Training for MIS in pediatric urology: proposition of a structured training curriculum
Introduction
Minimally invasive techniques for an ever-growing number of indications in pediatric surgery are adopted around the world and are becoming the gold standard for certain indications (1).
Laparoscopic surgery in urology differs from its counterparts in general surgery in that there are no relatively simple high-volume procedures suitable for training. Consequently, laparoscopy in urology has traditionally been considered a sub-specialist procedure. Therefore, the need of well-trained and certified laparoscopic urologists will increase (2).
Training in pediatric urological laparoscopic surgery has been inadequate because of several factors, e.g. a shortage of designated training centers, a shortage of recognized trainers, and the lack of appropriate facilities, in the form of either equipment, expertise or support from respective trusts (2).
Minimally invasive surgery (MIS) is technically more difficult than ordinary open surgery and several complications can happen especially at the beginning of experience (3,4).
Moreover, the advantage of successfully performing different urology procedures like nephrectomy, pyeloplasty, orchidopexy, by laparoscopy in pediatric age group mandates formal laparoscopic training of practicing urologists (5). Since laparoscopic surgery requires different set of surgical skills and way of viewing anatomy, so a need for planned training programs is warranted to help urologists gain considerable hands on training and experience in basic pediatric laparoscopic skills (5).
At the moment in Europe there are a lot of training centers for MIS but a standardized MIS training program in pediatric urology doesn’t exist. A training center should be able to offer laparoscopic training in both a structured “dry” and “wet” laboratory facility (3). Trainees at such center should be able to participate in complex laparoscopic surgery and undertake laboratory-based simulation practice on a daily basis. They would be expected to undergo structured training in all aspects of the procedure, then to perform a designated number of cases under supervision (6,7). Therefore, a structured and focused training curriculum in MIS urology is needed for optimal utilization of the available training hours (5).
We performed a review of current literature with the ultimate goal to construct a curriculum that provides a safe, uniform, efficient and procedure-specific training program in MIS urology to gain experience while maintaining patient safety.
Methods
A Literature search was performed using PubMed and Medline databases to identify studies published during the last 15 years that described training in pediatric laparoscopic surgery and specifically for urological procedures. The following keywords were used: “training”, “laparoscopy”, “urology”, “children”, “MIS”, “curriculum”, “technical skills”, “animal models”, “simulation”.
Searches were also performed using the following as limit: clinical trials, randomized controlled trials, multicenter retrospective, prospective studies, expert opinion. Conference abstracts were excluded because of the limited data presented in them.
Although no language restrictions were imposed initially, the search was limited to studies published in the English language for the full-text review and final analysis.
After identifying relevant titles, the abstracts of these studies were read to decide if the study was eligible. The full article was retrieved when the information in the title and/or abstract appeared to meet the objective of our review.
Results
A total of 26 studies of adolescent (8-27) and pediatric surgery (28-33). Huge variation was noticed in the types of validity sought by researchers and suboptimal incorporation of these tools into curricula was noted across the subgroups of urological surgery. The following key recommendations emerged from the review: adoption of simulation-based curricula in training; better integration of dedicated training time in simulated environments within a trainee’s working hours; better incentivization for educators and assessors to improvise, research, and deliver teaching using the technologies available; and continued emphasis on developing nontechnical skills in tandem with technical operative skills.
However, only 6 out of the 26 selected studies were focused on pediatric surgery (28-33).
The role of simulation in urological training
Laparoscopic surgery is different from open surgery because of the increased need for hand-eye co-ordination to perform tasks when looking at a screen and to compensate for not being able to operate under direct vision; increased need for manual dexterity to compensate for the use of long instruments (the fine motor skills required for performing laparoscopic surgery are greater than in open surgery since small movements are more amplified in laparoscopic surgery than open surgery because of the longer instruments used in laparoscopic surgery), which can amplify any error in movement; the fulcrum effect of the body wall, that is, when the surgeon moves his hand to the patient’s right the operating end of the instrument moves to the patient’s left on the monitor; the lack of sensation of touch using hands; and the lack of three-dimensional images.
