Laparoscopic management of urachal cysts
Introduction
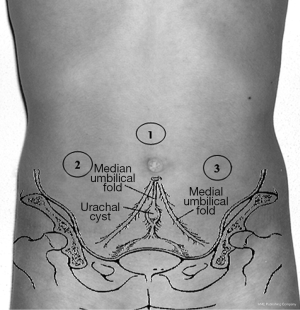
The urachus is a tubular structure that is patent during gestation. It connects the allantois at the umbilicus to the dome of the bladder during fetal development. Normally the lumen closes at about the twelfth week of gestation and obliterates completely after birth giving rise a fibrous cord running from the inferior aspect of the umbilicus to the dome of the bladder: the median umbilical ligament. The urachus is extraperitoneal and easily viewed during laparoscopic visualization of the pelvis (1). Urachal remnants represent a failure in the obliteration process. It is a rare congenital anomaly, occurring in 1.6% of children under 15 years of age and in 0.063% of adults (2) with an incidence in the adult population of about 1:5,000 while in pediatric age of about 1:150,000, extremely rare. Incomplete regression of the urachal lumen results in several anomalies: urachal cyst, sinus, diverticulum and a patent urachus. The persistence of this lumen after birth manifests in different clinical presentations of which recurrent periumbilical discharge is the most common. Among urachal anomalies, the incidence of urachal cyst range between 30% and 54% according to different reports (3,4). Complete excision is indicated both in case of persistent symptomatic remnants (umbilical discharge, recurrent infection, abdominal pain, urinary symptoms) and also when asymptomatic for the associated risk of malignant degeneration (5,6). The traditional approach for removing urachal remnant and for the treatment of complicated urachal cysts has been open surgery. However, open surgery is associated with increased morbidity and longer convalescence. We report our experience in the laparoscopic management of urachal anomalies.
Materials and methods
We included in this retrospective study all patients treated in our Department for urachal anomalies between 2006 and 2016 focusing our attention on urachal cysts diagnosis and mini-invasive treatment. This period was considered because in 2006 we started to treat this pathology laparoscopically. In a total of 16 patients 8 (50%), (6 females, 2 males) underwent open excision of an urachal remnant. The average age was 5.5 years (range, 4 months–13 years). The other eight patients were treated by laparoscopic surgery. We reviewed the charts of this group of patients to determine: age at surgery, preoperative imaging results, operative time, need for conversion, hospital stay length, postoperative complications. In this group signs and symptoms at onset were abdominal pain (acute in one patient and recurrent in two ones), macrohematuria and dysuria (1 pt), umbilical urinary discharge (3 pts), omphalitis with urinary umbilical discharge (1 pt). All patients underwent ultrasound, urinalysis was performed in 3 patients, while one of the eight was studied also with voiding cysto-urhethrogram and renal scintigraphy. The suspect of urachal remnant was based on the clinical symptoms and signs. All patients were operated on laparoscopically.
Surgical technique: all patients were administered a single dose of parenteral Amoxicillin/Sulbactam during induction of anesthesia. The patient is placed in supine position with both arms secured at the side of the body. Foley’s catheterization of bladder was performed to initially decompress the bladder during the dissection of the urachal remnant and later allows a retrograde distension of the bladder at the time of wire the insertion of the urachus at the dome of the bladder. The operating table should be preferably inclined at 20°–30° in Trendelenburg position to allow the abdominal contents to fall in a cephalad manner away from the pelvis. The surgeon and the camera surgeon stand on the right side of the patient (at the patient’s head in younger ones) with the monitor in the opposite side of the patient (normally at the foot).
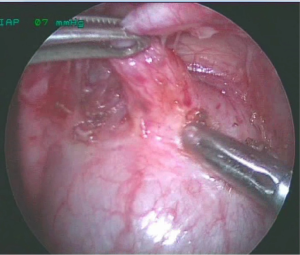
Trocars position: the first 5 mm trocar can be placed with “open” technique infraumbilically and if this is not possible in the sovraumbilical region. Once the port is placed inside the peritoneal cavity, is created an appropriate pneumoperitoneum with CO2 pressures, which range from 6–8 to 12 mmHg according to the patient’s weight. A 5-mm 0° or 30° angled lens camera (according the surgeon’s preference) is inserted and under direct vision other two 3-mm/5-mm trocars are placed respectively in the right and left iliac fossa. A third accessory trocar can be placed in case of need (Figure 1).
