
Bilateral fronto-orbital advancement combined with cranial vault release using a free-floating bone flap technique for nonsyndromic unilateral coronal synostosis
Highlight box
Key findings
• Bilateral fronto-orbital advancement combined with cranial vault release (CVR) using a free-floating bone flap technique offers favorable outcomes in intracranial volume expansion and fronto-orbital symmetry.
What is known and what is new?
• At present, the main surgical methods for the treatment of unilateral coronal synostosis (UCS) are fronto-orbital advancement and endoscopic suturectomy.
• A more comprehensive surgical release offers favorable outcomes in intracranial volume expansion and fronto-orbital symmetry.
What are the implications, and what should change now?
• Bilateral fronto-orbital advancement combined with CVR in children with nonsyndromic UCS was effective without serious complications, and it is worthy of further promotion and application in clinical practice.
Introduction
Unilateral coronal synostosis (UCS) not only results in cosmetic malformation with ipsilateral flattening of the frontal and parietal bones, temporal retrusion with elevation and recession of the supraorbital rim (also known as “harlequin” eye deformity) (1). Of note, single-suture craniosynostosis may also result in a significant volumetric reduction of the skull cavity on the affected side with consequent functional impact due to potential increases in intracranial pressure (ICP) in about 15–20% of children (2). The goals of operative treatment are therefore to improve appearance and allow unrestricted brain growth while minimizing any detriment to brain development (3).
At present, the main surgical methods for the treatment of UCS are fronto-orbital advancement and endoscopic suturectomy. However, for severe unilateral premature closure of the coronal suture, this method cannot address the compression of the brain or expand the volume of the skull cavity. From April 2014 to May 2019, we treated 20 patients with nonsyndromic UCS using bilateral fronto-orbital advancement combined with anterior cranial vault release (CVR). During the operation, we used a non-detachable free-floating bone flap (FFBF) technique, which not only improved the patient’s aesthetics but also expanded the skull cavity as much as possible to couple the best results from both cosmetic and functional perspectives. We report our experience with bilateral fronto-orbital advancement combined with CVR + FFBF technique and the resulting changes in the anterior cranial vault asymmetry index (ACVAI) and intracranial volume. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-495/rc).
Methods
Clinical data
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). After obtaining approval from the Shanghai Children’s Medical Center Review Board (No. SCMCIRB-K2022035-1), we carried out a retrospective analysis of all demographic, surgical, and radiographic data pertaining to patients treated for isolated, nonsyndromic UCS between April 2014 and May 2019. Written consent was obtained from patients’ parents or guardians. The study captured key information regarding all patients presenting with the following clinical features: ipsilateral flattening of the frontal, parietal, and occipital bones; temporal retrusion with elevation and recession of the supraorbital rim, a widened ipsilateral palpebral fissure, and vertical orbital dystopia. The following exclusion criteria were considered: syndromic diagnosis, multi-suture involvement, and follow-up under 1 year. Furthermore, an incomplete dataset due to any type of missing data was considered as a cause for exclusion from final analysis.
As an expected feature of UCS, the skull cavity was smaller ipsilateral to the synostosis compared to the healthy contralateral side. The full list of data collected in each patient’s case report form (CRF) for the purposes of this study included: patient demographic information, age at surgical treatment, operative details, perioperative complications graded according to the Clavien-Dindo classification (4), and postoperative outcomes for all patients with at least 1 year of follow-up.
Reporting was conducted in agreement with the standardized quality assessment scale designed for retrospective studies in pediatric surgery proposed by the Divisions of Pediatric Surgery and Neonatology, and the Department of Epidemiology at Stanford University School of Medicine (5).
Operative method
The operation for UCS was standardized and identical for all patients who were included in the present study. The surgical procedure consisted of removing, shaping, and repositioning the fronto-orbital skull segments and cranial vault remodeling using the FFBF technique. A wavy bicoronal incision was preformed, and scalp clips were used to maintain meticulous hemostasis. Subperiosteal dissection proceeded to the supraorbital rims with release of the supraorbital nerves. Temporalis muscles were elevated in continuity with the flap. The dissection of the lateral orbit margin continued inferiorly below the frontozygomatic suture. The frontal bone flap and bilateral supraorbital plates were detached with an air drill. Abnormal hyperplasia of the lesser wing between the anterior and middle skull bases was removed. After the reconstruction of the supraorbital plate, a corresponding advancement was carried out on the flattened side. The orbital segment was repositioned with a slight overcorrection in both the coronal and sagittal planes. The frontal bone was reshaped by microfractures to correct ipsilateral flattening and contralateral frontal bossing. After correction, the frontal bone flap was fixed to the orbit using absorbable microplates. Then, the bilateral temporal bone, parietal bone, and the upper half of the occipital bone were cut in a mosaic manner but not separated from the dura mater and fixed, forming a non-detachable floating bone flap. At this point, the whole head deformity and orbital deformity were improved, and the volume of the skull cavity was expanded. Subgaleal drainage was used and remained in place until the second postoperative day. Wound closure was performed with 4-0 subcutaneous Vicryl sutures (Dermabond, Johnson & Johnson, New Brunswick, NJ, USA). Patients were monitored for 24–48 hours post-operatively in an intensive care unit. To prevent thromboembolism all patients had perioperative thromboprophylaxis with stockings and mechanical compression devices, pharmacological prophylaxis with low molecular weight heparin was routinely started at 48 hours from surgery as per international protocols (6). Hospital discharge was scheduled when intravenous pain medication could be safely withdrawn. A cranial computed tomography (CT) scan was usually performed before the operation, 1 week after the operation, and at the last follow-up.
