
Eclampsia, in vitro fertilization and the risk of preterm birth: a retrospective cohort study based on 2,880,759 samples
Highlight box
Key findings
• There exists a synergistic interaction effect of eclampsia and IVF on preterm birth.
What is known and what is new?
• Eclampsia and IVF were associated with an increased risk of preterm birth.
• The coexistence of eclampsia and IVF increased the risk of preterm birth.
What is the implication, and what should change now?
• Women with infertility treated with IVF may need to counsel and assess their potential eclampsia risk before starting IVF, as well as close supervision during pregnancy, timely identification and active intervention of eclampsia development.
Introduction
Preterm birth is defined as delivery at less than 37 completed weeks or 259 days of gestation; it has become one of the most important obstetric issues and is the main cause of perinatal morbidity and mortality (1). In addition, preterm birth is associated with increased health care costs (2). Consequently, it is necessary and important to focus on risk factors for preterm birth to reduce the public health burden.
Extensive evidence has shown that the risk of preterm birth is associated with maternal health (3,4). In recent years, in vitro fertilization (IVF) has emerged as a successful treatment for infertility, thus providing benefits for many couples (5). However, it is worth noting that a number of studies have noted that the preterm birth rate of newborns conceived through IVF increased significantly compared with those conceived naturally, which is one of the reasons for the high rate of preterm birth (6,7). A meta-analysis showed that the risk of preterm birth <37 weeks in singleton pregnancies achieved after IVF/ intra-cytoplasmic sperm injection (ICSI) was significantly greater than that occurring in spontaneous conception. This is due to a multifactorial iatrogenic etiology in which placental diseases are included (of which preeclampsia and eclampsia are major components) (8). Gui et al. pointed out that IVF is not only associated with an increased risk of preeclampsia (PE) but is also associated with the progression of PE (9). Moreover, Wang et al. reported that IVF was associated with the development of PE and eclampsia (10). Several studies have stated that PE or eclampsia was a common complication of pregnancy and a cause of maternal morbidity and mortality, which were considered to be independent risk factors for preterm birth (11,12). It seems that there may be pathways between IVF and eclampsia that have a common effect on the risk of preterm birth, which may substantially increase the risk of preterm birth in IVF participants with eclampsia (13). Nevertheless, to the best of our knowledge, few studies have focused on the relationship between IVF and eclampsia on the risk of preterm birth.
Understanding the combined effects of multiple risk factors for preterm birth is critical to making accurate and personalized risk predictions. Herein, the aim of our work was to explore the effect of the interaction between eclampsia and IVF on the risk of preterm birth. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-234/rc).
Methods
Data population
In this retrospective cohort study, all information was collected from the National Vital Statistics System (NVSS) database. In the United States, state law requires that all births fill out birth certificates, and federal law mandates the collection and release of birth data nationwide; then, the federation compiles these data in NVSS (14). Therefore, NVSS contains the most complete birth data, thus serving as a successful example of data sharing between governments in the field of public health (14). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
A total of 3,757,582 participants from 2019 were extracted from the Birth Data Files in the NVSS database 2019. The exclusion criteria were as follows: (I) mothers under the age of 18 years; (II) participants with missing information on preterm birth, IVF and eclampsia, newborn data, parental age, race or education level. All eligible participants were divided into a non-preterm birth group and a preterm birth group based on whether preterm birth occurred. The data of this study were desensitized and downloaded from a publicly available database, which did not require ethical review of Changzhou No.2 People’s Hospital, The Affiliated Hospital of Nanjing Medical University.
Outcome
The main outcome of this study was the occurrence of preterm birth. Preterm birth was defined as <37 weeks gestation (1). IVF is considered an assisted reproductive technology (ART). Eclampsia is a kind of generalized tonic-clonic convulsion in pregnant women that mostly occurs in women with established gestational hypertension or preeclampsia.
Data collection
Our study collected data from mothers, fathers and newborns separately; mothers’ information included age, race, education level, prepregnancy body mass index (BMI, kg/m2), gestational weight gain (GWG), smoking status before pregnancy, smoking status during pregnancy, history of prepregnancy diabetes, history of prepregnancy hypertension, history of cesarean section, history of preterm birth, number of fetuses, gestational hypertension (GH), gestational diabetes mellitus (GDM), pregnancy infections, IVF and eclampsia; fathers’ information contained age, race, and education level; and newborns’ information incorporated gender and preterm birth.
