
Environmental tobacco smoke exposure and 24-h movement guidelines in Spanish young people
Highlight box
Key findings
• Environmental tobacco smoke exposure was associated with lower odds of meeting 24-h movement guidelines.
What is known and what is new?
• Environmental tobacco smoke exposure is one of the most important factors affecting the health of young people.
• Children are the most susceptible population to the harmful effects of environmental tobacco smoke exposure.
What is the implication, and what should change now?
• This is the first study examining the associations between exposure to secondhand smoke and the 24-h movement guidelines.
• Avoiding exposure to tobacco smoke in the environment is essential, as it can potentially influence the 24-h movement behaviors of young people, and consequently, the health benefits associated with such behaviors.
Introduction
Environmental tobacco smoke exposure, second-hand smoke, or passive smoking (i.e., the smoke to which nonsmokers are exposed when they are in an indoor environment with smokers) (1), is a preventable cause of disease and disability and a sizable public health problem. Children are at the highest risk of experiencing the negative consequences of being exposed to environmental tobacco smoke exposure (2). Passive exposure to tobacco smoke significantly contributes to mortality and morbidity among children (3). A previous systematic review and meta-analysis by Faber et al. (4) has shown that exposure to environmental tobacco smoke is linked to various adverse respiratory health outcomes in children, including respiratory tract infections, wheezing, and asthma. Furthermore, exposure to environmental tobacco smoke in children can result in an increased lifelong risk of poor lung health (5).
The 24-h movement guidelines for young people emphasize the integration of all behaviors across the 24-h time-use continuum rather than focusing on individual activity components. According to these guidelines, children who are under the age of five should participate in at least 180 min daily in different kinds of physical activity (PA), with a minimum of 60 min daily of moderate-to-vigorous intensity) and should avoid screen time. Children and adolescents between the ages of 5–17 should engage in at least 60 min per day of moderate-to-vigorous PA, limit their recreational screen time (ST) to no more than 1 h daily for children under 5 years old and a maximum of 2 h daily of for children and adolescents (aged 5–17 years), and get sufficient sleep, which means 10 to 13 h daily for children under 5 years old, 9 to 11 h for children, and 8 to 10 h for adolescents), during a 24-h period (6,7). Thus, the clustering and interactions among all 24-h movement guidelines should be targeted to increase health benefits (8-14). However, a recent systematic review and meta-analysis concluded that only 7.12% met the 24-h movement guidelines at the global level (15).
A handful of studies have, in an isolated manner, examined the association between environmental tobacco smoke exposure and 24-h movement behaviors (i.e., PA, recreational ST, and sleep duration) among young populations (16,17). For instance, Ebrahimi et al. (17) showed that lower PA and higher ST were notably related to passive smoking. A recent study by Mahabee-Gittens et al. (18) showed that children with tobacco smoke exposure had lower odds of adhering to a healthy lifestyle (e.g., higher PA, lower ST). Supporting this notion, another study conducted in the US reported that children who are exposed to tobacco smoke are less likely to participate in afterschool activities (19). Similarly, Merianos et al. (16) showed that children exposed to tobacco smoke had poorer sleep than children not exposed to tobacco smoke. Based on the above, an inverse relationship between passive smoking and 24-h movement behaviors could also be expected. However, no prior research has investigated how exposure to environmental tobacco smoke is related to the combination of 24-h movement behaviors among young populations thus far.
Additionally, previous studies have shown that 24-h movement behaviors could be related to smoking behavior among young people (20,21). For example, Grao-Cruces et al. (20) indicated that higher levels of PA (in boys) were associated with lower tobacco use. Similarly, smoking tobacco (among other factors) has been associated with decreased total sleep among adolescents (21). This is particularly concerning, as these behaviors are important for maintaining good health and preventing chronic diseases. On the other hand, based on the gap found in the scientific literature, this is the first study examining the associations between exposure to secondhand smoke and the 24-h movement guidelines. According to previous literature, we hypothesized that exposure to environmental tobacco smoke will be associated with lower odds of adherence to the 24-h movement guidelines in our study sample. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-93/rc).
Methods
Study design
This is a cross-sectional study using data from the last available wave [2017] of the Spanish National Health Survey (SNHS) (22), a nationally representative survey of the Spanish children and adult population. This survey was conducted by the Ministry of Health, Consumer Affairs and Social Welfare and the National Statistics Institute (23). The sampling framework involved noninstitutionalized Spanish individuals. The SNHS uses a three-stage sampling design: (I) first stage (census section); (II) second stage (households); and (III) third stage (individuals). Within each household, an adult (aged 15 or older) was selected to complete the Adult Questionnaire, and if there were minors in the households (from 0 to 14 years of age), one of them was also randomly selected to complete the Minors Questionnaire.