Measurements
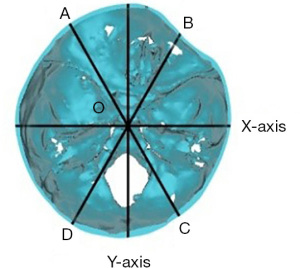
The ACVAI reflects the asymmetric deformity of the anterior cranial fossa and the severity of the oblique head deformity in patients with UCS (7). All patients were imaged with a helical CT scan (General Electric Discovery CT750 HD, General Electric Company, Medical System Group, Milwaukee, WI, USA). Mimics Medical 20.0 software was used to remove unwanted objects, such as the headrest, and to produce 3D reconstructions. The orbital ear axial plane 1 cm above the nasal root was used as the measurement plane. The line between the midpoint of the anterior edge of the foramen magnum and the center of the sella turcica was selected as the X-axis. The vertical line passing through the midpoint O of the X-axis was delineated as the Y-axis. The left and right oblique diameters passing through the O point and the Y-axis at 30° were labeled as BD and AC, respectively. The lengths of the two bisectors AO and BO were used to obtain the index [ACVAI = |AO − BO|/min(AO, BO) × 100%] (Figure 1).
For intracranial volume, the DICOM head CT data were imported into the Mimics Medical 20.0 software for 3D reconstruction. The redundant skin soft tissue and orbital soft tissue were removed layer by layer, and the intracranial soft tissue was retained. The volume of the skull cavity was automatically measured by the software. Tomita et al. measured the intracranial volume of normal boys and girls of different ages and created an intracranial volume curve (8), we used the data from that study as the normal control group to quantitatively analyze the changes in intracranial volume before and after the operation.
Statistical analysis
SPSS Statistics 23.0 software was used to analyze the data. Statistical significance for the ACVAI and cranial volume was estimated by means of a nonparametric, paired t-test with a P value <0.05.
Results
Among the cohort of 20 children, 8 were males and 12 were females. All patients underwent bilateral fronto-orbital advancement combined with anterior CVR + FFBF technique at an average age of 10.45 months (range, 5 to 23 months). The average length of follow-up was 19.9 months (range, 12 to 40 months).
There were no reported major intraoperative or postoperative complications (grade III–V according to Clavien-Dindo classification), such as the need for reoperation or mortality. Furthermore, no patients experienced bone flap necrosis, bone flap displacement, cerebrospinal fluid leakage or wound healing problems.
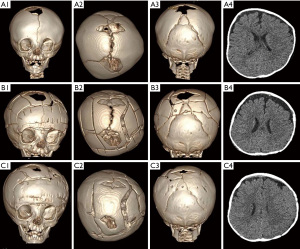
Judging from the CT images, postoperative recovery was well. Preoperative head CT showed premature closure of the left coronal suture, ipsilateral flattening of the frontal and parietal bones, temporal retrusion with elevation and recession of the supraorbital rim, and reduction of the volume of the skull cavity on the affected side (Figure 2A). One week after the operation, the head CT showed that the bilateral orbits were basically symmetrical. The sizes of the bilateral cranial cavities were comparatively the same (Figure 2B). Three months after the operation, the skull CT showed that the floating bone flap space had begun to fuse. No bone flap displacement, necrosis, or orbital invagination was observed. Compared with 1 week after the operation, the flattening of the left frontal, parietal, and occipital bones was significantly corrected (Figure 2C). Compared with preoperative, the skull demonstrated a mosaic appearance 1 week after the operation (Figure 3A,3B). One year after the operation, the head CT showed no recession of the supraorbital rim. Most of the floating bone flap spaces were also fused. The appearance of the bilateral parietal and frontal bone flaps was similarly symmetrical. Two years after the operation, the patients had an improved appearance and bilateral orbital symmetry, the sizes of the bilateral cranial cavities were generally the same, and no recurrence was observed (Figure 3C).

The ACVAI was 9.07%±3.55%, 3.56%±3.42%, and 3.13%±2.41% before the operation, 1 week after the operation, and at the last follow-up, respectively. The ACVAI value 1 week after the operation was significantly lower than that before the operation (t=4.827, P<0.001). No significant difference was found in the ACVAI between the last follow-up and 1 week after the operation (t=0.660, P=0.517).