Statistical analysis
In our study, categorical and rank data were described by the number of cases and composition ratio N (%). The comparison between groups was performed by the chi-square test for categorical data, and the Mann-Whitney U rank sum test was used for comparison between the two groups for rank data.
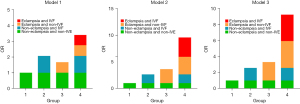
First, univariate logistic regression was conducted to analyze differences, and then the variables that were significant in univariate analysis along with eclampsia and IVF were included in multivariate logistic regression analysis to investigate whether eclampsia and IVF were statistically related to preterm birth. Three models were used in this study. Model 1 was unadjusted. Model 2 was adjusted for mothers’ age, mothers’ race, mothers’ education level, fathers’ age, fathers’ race, and fathers’ education level. Model 3 was adjusted for mothers’ information (age, race, education level, prepregnancy BMI, GWG, smoking status before pregnancy, smoking status during pregnancy, history of prepregnancy diabetes, history of prepregnancy hypertension, history of cesarean section, number of fetuses, GH, GDM, pregnancy infections), fathers’ information (age, race, education level) and newborns’ information (gender).
In addition, we constructed interaction terms between IVF and eclampsia to assess the effect of the coexistence of IVF and eclampsia on the risk of preterm birth: non-eclampsia and non-IVF, non-eclampsia and IVF, eclampsia and non-IVF, and eclampsia and IVF. Relative excess risk due to interaction (RERI), attributable proportion (AP) or synergy index (S) were used to assess the additive interaction between eclampsia and IVF on the risk of preterm birth; when the 95% confidence intervals (CI) of RERI or AP did not include 0 or the 95% CI of S did not include 1 (15), the interaction was regarded as statistically significant. Samples with missing information were excluded. All statistical tests were two-sided, and P<0.05 was considered to indicate statistical significance. SAS 9.4 statistical analysis software was used to complete univariate and multivariate logistic regression analyses, and R 4.20 software was used to draw the interaction diagram.
Results
Baseline characteristics
After excluding participants with missing information of preterm birth, IVF and eclampsia (n=9,337), newborn information (n=2,700) and parental age, race, education level (n=821,894) and participants with mothers <18 years old (n=42,892), a total of 2,880,759 eligible samples were eventually enrolled in this study, and all participants were divided into a non-preterm birth group (n=2,561,072) and a preterm birth group (n=319,687). The flow chart of the study population is presented in Figure 1. The incidence of preterm birth was approximately 11.10%. Table 1 summarizes the characteristics of the 2,880,759 samples and compares the features between the control group and preterm birth group. The percentages of mothers who had a history of prepregnancy diabetes, prepregnancy hypertension, cesarean section, preterm birth, GH, GDM, pregnancy infections, eclampsia and IVF were 0.93%, 2.13%, 15.58%, 3.37%, 7.76%, 7.11%, 1.95%, 0.27%, and 1.47%, respectively. Additionally, we also found that the age of mothers and fathers, the number of multiple births, the proportion of mothers with a history of preterm birth, GH, GDM, pregnancy infections, eclampsia and IVF among the preterm birth group were all higher than those among the non-preterm birth group. The variables in Table 1 were significantly different between the preterm birth and control groups (P<0.001). The detailed baseline data are shown in Table 1.