Technique: the first step is the identification of anatomical findings (bladder, lateral umbilical ligaments, ureters and iliac vessels). The urachus is usually easily identified midway between the umbilicus and the urinary bladder in the midline. Dissection begins with lysis of the omental adhesions, if present, which are often adherent to the cyst. Once identified the urachus we proceed with dissecting forceps and a combination of scissors or hook with the opening of the anterior parietal peritoneum and the dissection of the urachal remnant and adjacent tissues off the transversalis fascia. The urachal remnant is cauterized and divided at its superior end near the umbilicus and then carefully dissected from the anterior abdominal wall using cautery. The dissection is carried down until the space of Retzius, where the urachal remnants insert into the dome of the bladder. The anterior bladder wall is mobilized from the anterior abdominal wall as well. In the case of fistula and diverticulum there’s always a communication with the bladder dome, but it is recommended to search this communication even in presence of urachal cyst.
The bladder can be distended partially or fully to assist with this dissection. We use to fill it with vital dye diluted (methylene blue, 300 mL of normal saline and 1mL of dye) allowing better visualization of the margins of the bladder and showing any possible communications with urachal residues. At the end of dissection one endoloop (2–0 vicryl) is positioned at the level of bladder dome, insertion site of urachus proceeding with the section and extraction of the remnant with small pad of detrusor. To ensure complete closure of the bladder, two additional single stitches (3–0 polydioxanone 5 mm operative ports) are placed with a 3/8 circular needle that was bent prior the introduction. Bladder seal is than confirmed by instilling diluted methylene blue into the bladder via catheter. In case of infected cysts, it can be first introduced in endobag (inserted by a 10 mm suprapubic trocar) then open, aspirated and extracted through one operating ports. To reduce the risk of visceral adhesions is advisable to complete the parietal peritoneum closing procedure. If the procedure is completed successfully the execution of a cystoscopy is optional.
Results
The patients treated were eight, four females and four males with a mean age of 10 years (range, 6–216 months). The most common presentation was umbilical discharge seen in four patients (50%) with an omphalitis in one patient (6 months of age); the remaining four patients presented with macrohematuria/dysuria and abdominal pain, (recurrent in two and acute in one). There was one patient who presented acute abdominal pain due to infected cyst and one with umbilical overlying cellulitis.
Although abdominal ultrasonography was performed for all patients, only three patients (37.5%) had sonographic evidence of patent urachal remnants. In four patients, laparoscopic inspection of the abdominal cavity revealed the presence of a patent urachus (Figure 2), while in the others a cyst on the bladder dome (3, 4, 5, 7 cm of diameter) that extended toward the umbilicus. In one case, the cyst was inflamed and full of pus (Figure 3). In all cases, a complete dissection of the cyst was performed by proceeding from the anterior abdominal cavity to the bladder dome. The urachal cyst, along with a small cuff of the bladder dome was closed proximally with an endoloop device using 2–0 vicryl and then removed. To ensure complete closure of the bladder are positioned two additional single stitches (polydioxanone), absorbable catgut (Figure 4).
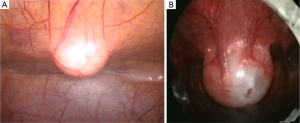
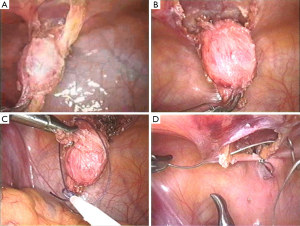
One case had a bladder to cyst communication. In three cases, the cyst was readily removed through the umbilical port after needle aspiration. The inflamed cyst, was introduced into an endo-bag, withdrew it to the umbilicus, then aspirated with a large needle; this allowed the cyst to be removed through the port. Only in this case the liquid of the cyst was purulent. In two cases, cystoscopy was performed before and after the laparoscopic excision.
Laparoscopic wide local excision was successfully completed in all cases without conversion. The procedure lasted an average of 50 minutes (range, 35–90 minutes). No intra- or postoperative complications were noted. The bladder catheter was removed after two days (at the end of procedure with patent urachus). The patients of laparoscopic group were all discharged after 2 days (range, 2–4 days). Diagnosis of urachal cyst was confirmed in all cases by histologic examination. Mean follow-up period was 4 years (range, 1–9 years) with clinical examination and abdominal ultrasound. Normally we perform a clinical and ultrasound examination at 1 month, 6 and 12 months after surgery. No reoccurrence or complications were noted.