Evidence suggests that simulation can act as a valuable adjunct to clinical training (24). It enables the trainee to repeatedly practice a procedure, as a result reducing the learning curve associated with the acquisition of new technical and non-technical skills without compromising patient safety. Simulators are becoming an integral part of the urology training curriculum and their effectiveness is totally dependent on the structure of the program implemented. An optimal simulation program would involve trainees receiving repeated exposure to the simulator over an extended period of time. Trainees can often start with low fidelity simulators to grasp basic surgical skills before moving onto full-procedural simulations as they progress through their training (25,26).
There are multiple types of simulators which include mechanical, virtual reality, hybrid simulators and animal models.
The most common simulators are video-box trainers. Training using a box model involves performance of tasks that are encountered in laparoscopic surgery using animal tissues, plastic models, foam, cloth, or other materials. The images can be obtained using a laparoscope (camera) and viewed on monitors. This is called a video-box trainer. Another type of box trainer is the mirrored-box trainer, in which mirrors are used to show the working field and direct vision of the working field is prevented. Training by box trainer may work by repeated practice and improve hand-eye coordination and manual dexterity (26).
For the endourological procedures of cystoscopy and ureterorenoscopy, numerous high-fidelity bench-top models and virtual reality (VR) simulators have been created. High-fidelity simulators, such as the Uro-Scopic Trainer consist of physical mannequins and allow trainees to practice using the standard operating instruments. VR trainers, such as the URO-Mentor, simulate surgical procedures through interactions with computer interfaces (24).
The recent literature has seen insurgence of several of animate simulators comprising porcine, rabbit and chicken models. On account of the natural tissue properties inherent to these animal models, they are proving to be instrumental in acquisition of higher surgical skills such as dissection, suturing and use of energy sources, all of which are required in real-time clinical scenarios (27). In vivo training in the animal model continues to be the most sophisticated training method before resorting to real-time surgery (27,31).
One consideration tutors need to consider is that simulation can be resource demanding, with a need for faculty, equipment and a location to be provided. Another consideration is that there is no agreed consensus on how to validate simulation tools, with different investigators adopting different approaches. More work is needed to compare different simulators and to identify which ones are more effective at training students (24).
Criteria for training program in pediatric laparoscopic urological surgery
In a recent paper (30), within a uniform learning curve for procedural training, the authors identified the different steps of a structured training curriculum in pediatric MIS, from basic skills up to certification. The program involves firstly acquisition of theoretical knowledge, hand-eye coordination and other basic laparoscopic skills in skills laboratory, specific procedural training in skills laboratory. The next steps are: video-assisted side-by-side training in the hospital operating room, operating under supervision in the hospital operating room and finally feedback through registration of results and certification.
In accordance with ESPES guidelines (30), structured for training in pediatric MIS, we propose that also pediatric urologists have to obtain a valid MIS training curriculum completing the following 4 steps:
- Theoretical part;
- Experimental training (simulation on pelvic trainer, virtual-reality simulators, animal models, 3-D ex-vivo models);
- Stages in European centers of reference for pediatric MIS urology;
- Personal operative experience.