Table 1
| Variables | Total (n=2,880,759) | Non-preterm birth group (n=2,561,072) | Preterm birth group (n=319,687) | Statistics | P |
|---|---|---|---|---|---|
| Mother information | |||||
| Age, years, n (%) | Z=35.729 | <0.001 | |||
| <20 | 78,795 (1.00) | 69,118 (0.88) | 9,677 (0.12) | ||
| 20–29 | 1,331,917 (1.00) | 1,191,087 (0.89) | 140,830 (0.11) | ||
| 30–34 | 901,071 (1.00) | 806,764 (0.90) | 94,307 (0.10) | ||
| ≥35 | 568,976 (1.00) | 494,103 (0.87) | 74,873 (0.13) | ||
| Race, n (%) | χ2=11226.02 | <0.001 | |||
| White (only) | 2,177,278 (1.00) | 1,953,185 (0.90) | 224,093 (0.10) | ||
| Black (only) | 376,280 (1.00) | 315,899 (0.84) | 60,381 (0.16) | ||
| ALAN (only) | 22,654 (1.00) | 19,775 (0.87) | 2,879 (0.13) | ||
| Asian (only) | 221,018 (1.00) | 198,773 (0.90) | 22,245 (0.10) | ||
| NHOPI (only) | 8,022 (1.00) | 6,825 (0.85) | 1,197 (0.15) | ||
| More than one race | 75,507 (1.00) | 66,615 (0.88) | 8,892 (0.12) | ||
| Education level, n (%) | Z=−64.480 | <0.001 | |||
| 8th grade or less | 64,265 (1.00) | 56,188 (0.87) | 8,077 (0.13) | ||
| 9th through 12th grade | 854,787 (1.00) | 745,625 (0.87) | 109,162 (0.13) | ||
| Undergraduate | 1,531,233 (1.00) | 1,369,149 (0.89) | 162,084 (0.11) | ||
| Postgraduate | 430,474 (1.00) | 390,110 (0.91) | 40,364 (0.09) | ||
| Prepregnancy BMI, kg/m2, n (%) | Z=61.946 | <0.001 | |||
| Underweight <18.5 | 83,979 (1.00) | 73,812 (0.88) | 10,167 (0.12) | ||
| Normal 18.5–24.9 | 1,216,278 (1.00) | 1,095,526 (0.90) | 120,752 (0.10) | ||
| Overweight 25.0–29.9 | 773,442 (1.00) | 689,130 (0.89) | 84,312 (0.11) | ||
| Obesity I 35.0–34.9 | 438,775 (1.00) | 385,170 (0.88) | 53,605 (0.12) | ||
| Obesity II 35.0–39.9 | 216,621 (1.00) | 188,133 (0.87) | 28,488 (0.13) | ||
| Obesity III >40.0 | 151,664 (1.00) | 129,301 (0.85) | 22,363 (0.15) | ||
| GWG, pounds, n (%) | Z=−100.426 | <0.001 | |||
| Less than 11 pounds | 263,216 (1.00) | 221,567 (0.84) | 41,649 (0.16) | ||
| 11 to 20 pounds | 497,366 (1.00) | 428,616 (0.86) | 68,750 (0.14) | ||
| 21 to 30 pounds | 830,196 (1.00) | 742,293 (0.89) | 87,903 (0.11) | ||
| 31to 40 pounds | 711,294 (1.00) | 647,052 (0.91) | 64,242 (0.09) | ||
| 41 to 98 pounds | 578,687 (1.00) | 521,544 (0.90) | 57,143 (0.10) | ||
| Smoking status before pregnancy, n (%) | 186,527 (1.00) | 160,523 (0.86) | 26,004 (0.14) | χ2=1634.884 | <0.001 |
| Smoking status during pregnancy, n (%) | 148,846 (1.00) | 117,548 (0.79) | 31,298 (0.21) | χ2=15686.42 | <0.001 |
| Prepregnancy diabetes, n (%) | 26,738 (1.00) | 19,750 (0.74) | 6,988 (0.26) | χ2=6186.039 | <0.001 |
| Prepregnancy hypertension, n (%) | 61,294 (1.00) | 46,721 (0.76) | 14,573 (0.24) | χ2=10203.38 | <0.001 |
| History of cesarean section, n (%) | 448,740 (1.00) | 388,593 (0.87) | 60,147 (0.13) | χ2=2865.498 | <0.001 |
| History of preterm birth, n (%) | 97,109 (1.00) | 69,069 (0.71) | 28,040 (0.29) | χ2=32192.73 | <0.001 |
| Number of fetuses, n (%) | χ2=215350.6 | <0.001 | |||
| Single birth | 2,785,970 (1.00) | 2,520,934 (0.90) | 265,036 (0.10) | ||
| Multiple births | 94,789 (1.00) | 40,138 (0.42) | 54,651 (0.58) | ||
| GH, n (%) | 223,679 (1.00) | 172,962 (0.77) | 50,717 (0.23) | χ2=32943.03 | <0.001 |
| GDM, n (%) | 204,836 (1.00) | 174,841 (0.85) | 29,995 (0.15) | χ2=2810.668 | <0.001 |
| Pregnancy infections, n (%) | 56,284 (1.00) | 48,220 (0.86) | 8,064 (0.14) | χ2=607.061 | <0.001 |
| Eclampsia, n (%) | 7,653 (1.00) | 4,798 (0.63) | 2,855 (0.37) | χ2=5342.349 | <0.001 |
| IVF, n (%) | 42,394 (1.00) | 32,659 (0.77) | 9,735 (0.23) | χ2=6140.545 | <0.001 |
| Father information | |||||