Discussion
The urachus is the embryologic remnant of the allantois and is found among the medial umbilical ligaments which in turn are remnants of the fetal umbilical arteries. The allantois appears in the fetus around day 16; as the bladder grows and descends to the pelvis, the distal allantois obliterates. During the fourth and fifth months of gestation with the progressive fetus development grows the distance between the vertex of the bladder and the umbilicus. The urachus or medial ligament turns into a fibrous cord originating in the bladder apex and extending to the umbilicus, oscillating from 3 to 10 cm in length and from 8 to 10 mm in diameter lying between the transverse fascia anteriorly and the peritoneum posteriorly (space of Retzius), surrounded by loose areolar tissue attaching the umbilicus. Histologically, it is composed of three layers; an innermost layer of modified transitional epithelium similar to urothelium, a middle fibroconnective tissue layer and an outer layer of smooth muscle continuous with the detrusor. The incapacity for obliteration of the urachus is infrequent, but when it appears it is usually in infancy, clinically important anomalies have an incidence of 2 in 300,000 births (7,8). Aberration in the obliteration process can give rise to various types of benign urachal problems including cysts, sinus, diverticulum and patent urachus. Congenital patent urachus is rare, accounting for approximately 15% of all benign urachal abnormalities. It is usually identified during the neonatal period by a persistent urine discharge from the umbilicus, which may be minimal or intermittent. External urachal sinus and diverticulum are rarest.
Urachal cysts are the most common remnants in all the age group; a connection frequently persists between the cyst and the bladder. The diagnosis may be incidental such as during the execution of abdominal ultrasound or cystography for various other reasons; or may be entertained during the evaluation of symptoms such as acute abdominal pain, recurrent urinary infections, fever, abdominal mass, or others (3-9).
Urachal cysts arise out of desquamation and degeneration of the urachal epithelium. The small connection existing between the urachus and the bladder can clear the way for a bacterial infection, which becomes manifest with fever, abdominal pain and may even resemble an acute abdomen, a palpable abdominal mass or a urinary infection. The complications of infected urachal cysts include rupture in the peritoneal cavity leading to an inflammatory involvement of the adjacent intestine and necrotizing fasciitis which is a rare complication usually seen in children (10,11).
Usually conservative management is often advocated for children who are diagnosed within the first year of life. There are different reports showing the spontaneous involution of the urachus during the 1st year of birth with resolution of symptoms.
Clinical presentation of urachal remnants is variable and a specific representing diagnostically a challenge. Different diagnostic procedures could be used to study and confirm the clinical suspicion: ultrasonography, computed tomography (but his use is rarest in pediatric age), voiding cystourethrography and fistulography. Ultrasonography is the most accurate modality (accuracy varies from 61.1% to 91.3%) (12,13) for diagnosis in these patients, noninvasive, easily performed. The remnants can be clearly seen from the ultrasound image because the preperitoneal space is free of interfering bowel gas. Interestingly, in our series, five patients (62.5%) had no demonstrable urachal remnants on ultrasonography despite the typical clinical presentation. Diagnostic laparoscopy is useful as a diagnostic modality in the event of equivocal sonographic findings and also enables definitive management of urachal remnants. This was the case where the five patients who had negative sonographic findings were confirmed to have urachal remnants by laparoscopy and underwent laparoscopic resection.
The first laparoscopic excision of urachal remnants was described by Trondsen in 1993 (14). By a revision of the literature a surgical approach with wide local resection of urachal remnants until the dome of the bladder along with adjacent inflammatory tissue is suggested in the treatment of these lesions for their potential recurrent inflammation and for the risk of malignant degeneration.
Inadequate resection risks recurrence of periumbilical discharge as well as possible malignant transformation of the urachal remnant. Malignancy in an urachal remnant was first described in 1894 by Fisher. Tumors may arise along the entire course of the urachus, but most appear as adenocarcinoma of the bladder apex.
Urachal cysts are usually asymptomatic, but epithelial degeneration or bacterial contamination can expand the cyst lumen. When grossly infected, the expanded cyst (pyourachus) can reestablish communication with the bladder or umbilicus and rupture into peritoneal cavity causing peritonitis (15) or become fistulous with the bowel. Other complications of persistent urachus include intestinal strangulation by entrapment of a bowel loop in a ruptured urachal cyst, calculus formation in an urachus, and mechanical complication of delivery (3).
Various port placement techniques have been described. Most studies have adopted a three-trocar technique: one camera and two working ports (16,17). The most common port positions are both either infraumbilical or supraumbilical for the camera port, with the right and left mid-abdominal wall positions of the working ports forming the triangulation (17). Another placement technique is based on the position of the three ports in the right or left lateral abdominal wall (18-20).