Those wishing to learn urological laparoscopy, assuming no previous laparoscopic skills, must complete the following steps:
- Acquisition of theoretical knowledge through participation to theoretical courses and masterclass (at least 3 courses):critical educational components include the pathophysiology of diseases, diagnosis, operative indications and contraindications, principles of pre- and post-operative care and understanding the prevention, diagnosis and treatment of complications;
- Complete a “dry-lab” course (at least 10–20 hours of training): basic laparoscopic skills such as access, dissection, haemostasis and reconstruction are initially best acquired in a “skills-laboratory” environment, thus improving skills by practice (11,23,24,28);
- Complete an animal-based “wet-lab” course (at least 10 hours of training): in vivo animal models are often used for the acquisition and refinement of advanced operative skills. Animal models most closely resemble operating on a live patient and they are the only models that can effectively simulate bleeding, tissues handling and complications (27,31);
- Attend a high-volume center (at least a 1–3 months stage) to watch designated cases and to learn all aspects of the surgery (11);
- Start practising basic laparo/endoscopic urological procedures (e.g. inguinal hernia repair, varicocele repair, cystoscopy), under supervision of a mentor (11,30,32);
- Start doing complex laparoscopic urological procedures (e.g. nephrectomy, partial nephrectomy, pyeloplasty) with the mentor (11,30,32);
- At the end of the training period, perform several procedures independently observed by an experienced laparoscopic surgeon (30);
- Feedback through registration of results and certification (11,30).
The operative procedures to perform may be divided in 3 modules:
- ureteroscopy/percutaneous renal access;
- laparoscopic ablative renal surgery;
- laparoscopic reconstructive renal surgery.
The number of laparoscopic procedures a surgeon needs to perform during training remains difficult to estimate, due to the lack of a consensus or guidelines on how to assess laparoscopic training in pediatric urology.
ESPES guidelines for pediatric MIS training proposed that trainees have to perform 30 procedures as cameraman and >50 basic MIS procedures as main surgeon under supervision (30). The BAUS indicated the aim to do at least 12 marker cases per year (11). For intricate reconstructive MIS (such as laparoscopic pyeloplasty) approximately 30 procedures are proposed as necessary to develop proficiency (32).
We propose that pediatric surgeons wishing to learn urological laparoscopy have to complete >50 basic MIS and/or endoscopic procedures and >20 advanced MIS procedures as main surgeon under supervision of an expert tutor.
Assessment of laparoscopic skills acquisition
The best technique for measuring and assessing specific surgical skills or techniques is currently considered to be the OSATS evaluation. This is based on the extensively utilized and accepted objective structured clinical examination (OSCE) format and is composed by checklists and a global rating scale.
The checklists encompass specific tasks that must be completed during a technique or procedure. A point is given if the task is performed correctly, and no point is given if the task is done incorrectly or not done at all. In addition, a qualitative component of assessment is performed using a global rating scale. Although the OSATS has been shown to have reliability and validity in assessing operative performance, the specific cut-off point that distinguishes the competent from the incompetent surgeon has yet to be defined for specific procedures (24).
In our training program, the global rating scale of trainees’ performances will consist of a Likert-type scale with scores ranging between 1 and 5. A score of 1 has the poorest performance and a score of 5 has the highest level of performance. The score of trainees’ performances will be expressed as follows (Figure 1):
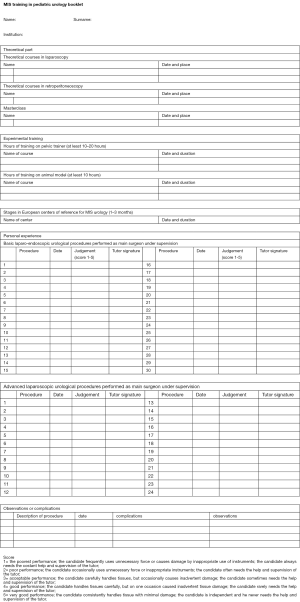
- Very poor performance; the candidate frequently uses unnecessary force or causes damage by inappropriate use of instruments; the candidate always needs the costant help and supervision of the tutor;
- Poor performance; the candidate occasionally uses unnecessary force or inappropriate instruments; the candidate often needs the help and supervision of the tutor;
- Acceptable performance; the candidate carefully handles tissues, but occasionally causes inadvertent damage; the candidate sometimes needs the help and supervision of the tutor;
- Good performance; the candidate handles tissues carefully, but on one occasion caused inadvertent tissue damage; the candidate rarely needs the help and supervision of the tutor;
- Very good performance; the candidate consistently handles tissue with minimal damage; the candidate is independent and he never needs the help and supervision of the tutor.