| Age, years, n (%) | Z=21.142 | <0.001 | |||
| <20 | 37,795 (1.00) | 33,093 (0.88) | 4,702 (0.12) | ||
| 20–29 | 1,025,582 (1.00) | 913,833 (0.89) | 111,749 (0.11) | ||
| 30–34 | 874,399 (1.00) | 784,221 (0.90) | 90,178 (0.10) | ||
| ≥35 | 942,983 (1.00) | 829,925 (0.88) | 113,058 (0.12) | ||
| Race, n (%) | χ2=10026.25 | <0.001 | |||
| White (only) | 2,138,536 (1.00) | 1,917,858 (0.90) | 220,678 (0.10) | ||
| Black (only) | 439,125 (1.00) | 371,600 (0.85) | 67,525 (0.15) | ||
| AIAN (only) | 21,968 (1.00) | 19,120 (0.87) | 2,848 (0.13) | ||
| Asian (only) | 198,651 (1.00) | 179,423 (0.90) | 19,228 (0.10) | ||
| NHOPI (only) | 8,999 (1.00) | 7,737 (0.86) | 1,262 (0.14) | ||
| More than one race | 73,480 (1.00) | 65,334 (0.89) | 8,146 (0.11) | ||
| Education level, n (%) | Z=−73.939 | <0.001 | |||
| 8th grade or less | 78,395 (1.00) | 68,573 (0.87) | 9,822 (0.13) | ||
| 9th through 12th grade | 1,083,687 (1.00) | 945,980 (0.87) | 137,707 (0.13) | ||
| Undergraduate | 1,372,078 (1.00) | 1,230,777 (0.90) | 141,301 (0.10) | ||
| Postgraduate | 346,599 (1.00) | 315,742 (0.91) | 30,857 (0.09) | ||
| Newborn information | |||||
| Gender, n (%) | χ2=572.221 | <0.001 | |||
| Female | 1,405,055 (1.00) | 1,255,506 (0.89) | 149,549 (0.11) | ||
| Male | 1,475,704 (1.00) | 1,305,566 (0.88) | 170,138 (0.12) |
χ2, Chi-square test; Z, Mann-Whitney U rank sum test; BMI, body mass index; GWG, gestational weight gain; GH, gestational hypertension; GDM, gestational diabetes mellitus; IVF, in vitro fertilization; AIAN, American Indian/Alaskan Native; NHOPI, Native Hawaiian and Other Pacific Islanders.
The effect of eclampsia or IVF on the risk of preterm birth
The relationship between eclampsia or IVF and the risk of preterm birth is displayed in Table 2. Table 2 shows that the risk of preterm birth in women with eclampsia is 4.804 times, 4.601 times and 4.278 times higher than that in women without eclampsia [Model 1: odds ratio (OR) =4.804, 95% CI: 4.586–5.032; Model 2: OR =4.601, 95% CI: 4.390–4.823, Model 3: OR =4.278, 95% CI: 4.075–4.492]. Similarly, the association of IVF and the risk of preterm birth is also shown in Table 2. Model 1 (OR =2.432, 95% CI: 2.377–2.488) indicated that women who received IVF had a higher risk of preterm birth than women who did not receive IVF, which was in accordance with the results of Model 2 (OR =2.607, 95% CI: 2.547–2.669) and Model 3 (OR =2.531, 95% CI: 2.471–2.593).
Table 2
| Variables | Model 1 | Model 2 | Model 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||
| Eclampsia | |||||||||||
| No | Ref | Ref | Ref | ||||||||
| Yes | 4.804 | 4.586–5.032 | <0.001 | 4.601 | 4.390–4.823 | <0.001 | 4.278 | 4.075–4.492 | <0.001 | ||
| IVF | |||||||||||
| No | Ref | Ref | Ref | ||||||||
| Yes | 2.432 | 2.377–2.488 | <0.001 | 2.607 | 2.547–2.669 | <0.001 | 2.531 | 2.471–2.593 | <0.001 | ||
Model 1: unadjusted; Model 2: adjusted for mothers’ age, mothers’ race, mothers’ education level, fathers’ age, fathers’ race, fathers’ education level; Model 3: adjusted for mothers’ information (age, race, education level, prepregnancy body mass index, gestational weight gain, smoking status before pregnancy, smoking status during pregnancy, history of prepregnancy diabetes, history of prepregnancy hypertension, history of cesarean section, number of fetuses, gestational hypertension, gestational diabetes mellitus, pregnancy infections), fathers’ information (age, race, education level) and newborns’ information (gender). IVF, in vitro fertilization; OR, odds ratio; CI, confidence interval.