To achieve the aim of this study, only individuals from the ages of 0 to 14 years old were included in the sample (as indicated by the Minors Questionnaire). The original sample consisted of 6,106 participants (100%). A total of 1,728 participants (28.3%) were removed due to missing data in independent/dependent variables. Further information about the selection process of the sample is found in Figure S1. Thus, a total of 4,378 Spanish participants aged 2–14 years were analyzed (71.7%).
Data from the SHNS [2017] were anonymized and acquired from the Ministry of Health, Consumer Affairs and Social Welfare (22) (public access: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm). Since this study utilized secondary data, it did not require approval from an Ethics Committee. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Procedures
Environmental tobacco smoke exposure was ascertained through a single item question: “How often is your child exposed to indoor tobacco smoke?”; possible responses were: (I) “never or almost never”; (II) “less than 1 hour daily; (III) “from one to 5 hours daily”; (IV) “more than 5 hours daily”. This question has been used in previous studies (24,25). For analytical purposes, we collapsed these categories into (I) “no environmental tobacco smoke exposure” (“never or almost never”); or (II) “environmental tobacco smoke exposure” (“less than one hour daily”, “from one to 5 hours daily”, or “more than 5 hours daily”) (26).
A modified version of the International Physical Activity Questionnaire (27) was used to assess PA in the study sample. Participants had four possible responses: (I) “no exercise” [free-time mainly spent in sedentary activities (e.g., reading, watching TV)]; (II) “occasional sport, or PA participation”; (III) “PA several times per month”, and (IV) “physical training or sports several times per week” (22). Participants who responded, ‘no exercise’, ‘occasional sport, or PA participation’; or ‘PA several times per month’ were categorized into the not ‘meeting the PA guidelines’ group. Participants who responded, ‘physical training or sports several times per week’, were categorized into the ‘meeting the PA guidelines’ group. Recreational ST was assessed with a set of questions related to the duration of ST both on weekdays and weekends: “How much time does your child typically spend on weekdays/weekends in front of a screen, including a computer, tablet, TV, video, video game or cell phone screen?”. The possible responses were (I) “nothing or almost nothing”; (II) “less than 1 hour”; and (III) “1 hour or more”. If participants reported “one hour or more”, they were additionally asked about the exact number of hours they spent with ST. Meeting the recreational ST guidelines was based on the World Health Organization international guidelines on sedentary behavior for children under 5 years old (7) (under 1 year old: no ST; 1 to 4 years old: <1 h/day) and the Canadian ST guidelines for the young population (5 to 14 years old: less than 2 h/day of ST) (6). Participants were also asked about sleep duration: “Can you tell me approximately how many hours your child usually sleeps daily? (Including nap times)”. The prevalence of meeting the sleep duration guidelines was based on the National Sleep Foundation’s sleep duration guidelines (28): children under 5 years old (from 10 to 13 h/day of sleep); children aged 5–12 years (from 9 to 11 h/day of sleep); adolescents aged 13–14 years (from 8 to 10 h/day of sleep).
Information about the participants’ sex (boys or girls), age, immigrant status (based on nationality), and region was gathered from their parents or caregivers. The socioeconomic status of the participants was determined by classifying the responders’ occupation into one of six categories, ranging from “class 1” (the highest) to “class 6” (the lowest). Additionally, the parents or caregivers reported the participants’ weight and height, which were used to calculate their body mass index (BMI) by dividing weight (in kilograms) by height (in meters squared). The selection of these covariates was informed by prior scientific literature (16-18,29,30).
Statistical analysis
The mean and standard deviation were used to express continuous data, while absolute and relative frequencies were used to present categorical data. To check for normality, the Kolmogorov-Smirnov test and normal probability plot were used for the variables. Differences in continuous data between environmental tobacco smoke exposure and the study participants’ characteristics were assessed using Student’s t-test. For categorical data, we used the chi-square test. Preliminary analyses revealed no significant interactions between sex or age and 24-h movement guidelines in relation to environmental tobacco smoke exposure (P>0.05 for both). Thus, all analyses were conducted including both boys and girls. We conducted binary logistic regression analyses to examine the relationship between exposure to environmental tobacco smoke and meeting the 24-h movement guidelines. Some covariates (i.e., sex, age, socioeconomic status, immigrant status, region, and BMI) were included in the analyses. All statistical analyses were performed with STATA 17.0 (StataCorp, College Station, TX, USA), and P<0.050 denoted statistical significance.