Discussion
Pediatric urology is a relatively new medical specialty that came out of urology and pediatric surgery (2). MIS is becoming a more prominent procedure in the field. Over the years, MIS has evolved due to improvements in the instrumentation and the creativity of specialized surgeons.
Simple diagnostic and ablative procedures have payed the way for intricate, reconstructive, laparoscopic surgery (32).
Currently, orchidopexy, partial nephrectomy, and ureteral reimplantation are widely performed in pediatric urology. Laparoscopic retroperitoneal and transperitoneal pyeloplasty is believed to be the gold standard procedure, and patients are increasingly requesting ‘keyhole’ surgery (32).
The outcomes of MIS are comparable to those of open techniques. Laparoscopy has been shown to be effective and safe with a low morbidity rate (2,8). It is known to have a steep learning curve due its technical challenges. Extended training and repetition are needed to become a skillful laparoscopic surgeon (8,9). In fact, the rate of complication in MIS is mainly dictated by the experience of the surgeon (32).
The intensive training needed for this procedure has become an important issue and has received increasing attention from the medical community. Nevertheless, no minimum number of procedures has been specified as a requirement for performing MIS procedures in pediatric urology. There is no consensus concerning the number of operations needed to become proficient in MIS. Assessment of surgeons is mainly based on their supervisors’ evaluations.
A structured and focused training curriculum in MIS for pediatric urologists needs of a standardized training program to secure an optimal utilization of the available training hours and a standard of technical skill qualification in MIS (30).
With the opportunity of simulating MIS, we aim to start training outside of the operating room. Laparoscopic skills such as access, dissection, suturing, knot-tying, precision cutting, haemostasis and reconstruction are initially best acquired in a “skills-laboratory” environment, thus improving skills by practice (8,9). There are also artificial models to simulate specific pathologies, such as pyelo-ureteric junction obstruction (PUJO), to reproduce and simulate the single steps of specific interventions (23). We recommend that each unit have an in-house dry simulator to maintain competence with the skills. Translational studies have shown that when a surgical resident successfully completes a simulator curriculum, his performance in the operating room improves (11).
Then we move on to practicing procedure-specific skills on animal models. The trainees should complete one or more animal-based “wet-lab” courses, where they have the chance of mastering complex tasks in a training facility. The most common used animal models are: pig-models that permit to perform several laparoscopic procedures, from those basic such as hernia repair, varicocele repair to those complex such as nephrectomy, partial nephrectomy, ureteral reimplantation, bladder suspension and rabbit-models, ideally suited for training in laparoscopic neonatal surgery for the possibility of simulating several laparoscopic neonatal procedures (25,31).
However, in some countries it is by law not possible to practice on live animals because there is an increasing reluctance from Animal Ethical Committees to allow for animal experiments, apart from the huge financial costs of such facilities. In this sense the now available 3-D ex-vivo models for different complex procedures may be much more worthwhile because the procedure can be practiced repetitively (13,15). A wide variety of simulators of differing fidelity are currently available, teaching both technical and non-technical urological surgical skills (24-26).
Another important point in the training program is to watch live procedures in the context of demonstrations such as MasterClass and attend a high-volume surgical center to watch designated cases (11).
After this step, the trainee will start practising laparoscopy in the operating theater firstly as cameraman and then he/she will start to perform laparoscopic/endoscopic basic procedures on patients guided by an expert tutor (11,30,32). At the end of the training period, the trainee should do several procedures independently observed by an experienced laparoscopic surgeon.
Fundamentals of Laparoscopic Surgery (FLS) is a comprehensive web-based education module that includes a hands-on skills training component and assessment tool designed to teach the physiology, fundamental knowledge and technical skills required in basic laparoscopic surgery. The FLS program is a joint educational offering of SAGES and the American College of Surgeons (ACS), designed for surgical residents, fellows and practicing physicians to learn and practice basic laparoscopic skills. FLS consists of web-based study guides, hands-on manual skills practice and training via the FLS Laparoscopic Trainer Box; and an assessment tool that measures both cognitive and technical skills (26,27,34-37).