The interaction of eclampsia and IVF on the risk of preterm birth
Table 2 shows that eclampsia and IVF increased the risk of preterm birth. After constructing the interaction terms between IVF and eclampsia, we adopted RERI, AP and S to estimate whether IVF and eclampsia interact to increase the risk of preterm birth. As shown in Tables 3,4, RERIModel 3 =3.426 (95% CI: 0.639–6.213), APModel 3 =0.374 (95% CI: 0.182–0.565), and SModel 3 =1.723 (95% CI: 1.222–2.428) after adjusting for variables, which indicated that the interaction between eclampsia and IVF on preterm birth was statistically significant, thus indicating a synergistic interaction. Furthermore, APModel 3 =0.374, indicating that 37.4% of preterm births in our study were attributable to the synergistic interaction of eclampsia and IVF. A schematic diagram of the interaction between eclampsia and IVF is shown in Figure 2.
Table 3
| Eclampsia | IVF | Sample size (n) | Model 1 | Model 2 | Model 3 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | |||||
| No | No | 2,830,893 | Ref | Ref | Ref | ||||||||
| No | Yes | 42,213 | 2.431 | 2.376–2.488 | <0.001 | 2.611 | 2.550–2.673 | <0.001 | 2.534 | 2.473–2.596 | <0.001 | ||
| Yes | No | 7,472 | 4.812 | 4.591–5.044 | <0.001 | 4.626 | 4.411–4.852 | <0.001 | 4.293 | 4.087–4.510 | <0.001 | ||
| Yes | Yes | 181 | 9.082 | 6.784–12.159 | <0.001 | 9.547 | 7.115–12.811 | <0.001 | 9.197 | 6.795–12.448 | <0.001 | ||
Model 1: unadjusted; Model 2: adjusted for mothers’ age, mothers’ race, mothers’ education level, fathers’ age, fathers’ race, fathers’ education level; Model 3: adjusted for mothers’ information (age, race, education level, prepregnancy body mass index, gestational weight gain, smoking status before pregnancy, smoking status during pregnancy, history of prepregnancy diabetes, history of prepregnancy hypertension, history of cesarean section, the number of fetuses, gestational hypertension, gestational diabetes mellitus, pregnancy infections), fathers’ information (age, race, education level) and newborns’ information (gender). IVF, in vitro fertilization; OR, odds ratio; CI, confidence interval.
Table 4
| Indicators | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| RERI (95% CI) | 2.832 (0.174–5.489) | 3.311 (0.495–6.127) | 3.426 (0.639–6.213) |
| AP (95% CI) | 0.312 (0.110–0.514) | 0.347 (0.153–0.540) | 0.374 (0.182–0.565) |
| S (95% CI) | 1.540 (1.106–2.144) | 1.632 (1.172–2.273) | 1.723 (1.222–2.428) |
Model 1: unadjusted; Model 2: adjusted for mothers’ age, mothers’ race, mothers’ education level, fathers’ age, fathers’ race, fathers’ education level; Model 3: adjusted for mothers’ information (age, race, education level, prepregnancy body mass index, gestational weight gain, smoking status before pregnancy, smoking status during pregnancy, history of prepregnancy diabetes, history of prepregnancy hypertension, history of cesarean section, the number of fetuses, gestational hypertension, gestational diabetes mellitus, pregnancy infections), fathers’ information (age, race, education level) and newborns’ information (gender). RERI, relative excess risk due to interaction; AP, attributable proportion; S, synergy index; OR, odds ratio; CI, confidence interval.
Discussion
Currently, with the increasing popularity of ART, IVF has become an important treatment for infertility worldwide (16). A number of studies have shown that compared with naturally conceived newborns, the premature birth rate of newborns conceived by IVF has increased significantly, which is a serious threat and is associated with short- and long-term adverse consequences (6,7,17). IVF has also been demonstrated to be associated with an increased risk of eclampsia, and IVF and eclampsia may jointly influence the risk of preterm birth. Therefore, in this study, we investigated the interaction of IVF and eclampsia on the risk of preterm birth. The findings showed that eclampsia and IVF were associated with an increased risk of preterm birth. More importantly, the coexistence of eclampsia and IVF accelerated the development and progression of preterm birth. In other words, the combination of eclampsia and IVF was not only a simple additive effect but also a synergistic interaction, leading to a higher risk of preterm birth. Our results may provide a reference to indicate that antenatal care for IVF pregnant women with preeclampsia should be emphasized and that obstetricians should try to prevent the development of eclampsia, especially in an IVF pregnancy.
