Peng X, Song J, Li B, et al. Umbilical cord blood stem cell therapy in premature brain injury: Opportunities and challenges. J Neurosci Res 2020;98:815-25. [Crossref] [PubMed]
- Taylor HG, Klein N, Hack M. School-age consequences of birth weight less than 750 g: a review and update. Dev Neuropsychol 2000;17:289-321. [Crossref] [PubMed]
- Linhart Y, Bashiri A, Maymon E, et al. Congenital anomalies are an independent risk factor for neonatal morbidity and perinatal mortality in preterm birth. Eur J Obstet Gynecol Reprod Biol 2000;90:43-9. [Crossref] [PubMed]
- Bental Y, Reichman B, Shiff Y, et al. Impact of maternal diabetes mellitus on mortality and morbidity of preterm infants (24-33 weeks' gestation). Pediatrics 2011;128:e848-55. [Crossref] [PubMed]
- D'Apremont I, Marshall G, Musalem C, et al. Trends in Perinatal Practices and Neonatal Outcomes of Very Low Birth Weight Infants during a 16-year Period at NEOCOSUR Centers. J Pediatr 2020;225:44-50.e1. [Crossref] [PubMed]
- Hornik CP, Fort P, Clark RH, et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev 2012;88:S69-74. [Crossref] [PubMed]
- Edwards MO, Kotecha SJ, Kotecha S. Respiratory distress of the term newborn infant. Paediatr Respir Rev 2013;14:29-36; quiz 36-7. [Crossref] [PubMed]
- Qi Z, Wang Y, Lin G, et al. Impact of maternal age on neonatal outcomes among very preterm infants admitted to Chinese neonatal intensive care units: a multi-center cohort study. Transl Pediatr 2022;11:1130-9. [Crossref] [PubMed]
- Olaloko O, Mohammed R, Ojha U. Evaluating the use of corticosteroids in preventing and treating bronchopulmonary dysplasia in preterm neonates. Int J Gen Med 2018;11:265-74. [Crossref] [PubMed]
- Barros FC, Bhutta ZA, Batra M, et al. Global report on preterm birth and stillbirth (3 of 7): evidence for effectiveness of interventions. BMC Pregnancy Childbirth 2010;10:S3. [Crossref] [PubMed]
- Subramaniam P, Ho JJ, Davis PG. Prophylactic nasal continuous positive airway pressure for preventing morbidity and mortality in very preterm infants. Cochrane Database Syst Rev 2016;CD001243. [Crossref] [PubMed]
- Allen MC. Neurodevelopmental outcomes of preterm infants. Curr Opin Neurol 2008;21:123-8. [Crossref] [PubMed]
- Haslam RH. Clinical neurological examination of infants and children. Handb Clin Neurol 2013;111:17-25. [Crossref] [PubMed]
- Rogers A, Gage S. Apparent Life-Threatening Event/Brief Resolved Unexplained Event. Nelson Pediatric Symptom-Based Diagnosis E-Book 2022:99.
- Spagnoli C, Falsaperla R, Deolmi M, et al. Symptomatic seizures in preterm newborns: a review on clinical features and prognosis. Ital J Pediatr 2018;44:115. [Crossref] [PubMed]
- Ergaz Z, Ornoy A. Perinatal and early postnatal factors underlying developmental delay and disabilities. Dev Disabil Res Rev 2011;17:59-70. [Crossref] [PubMed]
- Bouza H. The impact of pain in the immature brain. J Matern Fetal Neonatal Med 2009;22:722-32. [Crossref] [PubMed]
- Cordeiro CN, Tsimis M, Burd I. Infections and Brain Development. Obstet Gynecol Surv 2015;70:644-55. [Crossref] [PubMed]
- Narang K, Szymanski LM. Multiple Gestations and Hypertensive Disorders of Pregnancy: What Do We Know? Curr Hypertens Rep 2020;23:1. [Crossref] [PubMed]
- Tanz LJ, Stuart JJ, Missmer SA, et al. Cardiovascular biomarkers in the years following pregnancies complicated by hypertensive disorders or delivered preterm. Pregnancy Hypertens 2018;13:14-21. [Crossref] [PubMed]
- Gonzalez Suarez ML, Kattah A, Grande JP, et al. Renal Disorders in Pregnancy: Core Curriculum 2019. Am J Kidney Dis 2019;73:119-30. [Crossref] [PubMed]
- Nuyt AM, Lavoie JC, Mohamed I, et al. Adult Consequences of Extremely Preterm Birth: Cardiovascular and Metabolic Diseases Risk Factors, Mechanisms, and Prevention Avenues. Clin Perinatol 2017;44:315-32. [Crossref] [PubMed]
- Mercanti I, Boubred F, Simeoni U. Therapeutic closure of the ductus arteriosus: benefits and limitations. J Matern Fetal Neonatal Med 2009;22:14-20. [Crossref] [PubMed]
- Warner BB, Tarr PI. Necrotizing enterocolitis and preterm infant gut bacteria. Semin Fetal Neonatal Med 2016;21:394-9. [Crossref] [PubMed]
- Cataldi L, Leone R, Moretti U, et al. Potential risk factors for the development of acute renal failure in preterm newborn infants: a case-control study. Arch Dis Child Fetal Neonatal Ed 2005;90:F514-9. [Crossref] [PubMed]
- Clark SM, Ghulmiyyah LM, Hankins GD. Antenatal antecedents and the impact of obstetric care in the etiology of cerebral palsy. Clin Obstet Gynecol 2008;51:775-86. [Crossref] [PubMed]
- Lastrucci V, Puglia M, Pacifici M, et al. Delayed Start of Routine Vaccination in Preterm and Small-for-Gestational-Age Infants: An Area-Based Cohort Study from the Tuscany Region, Italy. Vaccines (Basel) 2022;10:1414. [Crossref] [PubMed]
- Renolleau C, Toumazi A, Bourmaud A, et al. Association between Baseline Cortisol Serum Concentrations and the Effect of Prophylactic Hydrocortisone in Extremely Preterm Infants. J Pediatr 2021;234:65-70.e3. [Crossref] [PubMed]
- Luo NX, Jiang SY, Cao SJ, et al. Outcomes at discharge of preterm infants born <34 weeks' gestation. Zhonghua Er Ke Za Zhi 2022;60:774-80. [PubMed]
- Liu X, Liu LJ, Jiang HY, et al. Establishment of a nomogram model for predicting necrotizing enterocolitis in very preterm infants. Zhongguo Dang Dai Er Ke Za Zhi 2022;24:778-85. [PubMed]
- Wedgwood S, Steinhorn RH, Lakshminrusimha S. Optimal oxygenation and role of free radicals in PPHN. Free Radic Biol Med 2019;142:97-106. [Crossref] [PubMed]
- Tsai ML, Lien R, Chiang MC, et al. Prevalence and morbidity of late preterm infants: current status in a medical center of Northern Taiwan. Pediatr Neonatol 2012;53:171-7. [Crossref] [PubMed]
(English Language Editor: J. Jones)