Basing on this models, we propose to standardize guidelines for a laparoscopic training curriculum, specially designed for pediatric urologists. This complete training curriculum has to be acquired step by step, from acquisition of theoretical knowledge and basic laparoscopic skills in experimental setting till to the autonomous and safe performance of laparoscopic procedures on patients. It concludes with certification of the completion of all steps of the training program.
According to our proposal, a structured MIS training curriculum for pediatric urologists must contain the following educational components: (I) theoretical knowledge; (II) practice-based learning and improvement in experimental setting; (III) stages in high-volume centers of pediatric MIS urology; (IV) personal operative experience.
Critical educational components include the pathophysiology of disease, diagnosis, operative indications and contraindications, principles of pre- and post-operative care and understanding the prevention, diagnosis and treatment of complications. Acquisition and mastery of basic laparoscopic skills must precede the performance of advanced laparoscopic operations. There is a core group of fundamental skills common to all laparoscopic operations. Examples of such skills include hand-eye coordination, two-handed instrument manipulation, dissection, intra-corporeal suturing, intra- and extra-corporeal knot-tying. Such skills are best acquired in skills laboratories using surgical trainers, animal models, virtual reality trainers before the trainee perform these procedures in the operating room on patients.
The number of laparoscopic procedures a surgeon needs to perform during training remains difficult to estimate, due to the lack of a consensus or guidelines on how to assess laparoscopic training in pediatric urology. Based on only the number of operations, it seems obvious that the number of laparoscopic procedures per pediatric urology clinic is not high enough to broadly teach MIS. This will predominantly affect medical doctors at the beginning of their surgical training (such as fellows and residents). A potential solution to increase experience in MIS may include collaboration between laparoscopic pediatric surgeons and urologists. By increasing the number of procedures with which surgeons are involved, the training time necessary to master MIS will be shorter compared with that among pediatric urologists alone. To increase laparoscopic exposure, centralizing the patients at one center may also be a viable option (32).
ESPES guidelines for pediatric MIS training proposed that trainees have to perform 30 procedures as cameraman and >50 basic MIS procedures as main surgeon under supervision (30). The BAUS indicated the aim to do at least 12 marker cases per year (11). For intricate reconstructive MIS (such as laparoscopic pyeloplasty) approximately 30 procedures are proposed as necessary to develop proficiency (32).
We propose that pediatric surgeons wishing to learn urological laparoscopy have to complete >50 basic MIS urological procedures and >20 advanced MIS urological procedures as main surgeon under supervision of an expert tutor. On the other side, in a recent paper, authors concluded that it is evident that the post-mentorship practice is affected by the number of cases initially performed during the training period. The development of an “expert” laparoscopic is dependent not only on initial training experience, but continued education through ongoing case exposure (29).
Evaluation of trainees will involve 3 phases: direct observation of performance, evaluation to promote improvement and avoid errors, and documentation of procedural skills. Direct observation and evaluation are the responsibilities of the supervising attending physician at the time of each procedure. Feedback should be immediate and direct, with constructive and informative discussion between the attending physician and fellow. The conduct and objective assessment of procedural competence should be documented by the attending physician supervising.
In addition, trainees will be required to maintain a training logbook of all of their procedures, which should be reviewed by the program director at regular intervals during the period of training and at completion of the fellowship. The procedure logbook also should include documentation, if available, of any significant complications occurred (Figure 1).
Certification of competence requires satisfactory performance in a minimum number of cases of each procedure under direct supervision, with independent performance of some procedures.
All steps completed during the training period will be registered on the personal training booklet.
At the end of the training program, each trainee has to attend an exit examination that will consist of a written test to verify the theoretical knowledge acquired during the training period. After that, the trainee has to perform a practical surgical test in the operating room performing a basic MIS urological procedure under supervision to verify the laparoscopic competence acquired. After passing this examination, each applicant will receive a certification.