Consistent with the results of previous studies, eclampsia and IVF were the potential risk factors for preterm birth (17,18). von Wolff et al. reported that the risk of preterm birth was 1.7 times higher for IVF singleton pregnancies than for non-IVF pregnancies (17). It is worth mentioning that Okby et al. (13) reported the risk factors and pregnancy outcome of natural fertilization and IVF twins with preeclampsia in 2018 based on 3,518 twin pregnancies; they found that IVF twins with PE had a higher risk of cesarean delivery, preterm delivery and low birth weight than natural fertilization twins, but the sample size of this study was not very large and did not control covariates, which may have skewed the results (13). Compared with the study of Okby et al. (13), our study based on 2,880,759 samples showed that after adjusting for some variables, IVF pregnant women with eclampsia had a higher risk of preterm delivery, and this result may be even more convincing.
Additionally, this study indicated that there was a synergistic interaction between eclampsia and IVF on the risk of preterm birth. A meta-analysis showed that women undergoing IVF had a higher incidence of pregnancy-related complications, including pregnancy-induced hypertension, GDM, polyhydramnios, and placenta previa, than women who had a natural pregnancy (19). The increased incidence of various pregnancy complications following IVF pregnancy may increase the risk of preterm birth in pregnant women with eclampsia. The age of women with infertility requiring IVF treatment was higher, and the underlying diseases associated with infertility (tubal inflammation, uterine malformation, immune infertility) might also trigger the risk of preterm birth in pregnant women with eclampsia during pregnancy (20,21). In vitro culture of embryos during IVF treatment may change the gene expression of trophoblast cells, expose nourishing cells to specific environments and affect placental function, thereby increasing the risk of eclampsia and promoting the development of preterm birth (22,23). Several studies have noted that IVF was more likely to trigger multiple pregnancies, which was one reason for the higher rate of preterm birth for newborns (24,25); similarly, the increased multiple pregnancy rate may also play a critical role in the higher risk of preterm birth among IVF pregnant women with eclampsia. Placental hypoperfusion induced by impaired placental vascular development and endothelial dysfunction may be the mechanism associated with preterm birth in eclampsia (26). A study has shown that IVF can also cause vascular dysfunction (27). At present, the mechanism by which the combined effect of IVF and eclampsia affects the risk of preterm birth remains unclear, and further studies are needed. Overall, the findings highlighted that women with infertility receiving IVF may need to actively intervene in eclampsia development, such as prenatal screening, regular prenatal check-ups, and monitoring changes in blood pressure (28-32).
The advantages of our study should be presented. First, our study had a large sample size and contained more comprehensive factors associated with preterm birth, drawing a more credible conclusion. Second, we found that the combination of eclampsia and IVF was a kind of synergistic interaction, which brought a higher risk of preterm birth. Nevertheless, the study also has some limitations. First, the NVSS database did not have information about the causes of infertility (33), placental abnormalities (34), polyhydramnios (35), and the type of IVF (36-38), which might be important for studying the risk of preterm birth (35-37). Second, although we excluded some participants who lacked information on preterm birth, IVF, eclampsia, newborn data, mothers, and fathers in the NVSS database, we were not sure whether these missing cases affected the results of this study. Third, we assessed the interaction between IVF and eclampsia on the risk of preterm birth and did not consider the effect of IVF and other pregnancy complications on preterm infants.
Moreover, the study recruited participants from the NVSS database, which lacked records of preeclampsia. Fourth, since all participants included in this study were from the United States, our results may not be generalizable to other countries. Last, this is a retrospective cohort study, which may have selection bias and recall bias. More prospective studies are needed to explore the interaction of eclampsia and IVF on the risk of preterm birth in the future.
Conclusions
Eclampsia and IVF might have a synergistic interaction on the development and process of preterm birth. Awareness of the risk profile associated with preterm birth is crucial for pregnant woman with infertility treated with IVF to implement dietary and lifestyle modifications.