The traditional approach to the total excision of urachal lesions in children has been via an infraumbilical transverse or midline vertical incision with port position the right and left mid-abdominal wall. Radical excision involves the removal of the whole block of tissue within the vesicoumbilical fascia, including the urachus and the medial umbilical ligaments, as well as the adjacent peritoneum from the umbilicus to bladder dome with a cuff of bladder wall. Most urachal cancers, in fact, occur in the distal part of the urachus (3).
Obviously care should be taken to position the trocars away from the umbilicus and potentially infected inflamed tissue. We prefer to start the dissection from the umbilicus to the bladder in the midline. In addition, we favored the use of a laparoscopic hook over other instruments as it allows a steep angle dissection along the posterior abdominal wall.
About the extent of resection we not perform umbilectomy but we associate a wild resection of adjacent inflamed tissue when grossly infected and in our cases we did not encounter any recurrence.
We routinely resect a pad of the bladder where the urachus inserts into its dome; it is easily identifiable intraoperatively with the distension of the bladder. We use normally one endoloop (2–0 vicryl) positioned at the level of bladder dome proceeding with the section and extraction of the remnant with small pad of detrusor. To ensure complete closure of the bladder are positioned two additional single stitches (polydioxanone), absorbable catgut, to avoid stone formation.
According to a revision of the literature there is also no consensus about the need for routine resection of the urachal remnant en bloc with a cuff of the bladder, especially in adult reports. Some argue and we agree, that excision of a cuff of the bladder is necessary to avoid recurrence and avoid possible occurrence of carcinoma in residual urachal tissue in particular if the urachal cyst is adherent and attached to the dome of the bladder with communication between the cyst and bladder, especially if this is demonstrated by imaging (2).
Before surgery we normally proceed with catheterization of the bladder. In this way is possible a control of the distension of the bladder modifying it when necessary to facilitate the dissection.
Once dissection is complete, it enables distension of the bladder to help identify where the urachus inserts into the dome of the bladder and also ensure that there is no communicating distensible urachal cyst. Postoperatively, the Foley’s catheter may be inserted 1–2 days.
According us when the urachal cyst is inflamed and infected the better will be to avoid surely open surgery for association with significant risk of surgical site infection and prolonged convalescence and to start antibiotics and analgesia therapy trying to delay the resection of the urachal remnant later (conservative management). Surgical resection should be performed after the inflammation has subsided, resolving the overlying cellulitis and reducing discharge. In one case we start surgery for acute abdomen associated to urinary frequency. Physical exam showed a right lower quadrant pain associated with rebound tenderness. Laboratory studies were remarkable for WBC count of 12,100/mm and a C-reactive protein (CRP) of 9.1 mg/dL; urinalysis was normal with absence of ultrasound evidence of urachal cyst. Laparoscopy revealed a normal appendix and an infected urachal cyst. We aspirated with a large needle the cyst introduced into an endo-bag withdrew it to the umbilicus. In case of inflammation and infection we considered this approach the adequate and appropriate. A needle aspiration via ultrasonography to drain the pyourachus could cause a surgical site infection. A 30% of recurrence is seen when complicated urachal cysts are managed conservatively by means of drainage and antibiotic therapy (11).
There have also been two very short series of laparoscopic management of urachal remnants, one in four adults and one in four children. Both of these series used basically the same technique and showed that a laparoscopic technique can be used safely and effectively to remove all urachal remnant tissue with minimal morbidity (21).
Conclusions
In the pediatric age group, laparoscopy represents an excellent diagnostic and therapeutic instrument, especially for patients with acute abdominal pain, doubtful clinical history, and no clear signs on physical and instrumental examinations.
Urachal remnant should be managed in standardized manner.
Clinical evaluation is the first step with an appropriate physical examination. Ultrasonography should be performed to confirm the suspected diagnosis. Sinography (fistulography) is useful to delineate the urachal sinuses. We warrant abdominal tomography. Laparoscopy is useful to confirm the diagnosis in instances where ultrasonography fails to identify the presence of urachal remnants but the recurrent umbilical discharge is highly suggestive.
An urachal cyst should be excised electively by laparoscopic approach. If inflamed excision should be performed electively once the infection and inflammation has abated and it should be performed laparoscopically. If laparoscopy is performed with a pyourachus we suggest dissecting carefully the cyst and the inflamed tissue around it, to introduce it into an endobag a then to aspire it through the umbilicus.
Traditionally excision of the urachus starts at the umbilicus and extends down to the bladder.