In conclusion, we would suggest to standardize and to validate this training curriculum in the current practice. We think that this MIS training program in pediatric urology adopt a policy that assures an integrated acquisition of basic and advanced laparoscopic skills during residency training in pediatric urology. Each European country should adopt this program so as to secure a standardized technical qualification in MIS urology for all future pediatric surgeons. To provide high quality MIS training, exposure to laparoscopic urological procedures must be expanded. This may be achieved by centralizing patients into a common center, collaborating with other specialties and training outside the operating theatre.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tam PK. Laparoscopic surgery in children. Arch Dis Child 2000;82:240-3. [Crossref] [PubMed]
- Norris RD, Ost MC. Evolution of laparoscopy in pediatric urology. Expert Rev Med Devices 2009;6:689-98. [Crossref] [PubMed]
- Bethlehem MS, Kramp KH, van Det MJ, et al. Development of a standardized training course for laparoscopic procedures using Delphi methodology. J Surg Educ 2014;71:810-6. [Crossref] [PubMed]
- Esposito C, Mattioli G, Monguzzi GL, et al. Complications and conversions of pediatric videosurgery: the Italian multicentric experience on 1689 procedures. Surg Endosc 2002;16:795-8. [Crossref] [PubMed]
- Gupta V, Yadav SK, Dean E, et al. Paediatric laparoscopic orchidopexy as a novel mentorship: Training model. Afr J Paediatr Surg 2013;10:117-21. [Crossref] [PubMed]
- Marks JM, Nussbaum MS, Pritts TA, et al. Evaluation of endoscopic and laparoscopic training practices in surgical residency programs. Surg Endosc 2001;15:1011-5. [Crossref] [PubMed]
- Van Hove C, Perry KA, Spight DH, et al. Predictors of technical skill acquisition among resident trainees in a laparoscopic skills education program. World J Surg 2008;32:1917-21. [Crossref] [PubMed]
- Keeley FX Jr, Timoney AG, Rané A, et al. Mentorship in urological laparoscopic surgery: lessons learned. BJU Int 2009;103:1111-3. [Crossref] [PubMed]
- Shalhav AL, Dabagia MD, Wagner TT, et al. Training postgraduate urologists in laparoscopic surgery: the current challenge. J Urol 2002;167:2135-7. [Crossref] [PubMed]
- Marguet CG, Young MD, L'Esperance JO, et al. Hand assisted laparoscopic training for postgraduate urologists: the role of mentoring. J Urol 2004;172:286-9. [Crossref] [PubMed]
- Keeley FX Jr, Rimington PD, Timoney AG, et al. British association of urological surgeons laparoscopic mentorship guidelines. BJU Int 2007;100:247-8. [Crossref] [PubMed]
- Sullivan ME, Jones A. Mentoring in laparoscopic urology. BJU Int 2007;99:7-8. [Crossref] [PubMed]
- Pansadoro A, Curto F, Mugnier C, et al. Teaching laparoscopy: the new challenge. BJU Int 2007;99:726-7. [Crossref] [PubMed]
- Okeke AA, Timoney AG, Wright MP. Laparoscopic urological surgery: mentor matters. BJU Int 2006;97:902-3. [Crossref] [PubMed]
- Bariol SV, Tolley DA. Training and mentoring in urology: the 'LAP' generation. BJU Int 2004;93:913-4. [Crossref] [PubMed]
- Keeley FX Jr, Eden CG, Tolley DA, et al. The British Association of Urological Surgeons: guidelines for training in laparoscopy. BJU Int 2007;100:379-81. [Crossref] [PubMed]
- Hennayake S, Jayawardhena D, Kumara S, et al. Training in laparoscopic renal surgery, in a few weeks of intense exposure. J Pediatr Urol 2005;1:295-9. [Crossref] [PubMed]
- Rabenalt R, Minh D, Dietel A, et al. Laparoscopic surgery in urology: Taining and education. Urologe A 2006;45:1155-6, 1158-60, 1162.