Acknowledgments
Funding: This research was supported by the Changzhou Sci & Tech Program (Grant No. CJ20210086).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-234/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-234/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-234/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Esposito G, Mauri PA, Cipriani S, et al. The role of maternal age on the risk of preterm birth among singletons and multiples: a retrospective cohort study in Lombardy, Norther Italy. BMC Pregnancy Childbirth 2022;22:234. [Crossref] [PubMed]
- Achana F, Johnson S, Ni Y, et al. Economic costs and health utility values associated with extremely preterm birth: Evidence from the EPICure2 cohort study. Paediatr Perinat Epidemiol 2022;36:696-705. [Crossref] [PubMed]
- Gurol-Urganci I, Jardine JE, Carroll F, et al. Maternal and perinatal outcomes of pregnant women with SARS-CoV-2 infection at the time of birth in England: national cohort study. Am J Obstet Gynecol 2021;225:522.e1-522.e11. [Crossref] [PubMed]
- Blitz MJ, Gerber RP, Gulersen M, et al. Preterm birth among women with and without severe acute respiratory syndrome coronavirus 2 infection. Acta Obstet Gynecol Scand 2021;100:2253-9. [Crossref] [PubMed]
- von Schondorf-Gleicher A, Mochizuki L, Orvieto R, et al. Revisiting selected ethical aspects of current clinical in vitro fertilization (IVF) practice. J Assist Reprod Genet 2022;39:591-604. [Crossref] [PubMed]
- Yu H, Liang Z, Cai R, et al. Association of adverse birth outcomes with in vitro fertilization after controlling infertility factors based on a singleton live birth cohort. Sci Rep 2022;12:4528. [Crossref] [PubMed]
- Sanders JN, Simonsen SE, Porucznik CA, et al. Fertility treatments and the risk of preterm birth among women with subfertility: a linked-data retrospective cohort study. Reprod Health 2022;19:83. [Crossref] [PubMed]
- Cavoretto PI, Giorgione V, Sotiriadis A, et al. IVF/ICSI treatment and the risk of iatrogenic preterm birth in singleton pregnancies: systematic review and meta-analysis of cohort studies. J Matern Fetal Neonatal Med 2022;35:1987-96. [Crossref] [PubMed]
- Gui J, Ling Z, Hou X, et al. In vitro fertilization is associated with the onset and progression of preeclampsia. Placenta 2020;89:50-7. [Crossref] [PubMed]
- Wang Y, Shi H, Chen L, et al. Absolute Risk of Adverse Obstetric Outcomes Among Twin Pregnancies After In Vitro Fertilization by Maternal Age. JAMA Netw Open 2021;4:e2123634. [Crossref] [PubMed]
- Das S, Das R, Bajracharya R, et al. Incidence and Risk Factors of Pre-Eclampsia in the Paropakar Maternity and Women's Hospital, Nepal: A Retrospective Study. Int J Environ Res Public Health 2019;16:3571. [Crossref] [PubMed]
- Shen M, Smith GN, Rodger M, et al. Comparison of risk factors and outcomes of gestational hypertension and pre-eclampsia. PLoS One 2017;12:e0175914. [Crossref] [PubMed]
- Okby R, Harlev A, Sacks KN, et al. Preeclampsia acts differently in in vitro fertilization versus spontaneous twins. Arch Gynecol Obstet 2018;297:653-8. [Crossref] [PubMed]
- GBD US Health Disparities Collaborators. Life expectancy by county, race, and ethnicity in the USA, 2000-19: a systematic analysis of health disparities. Lancet 2022;400:25-38. [Crossref] [PubMed]
- Shi W, Wang H, Zhou Y, et al. Synergistic interaction of hyperuricemia and hypertension on reduced eGFR: insights from a general Chinese population. Postgrad Med 2020;132:263-9. [Crossref] [PubMed]
- Li Q, Zhao L, Zhou L, et al. Effect Analysis of Degranulated Cell in Early Fertilization on FET Outcome and Offspring Safety with Data Mining. Comput Math Methods Med 2022;2022:4955287. [Crossref] [PubMed]
- von Wolff M, Haaf T. In Vitro Fertilization Technology and Child Health. Dtsch Arztebl Int 2020;117:23-30. [Crossref] [PubMed]
- Rugumisa BT, Bongcam-Rudloff E, Lukumay MS, et al. Factors associated with risk of preterm delivery in Tanzania: A case-control study at Muhimbili National Hospital. Int J Gynaecol Obstet 2021;154:318-23. [Crossref] [PubMed]
- Qin J, Liu X, Sheng X, et al. Assisted reproductive technology and the risk of pregnancy-related complications and adverse pregnancy outcomes in singleton pregnancies: a meta-analysis of cohort studies. Fertil Steril 2016;105:73-85.e1-6.