If the procedure is completed successfully, the execution of a cystoscopy is optional. According to the literature, in the adult patient, laparoscopic management of urachal pathology is clearly feasible. In our opinion, the laparoscopic excision of urachal cysts represents an effective option, as well as with the pediatric patient. It affords an excellent panoramic view of the operative field (magnified dissection of the preperitoneal plane) and easier access to the bladder dome in contrast to classical open surgical incisions and permits an acceptable excision of the lesion without producing marked scarring; it yields good long-term cosmetic results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by our institutional ethics committee and written informed consent was obtained from all patients.
References
- Patrzyk M, Glitsch A, Schreiber A, et al. Single-incision laparoscopic surgery as an option for the laparoscopic resection of an urachal fistula: first description of the surgical technique. Surg Endosc 2010;24:2339-42. [Crossref] [PubMed]
- Siow SL, Mahendran HA, Hardin M. Laparoscopic management of symptomatic urachal remnants in adulthood. Asian J Surg 2015;38:85-90. [Crossref] [PubMed]
- Chiarenza SF, Scarpa MG, D'Agostino S, et al. Laparoscopic excision of urachal cyst in pediatric age: report of three cases and review of the literature. J Laparoendosc Adv Surg Tech A 2009;19 Suppl 1:S183-6. [Crossref] [PubMed]
- Yamzon J, Kokorowski P, De Filippo RE, et al. Pediatric robot-assisted laparoscopic excision of urachal cyst and bladder cuff. J Endourol 2008;22:2385-8; discussion 2388. [Crossref] [PubMed]
- Pesce C, Costa L, Musi L, et al. Relevance of infection in children with urachal cysts. Eur Urol 2000;38:457-60. [Crossref] [PubMed]
- Khurana S, Borzi PA. Laparoscopic management of complicated urachal disease in children. J Urol 2002;168:1526-8. [Crossref] [PubMed]
- Stone NN, Garden RJ, Weber H. Laparoscopic excision of a urachal cyst. Urology 1995;45:161-4. [Crossref] [PubMed]
- Gearhart JP, Jeffs RD. Exstrophy-epispadias complex and bladder anomalies. In: Campbell’s Urology, Seventh Edition. Philadelphia: Saunders WB Co., 1993:1815.
- Bertozzi M, Nardi N, Prestipino M, et al. Minimally invasive removal of urachal remnants in childhood. Pediatr Med Chir 2009;31:265-8. [PubMed]
- Huang CS, Luo CC, Chao HC, et al. Urachal anomalies in children: experience at one institution. Chang Gung Med J 2003;26:412-6. [PubMed]
- Castillo OA, Vitagliano G, Olivares R, et al. Complete excision of urachal cyst by laparoscopic means: a new approach to an uncommon disorder. Arch Esp Urol 2007;60:607-11. [Crossref] [PubMed]
- McCollum MO, Macneily AE, Blair GK. Surgical implications of urachal remnants: Presentation and management. J Pediatr Surg 2003;38:798-803. [Crossref] [PubMed]
- Widni EE, Höllwarth ME, Haxhija EQ. The impact of preoperative ultrasound on correct diagnosis of urachal remnants in children. J Pediatr Surg 2010;45:1433-7. [Crossref] [PubMed]
- Trondsen E, Reiertsen O, Rosseland AR. Laparoscopic excision of urachal sinus. Eur J Surg 1993;159:127-8. [PubMed]
- Siegel JF, Winfield HN, Valderrama E, et al. Laparoscopic excision of urachal cyst. J Urol 1994;151:1631-3. [PubMed]
- Lipskar AM, Glick RD, Rosen NG, et al. Nonoperative management of symptomatic urachal anomalies. J Pediatr Surg 2010;45:1016-9. [Crossref] [PubMed]
- Patrzyk M, Wilhelm L, Ludwig K, et al. Improved laparoscopic treatment of symptomatic urachal anomalies. World J Urol 2013;31:1475-81. [Crossref] [PubMed]
- Okegawa T, Odagane A, Nutahara K, et al. Laparoscopic management of urachal remnants in adulthood. Int J Urol 2006;13:1466-9. [Crossref] [PubMed]
- Li Destri G, Schillaci D, Latino R, et al. The urachal pathology with umbilical manifestation: overview of laparoscopic technique. J Laparoendosc Adv Surg Tech A 2011;21:809-14. [Crossref] [PubMed]
- Araki M, Saika T, Araki D, et al. Laparoscopic management of complicated urachal remnants in adults. World J Urol 2012;30:647-50. [Crossref] [PubMed]
- Jeong HJ, Han DY, Kwon WA. Laparoscopic management of complicated urachal remnants. Chonnam Med J 2013;49:43-7. [Crossref] [PubMed]