Results
Descriptive data of the study participants are shown in Table 1. The prevalence of participants exposed to environmental tobacco smoke was 6.9%. Participants exposed to environmental tobacco smoke were older (9.8±3.5 years) than those not exposed (8.6±3.7 years) (P<0.001). A higher proportion of participants with the lowest SES (i.e., Class 6) was observed in participants with tobacco smoke exposure (23.0%) than in the group not exposed (11.5%) (P<0.001 for trend). The characteristics and differences between the included and excluded participants are shown in Table S1.
Table 1
| Variables | No tobacco smoke exposure (n=4,074; 93.1%) |
Tobacco smoke exposure (n=304; 6.9%) |
P |
|---|---|---|---|
| Age (years) | 8.6±3.7 | 9.8±3.5 | <0.001 |
| Age group | <0.001 | ||
| Children under 5 (2–4 years) | 1,024 (25.1) | 50 (16.4) | |
| Children (5–12 years) | 2,281 (56.0) | 169 (55.6) | |
| Adolescents (13–14 years) | 769 (18.9) | 85 (28.0) | |
| Sex | 0.917 | ||
| Boys | 2,078 (51.0) | 156 (51.3) | |
| Girls | 1,996 (49.0) | 148 (48.7) | |
| Immigrant status | 0.163 | ||
| Native | 3,879 (95.2) | 284 (93.4) | |
| Immigrant | 195 (4.8) | 20 (6.6) | |
| SES | <0.001 | ||
| Class 1 (the highest) | 584 (14.3) | 20 (6.6) | |
| Class 2 | 373 (9.2) | 11 (3.6) | |
| Class 3 | 836 (20.5) | 48 (15.8) | |
| Class 4 | 572 (14.0) | 39 (12.8) | |
| Class 5 | 1,241 (30.5) | 116 (38.2) | |
| Class 6 (the lowest) | 468 (11.5) | 70 (23.0) | |
| Anthropometric data | |||
| Weight (kg) | 34.3 (15.5) | 40.8 (17.5) | <0.001 |
| Height (cm) | 133.5 (24.5) | 141.5 (23.3) | <0.001 |
| BMI (kg/m2) | 18.3 (3.6) | 19.5 (4.6) | <0.001 |
Data are expressed as the mean ± standard deviation or absolute frequencies (relative frequencies). BMI, body mass index; SES, socioeconomic status.
Figure 1 shows the proportion of the young population meeting the 24-h movement guidelines according to environmental tobacco smoke exposure. Global adherence to all three 24-h movement guidelines was 7.3%. A lower prevalence of participants meeting both the ST and sleep duration guidelines was reported in young people exposed to environmental tobacco smoke (P<0.05 for all). In addition, the prevalence of meeting all three guidelines was lower in the young population exposed to environmental tobacco smoke (6.9%) than in those not exposed (12.5%) (P=0.004).

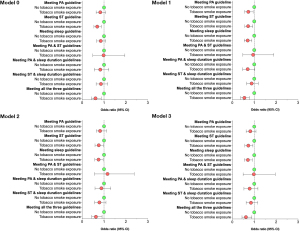
Figure 2 shows the association of environmental tobacco smoke exposure with meeting the 24-h movement guidelines. A lower likelihood of meeting ST and all three 24-h movement guidelines were found in those exposed to environmental tobacco smoke in unadjusted models. However, meeting ST [odds ratio (OR) =0.76; 95% confidence interval (CI), 0.59–0.97], sleep duration (OR =0.75; 95% CI, 0.58–0.96), and all three 24-h movement guidelines (OR =0.63; 95% CI, 0.44–0.91) reached significance after adjusting for potential confounders.
Discussion
We found that approximately one in ten participants were exposed to some form of secondhand smoke. This figure contrasts with higher global estimations of childhood environmental tobacco smoke exposure reported elsewhere (40% to 70%) (1,5,31). These differences may be due to the use of different methodologies to assess the exposure, which could have biased our results (5). Nonetheless, and as stated in Goal 3 of the United Nations Sustainable Development document (32), it seems reasonable to call for preventive public health actions to minimize children’s exposure to environmental tobacco smoke by advising parents not to smoke in the presence of their children.