- Dunietz GL, Holzman C, Zhang Y, et al. Assisted reproduction and risk of preterm birth in singletons by infertility diagnoses and treatment modalities: a population-based study. J Assist Reprod Genet 2017;34:1529-35. [Crossref] [PubMed]
- Savasi VM, Mandia L, Laoreti A, et al. Maternal and fetal outcomes in oocyte donation pregnancies. Hum Reprod Update 2016;22:620-33. [Crossref] [PubMed]
- Cavoretto P, Dallagiovanna C, Viganò P, et al. First trimester combined screening test in pregnancies derived from blastocyst transfer. Eur J Obstet Gynecol Reprod Biol 2016;198:50-5. [Crossref] [PubMed]
- von Versen-Höynck F, Narasimhan P, Selamet Tierney ES, et al. Absent or Excessive Corpus Luteum Number Is Associated With Altered Maternal Vascular Health in Early Pregnancy. Hypertension 2019;73:680-90. [Crossref] [PubMed]
- Lin D, Li P, Fan D, et al. Association between IVF/ICSI treatment and preterm birth and major perinatal outcomes among dichorionic-diamnionic twin pregnancies: A seven-year retrospective cohort study. Acta Obstet Gynecol Scand 2021;100:162-9. [Crossref] [PubMed]
- Sullivan-Pyke CS, Senapati S, Mainigi MA, et al. In Vitro fertilization and adverse obstetric and perinatal outcomes. Semin Perinatol 2017;41:345-53. [Crossref] [PubMed]
- An H, Jin M, Li Z, et al. Impact of gestational hypertension and pre-eclampsia on preterm birth in China: a large prospective cohort study. BMJ Open 2022;12:e058068. [Crossref] [PubMed]
- Rexhaj E, Paoloni-Giacobino A, Rimoldi SF, et al. Mice generated by in vitro fertilization exhibit vascular dysfunction and shortened life span. J Clin Invest 2013;123:5052-60. [Crossref] [PubMed]
- Xu W, Ru P, Gu Z, et al. Comprehensive Analysis of Differently Expressed and Methylated Genes in Preeclampsia. Comput Math Methods Med 2020;2020:2139270. [Crossref] [PubMed]
- Zhu X, Huang C, Wu L, et al. Perinatal Outcomes and Related Risk Factors of Single vs Twin Pregnancy Complicated by Gestational Diabetes Mellitus: Meta-Analysis. Comput Math Methods Med 2022;2022:3557890. [Crossref] [PubMed]
- Chung EH, Lim SL, Havrilesky LJ, et al. Cost-effectiveness of prenatal screening methods for congenital heart defects in pregnancies conceived by in-vitro fertilization. Ultrasound Obstet Gynecol 2021;57:979-86. [Crossref] [PubMed]
- Murad NM. Ultrasound or ultrasound and hormonal determinations for in vitro fertilization monitoring. Int J Gynaecol Obstet 1998;63:271-6. [Crossref] [PubMed]
- Cnossen JS, Morris RK, ter Riet G, et al. Use of uterine artery Doppler ultrasonography to predict pre-eclampsia and intrauterine growth restriction: a systematic review and bivariable meta-analysis. CMAJ 2008;178:701-11. [Crossref] [PubMed]
- Sunkara SK, Antonisamy B, Redla AC, et al. Female causes of infertility are associated with higher risk of preterm birth and low birth weight: analysis of 117 401 singleton live births following IVF. Hum Reprod 2021;36:676-82. [Crossref] [PubMed]
- Zhang YJ, Shen J, Lin SB, et al. The risk factors of preterm birth: A multicentre case-control survey in China in 2018. J Paediatr Child Health 2022;58:1396-406. [Crossref] [PubMed]
- Huang J, Qian Y, Gao M, et al. Analysis of factors related to preterm birth: a retrospective study at Nanjing Maternity and Child Health Care Hospital in China. Medicine (Baltimore) 2020;99:e21172. [Crossref] [PubMed]
- Cavoretto PI, Farina A, Gaeta G, et al. Uterine artery Doppler in singleton pregnancies conceived after in-vitro fertilization or intracytoplasmic sperm injection with fresh vs frozen blastocyst transfer: longitudinal cohort study. Ultrasound Obstet Gynecol 2020;56:603-10. [Crossref] [PubMed]
- Wiegel RE, Karsten MJH, Reijnders IF, et al. Corpus luteum number and the maternal renin-angiotensin-aldosterone system as determinants of utero-placental (vascular) development: the Rotterdam Periconceptional Cohort. Reprod Biol Endocrinol 2021;19:164. [Crossref] [PubMed]
- Cavoretto PI, Farina A, Miglio R, et al. Prospective longitudinal cohort study of uterine arteries Doppler in singleton pregnancies obtained by IVF/ICSI with oocyte donation or natural conception. Hum Reprod 2020;35:2428-38. [Crossref] [PubMed]