- Shepherd W, Arora KS, Abboudi H, et al. A review of the available urology skills training curricula and their validation. J Surg Educ 2014;71:289-96. [Crossref] [PubMed]
- Laguna MP, de Reijke TM, Wijkstra H, et al. Training in laparoscopic urology. Curr Opin Urol 2006;16:65-70. [Crossref] [PubMed]
- Hoznek A, Katz R, Gettman M, et al. Laparoscopic and robotic surgical training in urology. Curr Urol Rep 2003;4:130-7. [Crossref] [PubMed]
- Palter VN, Orzech N, Reznick RK, et al. Validation of a structured training and assessment curriculum for technical skill acquisition in minimally invasive surgery: a randomized controlled trial. Ann Surg 2013;257:224-30. [Crossref] [PubMed]
- Zhang J, Liu C. A training model for laparoscopic dismembered pyeloplasty. Nan Fang Yi Ke Da Xue Xue Bao 2013;33:1541-3. [PubMed]
- Preece R. The current role of simulation in urological training. Cent European J Urol 2015;68:207-11. [Crossref] [PubMed]
- Ahmed K, Amer T, Challacombe B, et al. How to develop a simulation programme in urology. BJU Int 2011;108:1698-702. [Crossref] [PubMed]
- Brewin J, Ahmed K, Challacombe B, et al. An update and review of simulation in urological training. Int J Surg 2014;12:103-8. [Crossref] [PubMed]
- Ganpule A, Chhabra JS, Desai M. Chicken and porcine models for training in laparoscopy and robotics. Curr Opin Urol 2015;25:158-62. [Crossref] [PubMed]
- Brydges R, Farhat WA, El-Hout Y, et al. Pediatric urology training: performance-based assessment using the fundamentals of laparoscopic surgery. J Surg Res 2010;161:240-5. [Crossref] [PubMed]
- Farhat W, Khoury A, Bagli D, et al. Mentored retroperitoneal laparoscopic renal surgery in children: a safe approach to learning. BJU Int 2003;92:617-20; discussion 620. [Crossref] [PubMed]
- Esposito C, Escolino M, Saxena A, et al. European Society of Pediatric Endoscopic Surgeons (ESPES) guidelines for training program in pediatric minimally invasive surgery. Pediatr Surg Int 2015;31:367-73. [Crossref] [PubMed]
- Esposito C, Escolino M, Draghici I, et al. Training Models in Pediatric Minimally Invasive Surgery: Rabbit Model Versus Porcine Model: A Comparative Study. J Laparoendosc Adv Surg Tech A 2016;26:79-84. [Crossref] [PubMed]
- Schroeder RP, Chrzan RJ, Klijn AJ, et al. Training potential in minimally invasive surgery in a tertiary care, paediatric urology centre. J Pediatr Urol 2015;11:271. [Crossref] [PubMed]
- Cook A, Khoury A, Bagli D, et al. The development of laparoscopic surgical skills in pediatric urologists: longterm outcome of a mentorship-training model. Can J Urol 2005;12:2824-8. [PubMed]
- Vlaovic PD, McDougall EM. New age teaching: beyond didactics. ScientificWorldJournal 2006;6:2370-80. [Crossref] [PubMed]
- La Torre M, Caruso C. The animal model in advanced laparoscopy resident training. Surg Laparosc Endosc Percutan Tech 2013;23:271-5. [Crossref] [PubMed]
- Ritter EM, Scott DJ. Design of a proficiency-based skills training curriculum for the fundamentals of laparoscopic surgery. Surg Innov 2007;14:107-12. [Crossref] [PubMed]
- Peters JH, Fried GM, Swanstrom LL, et al. Development and validation of a comprehensive program of education and assessment of the basic fundamentals of laparoscopic surgery. Surgery 2004;135:21-7. [Crossref] [PubMed]