We observed that tobacco smoke exposure was inversely associated with meeting some individual 24-h movement guidelines (e.g., ST or sleep guidelines). Previous studies have reported that passive smoking is related to higher ST (17,18,33). This finding could be (at least partially) justified by the fact that young people who spend more time at home after school also engage in more ST (34) and may be exposed for longer periods to tobacco smoke in smoking households. A previous study also found that children exposed to secondhand smoke had inadequate sleep (16). It is plausible that children exposed to tobacco smoke are more likely to have obstructive sleep apnea syndrome (35,36) or snoring-arousal indices (37), which could affect sleep duration and quality.
On the other hand, we did not detect an association between tobacco smoke exposure and PA. Previous studies have shown that children with tobacco smoke exposure have lower odds of being physically active (17,18). However, studies analyzing this association are scarce in the scientific literature. It has been reported that children from nonsmoking households seem to have higher awareness of the PA guidelines (38). This disparity reported in our study may be related to differences in the assessment of PA, and caution should be exercised when interpreting our results.
Another relevant finding from our study is that young people exposed to environmental smoking tobacco had a lower probability of meeting all three 24-h movement guidelines. This result agrees with the theoretical framework of the 24-h movement behaviors, which highlights the relevance of integrating all these behaviors since they cover the 24-h period, and a balance among them is needed for optimal health (13) at all ages (14). To the best of our knowledge, this is the first study examining the association between environmental tobacco smoke and 24-h movement guidelines among a young population, which is difficult to discuss with previous studies. Possible explanations justifying (at least in part) this finding could lie in the influence of environmental tobacco smoke exposure on the respiratory system. Tobacco smoke includes a great number of carcinogens and chemicals, which may negatively affect the developing respiratory system in children, increase susceptibility to allergic diseases during childhood (39), and cause the loss of lung function in this population (40). This fact could lead to a lower exercise capacity among this population (41), which could affect the rest of the movement behaviors synergistically (42). Supporting this idea, some studies have shown that children living in smoking households have lower cardiorespiratory fitness than their counterparts living in nonsmoking households (43,44). Thus, the hypothesis that environmental tobacco smoke exposure could have a detrimental effect on cardiorespiratory fitness and, therefore, be associated with lower meeting of the 24-h movement guidelines among young people appears to be likely. However, caution is required to interpret this hypothesis since other observational studies have also shown an opposite direction [i.e., meeting with all three 24-h movement guidelines and higher cardiorespiratory fitness in young people (8,14)]. Therefore, further studies are needed to clarify the direction of this association.
There are some limitations to this study. First, because of the cross-sectional design of this study, it is not possible to determine if the observed relationships represent cause-effect associations. Longitudinal studies are required to investigate how 24-h movement behaviors are associated with environmental tobacco smoke exposure. Second, we used self-report questionnaires, and consequently, we cannot confirm that the declared data are truthful. Likewise, there could be a possible recall bias. Third, body mass index and excess weight were determined through height and weight reported by the parents/caregivers for young people, which could involve measurement errors. In contrast, the main strength of this study is that, to date, it is the first study to examine the association between environmental tobacco smoke exposure 24-h movement guidelines among young people. In addition, this study benefited from a large and diverse sample of young individuals from various regions of Spain, which enhances the generalizability of the findings.
Conclusions
Given the inverse associations found, environmental tobacco smoke exposure should be a relevant factor to consider when promoting 24-h behaviors in the young population. This result is clinically significant, as environmental tobacco smoke exposure is one of the most important factors affecting the health of young people (2,3). Avoiding exposure to tobacco smoke in the environment is essential, as it can potentially influence the 24-h movement behaviors of young people, and consequently, the health benefits associated with such behaviors.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-93/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-93/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-93/coif). AGH serves as an unpaid editorial board member of Translational Pediatrics from August 2021 to July 2023. JFLG is a Margarita Salas Fellow (Universidad Pública de Navarra – 1225/2022). AGH is a Miguel Servet Fellow (Instituto de Salud Carlos III-FSE – CP18/0150). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Oberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 2011;377:139-46. [Crossref] [PubMed]
- Pugmire J, Sweeting H, Moore L. Environmental tobacco smoke exposure among infants, children and young people: now is no time to relax. Arch Dis Child 2017;102:117-8. [Crossref] [PubMed]
- GBD 2016 Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017;390:1345-422. Erratum in: Lancet 2017;390:1736 Erratum in: Lancet 2017;390:e38. [Crossref] [PubMed]
- Faber T, Kumar A, Mackenbach JP, et al. Effect of tobacco control policies on perinatal and child health: a systematic review and meta-analysis. Lancet Public Health 2017;2:e420-37. [Crossref] [PubMed]
- Vanker A, Gie RP, Zar HJ. The association between environmental tobacco smoke exposure and childhood respiratory disease: a review. Expert Rev Respir Med 2017;11:661-73. [Crossref] [PubMed]
- Tremblay MS, Carson V, Chaput JP, et al. Canadian 24-Hour Movement Guidelines for Children and Youth: An Integration of Physical Activity, Sedentary Behaviour, and Sleep. Appl Physiol Nutr Metab 2016;41:S311-27. [Crossref] [PubMed]
- World Health Organization. Guidelines on physical activity, sedentary behaviour, and sleep for children under 5 years of age. Geneva: World Health Organization; 2019.
- Tapia-Serrano MÁ, López-Gil JF, Sevil-Serrano J, et al. What is the role of adherence to 24-hour movement guidelines in relation to physical fitness components among adolescents? Scand J Med Sci Sports 2023;33:1373-83. [Crossref] [PubMed]
- García-Hermoso A, Ezzatvar Y, Ramírez-Vélez R, et al. Trajectories of 24-h movement guidelines from middle adolescence to adulthood on depression and suicidal ideation: a 22-year follow-up study. Int J Behav Nutr Phys Act 2022;19:135. [Crossref] [PubMed]
- García-Hermoso A, Ezzatvar Y, Alonso-Martinez AM, et al. Twenty-four-hour movement guidelines during adolescence and its association with obesity at adulthood: results from a nationally representative study. Eur J Pediatr 2023;182:1009-1017. [Crossref] [PubMed]
- García-Hermoso A, López-Gil JF, Ezzatvar Y, et al. Twenty-four-hour movement guidelines during middle adolescence and their association with glucose outcomes and type 2 diabetes mellitus in adulthood. J Sport Health Sci 2023;12:167-74. [Crossref] [PubMed]
- Miguel Angel TS, Pedro Antonio SM, Javier SS, et al. Is adherence to the 24-Hour Movement Guidelines associated with Mediterranean dietary patterns in adolescents? Appetite 2022;179:106292. [Crossref] [PubMed]
- Chaput JP, Carson V, Gray CE, et al. Importance of all movement behaviors in a 24 hour period for overall health. Int J Environ Res Public Health 2014;11:12575-81. [Crossref] [PubMed]
- Rollo S, Antsygina O, Tremblay MS. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J Sport Health Sci 2020;9:493-510. [Crossref] [PubMed]
- Tapia-Serrano MA, Sevil-Serrano J, Sánchez-Miguel PA, et al. Prevalence of meeting 24-Hour Movement Guidelines from pre-school to adolescence: A systematic review and meta-analysis including 387,437 participants and 23 countries. J Sport Health Sci 2022;11:427-37. [Crossref] [PubMed]
- Merianos AL, Mahabee-Gittens EM, Choi K. Tobacco smoke exposure and inadequate sleep among U.S. school-aged children. Sleep Med 2021;86:99-105. [Crossref] [PubMed]
- Ebrahimi M, Aghdam MH, Qorbani M, et al. Passive smoking and cardiometabolic risk factors in Iranian children and adolescents: CASPIAN-V study. J Diabetes Metab Disord 2019;18:401-8. [Crossref] [PubMed]
- Mahabee-Gittens EM, Ding L, Merianos AL, et al. Examination of the '5-2-1-0' Recommendations in Racially Diverse Young Children Exposed to Tobacco Smoke. Am J Health Promot 2021;35:966-72. [Crossref] [PubMed]
- Merianos AL, Jacobs W, Olaniyan AC, et al. Tobacco Smoke Exposure, School Engagement, School Success, and Afterschool Activity Participation Among US Children. J Sch Health 2022;92:1202-13. [Crossref] [PubMed]
- Grao-Cruces A, Nuviala A, Fernández-Martínez A, et al. Relationship of physical activity and sedentarism with tobacco and alcohol consumption, and Mediterranean diet in Spanish teenagers. Nutr Hosp 2015;31:1693-700. [PubMed]
- Bartel KA, Gradisar M, Williamson P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep Med Rev 2015;21:72-85. [Crossref] [PubMed]
- Ministry of Health, Consumer Affairs and Social Welfare. Spanish National Health Survey. Madrid, Spain; 2018. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuestaNac2017/ENSE17_Metodologia.pdf
- National Statistics Institute. National Health Survey. Results. Madrid, España; 2018. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176783&menu=resultados&idp=1254735573175#!tabs-1254736195650
- Perales J, Checa I, Espejo B. Current active and passive smoking among adults living with same sex partners in Spain. Gac Sanit 2018;32:547-52. [Crossref] [PubMed]
- National Statistics Institute. European Health Interview Survey in Spain: Method-ology. Madrid, Spain; 2020.
- Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation 2010;121:1518-22. [Crossref] [PubMed]
- Roman-Viñas B, Serra-Majem L, Hagströmer M, et al. International Physical Activity Questionnaire: Reliability and validity in a Spanish population. European Journal of Sport Science 2010;10:297-304. [Crossref]
- Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation's updated sleep duration recommendations: final report. Sleep Health 2015;1:233-43. [Crossref] [PubMed]
- Agaku IT, Odani S, King BA, et al. Prevalence and correlates of secondhand smoke exposure in the home and in a vehicle among youth in the United States. Prev Med 2019;126:105745. [Crossref] [PubMed]
- Robinson O, Martínez D, Aurrekoetxea JJ, et al. The association between passive and active tobacco smoke exposure and child weight status among Spanish children. Obesity (Silver Spring) 2016;24:1767-77. [Crossref] [PubMed]
- Wipfli HL, Samet JM. Second-hand smoke's worldwide disease toll. Lancet 2011;377:101-2. [Crossref] [PubMed]
- Lee BX, Kjaerulf F, Turner S, et al. Transforming Our World: Implementing the 2030 Agenda Through Sustainable Development Goal Indicators. J Public Health Policy 2016;37:13-31. [Crossref] [PubMed]
- Burke V, Gracey MP, Milligan RA, et al. Parental smoking and risk factors for cardiovascular disease in 10- to 12-year-old children. J Pediatr 1998;133:206-13. [Crossref] [PubMed]
- Haycraft E, Sherar LB, Griffiths P, et al. Screen-time during the after-school period: A contextual perspective. Prev Med Rep 2020;19:101116. [Crossref] [PubMed]
- Włodarska A, Doboszyńska A. Tobacco smoke exposure as a risk factor for obstructive sleep apnea in children. Pediatr Int 2020;62:840-7. [Crossref] [PubMed]
- Subramanyam R, Tapia IE, Zhang B, et al. Secondhand Smoke exposure and risk of Obstructive Sleep Apnea in Children. Int J Pediatr Otorhinolaryngol 2020;130:109807. [Crossref] [PubMed]
- Montgomery-Downs HE, Gozal D. Snore-associated sleep fragmentation in infancy: mental development effects and contribution of secondhand cigarette smoke exposure. Pediatrics 2006;117:e496-502. [Crossref] [PubMed]
- Parnell M, Gee I, Foweather L, et al. Children of Smoking and Non-Smoking Households' Perceptions of Physical Activity, Cardiorespiratory Fitness, and Exercise. Children (Basel) 2021;8:552. [Crossref] [PubMed]
- Gibbs K, Collaco JM, McGrath-Morrow SA. Impact of Tobacco Smoke and Nicotine Exposure on Lung Development. Chest 2016;149:552-61. [Crossref] [PubMed]
- Gerald LB, Gerald JK, Gibson L, et al. Changes in environmental tobacco smoke exposure and asthma morbidity among urban school children. Chest 2009;135:911-6. [Crossref] [PubMed]
- Rodrigues CMB, Schiwe D, Campos NE, et al. Exercise capacity in children and adolescents with post-infectious bronchiolitis obliterans: a systematic review. Rev Paul Pediatr 2019;37:234-40. [Crossref] [PubMed]
- Pedišić Z. Measurement issues and poor adjustments for physical activity and sleep undermine sedentary behaviour research—The focus should shift to the balance between sleep, sedentary behaviour, standing and activity. Kinesiology 2014;46:135-46.
- Parnell M, Gee I, Foweather L, et al. The impact of environmental tobacco smoke exposure on cardiorespiratory fitness in children: A pilot study. Int J EI 2019;2:240-8. [Crossref]
- Pavić I, Pavić P, Palčić I, et al. Influence of passive smoking on functional abilities in children. Int J Environ Health Res 2012;22:355-61. [Crossref] [PubMed]