The intracranial volumes of the treatment group and the normal control group were 1,027.85±112.25 and 1,131.92±161.71 mL, respectively. The intracranial volume of the treatment group was significantly smaller than that of the normal control group (t=2.364, P=0.023). One week after the operation, the intracranial volume was 1,081.62±111.10 mL, which was significantly greater than that before the operation (t=8.703, P<0.001). There was no significant difference when compared with the normal control group (t=1.147, P=0.259). At the last follow-up, the intracranial volumes of the treatment group and the normal control group were 1,386.90±119.30 and 1,438.22±89.28 mL, respectively. There was no significant difference between the two groups (t=1.540, P=0.132) (Figure 4).

Discussion
Single-suture craniosynostosis refers to an isolated premature fusion of one cranial suture: the metopic, sagittal, and right or left coronal and the right or left lambdoid. The overall incidence of single-suture craniosynostosis is approximately 1 in 2,000 live births, although estimates vary (9). UCS occurs at a rate of 1 in 1,000. UCS is often accompanied by a decrease in intracranial volume (10). The data from this group show that unilateral premature closure of the coronal suture causes not only fronto-orbital bony constriction but also occipital bony constriction on the affected side, resulting in the entire cranial cavity of the affected side being smaller than that of the healthy side. Premature fusion results in an abnormally shaped skull and brain. If left uncorrected, there is a progressive worsening of the cranial pathology (bone and brain) during early childhood.
The prevalence of cognitive dysfunction in nonsyndromic craniosynostosis patients is relatively high and manifests primarily in higher-order associative functions, including behavior, language, and visuospatial processing (11). Nonsyndromic craniosynostosis infants have impaired cognitive, motor, and/or language development (12-16). Adolescent (age 6–16 years) reports have shown that approximately 50% of nonsyndromic UCS patients experience significant cognitive and/or executive planning dysfunction (17-24). Kalmar et al. reported that 52% of children with left UCS and 61% of children with right UCS demonstrated a developmental problem related to intelligence, speech, learning, or behavior (11). The mechanism by which the fused suture constricts skull growth during the period of greatest brain volume growth is likely the reason for the observed learning disability in UCS patients. Although preliminary findings decades ago of ICP in nonsyndromic craniosynostosis patients were negative, sensitive and quantitative imaging studies now suggest that ICP effects may, in fact, occur and generate damage to the cortex. Hemodynamic and metabolic study indicate that blood flow and neural metabolism, which are low before surgery, preliminarily appear to improve after vault constriction release, which supports a bony constriction role in nonsyndromic craniosynostosis brain insult and dysfunction (25).
The surgical treatments for UCS have evolved over decades. The primary treatment options include fronto-orbital advancement procedures, release operations along with springs or distractors, and endoscopic surgery followed by helmet therapy. The shortcomings of fronto-orbital advancements are mainly believed to be due to the relatively limited increase in intracranial volume. A high rate of recurrent intracranial hypertension, necessitating secondary cranial vault expansion procedures, has been demonstrated. Endoscopic suturectomy combined with helmet correction after surgery causes little trauma; its disadvantages are that the forehead and orbital deformities are not shaped, and the surgical effect is limited and frequent to relapse (26-28). Because endoscopic suturectomy does not typically extend into the frontosphenoidal suture along the cranial base, optimal results are achieved if endoscopic suturectomy is performed before this suture fuses, ideally, before 3 months of age but no later than 5 months (29). Sugawara used a multidirectional cranial distraction osteogenesis technique for treating bicoronal synostosis. The feasibility of this technique has been confirmed, and the trauma of this technique is less than that of fronto-orbital advancement. The disadvantages are the risk of infections of the percutaneous hardware and the requirement of a second craniotomy for removal (30).
This study of patients with UCS demonstrated favorable outcomes in intracranial volume expansion and fronto-orbital symmetry. The intracranial volume 1 week after the operation was significantly increased compared with that before the operation, and the intracranial volume at the later follow-up was close to that of normal children. The ACVAI value 1 week after the operation was significantly lower than that before the operation (t=4.827, P<0.001). No significant difference was found in the ACVAI between the last follow-up and 1 week after the operation.
We opted for the more rapid release of pressure through bilateral fronto-orbital advancement combined with the FFBF technique. To achieve a large increase in intracranial volume, we not only expanded the anterior cranial cavity by bilateral fronto-orbital advancement but also expanded the middle cranial cavity by CVR, in which the bilateral temporal bone, parietal bone and the upper half of the occipital bone were cut in a mosaic manner, forming a non-detachable FFBF.
The mechanism of free-floating CVR is based on the fact that the brain tissue of children under 2–3 years old is in a stage of rapid development (31,32). When the large deformed skull that compresses the brain is cut into small pieces, the pressure on the brain tissue is immediately relieved. With the natural expansion of the brain, the shape of the skull is improved. In addition to correcting calvarial morphology, the CVR + FFBF may also allow for an enlarged cranial cavity and more normalized brain growth. By relieving bony constrictive forces on the brain early in life, surgery may reduce the possibility of recurrence and attenuate the cognitive dysfunction reported later in life (33). In addition, we found abnormal hyperplasic lesser wings of the skull base on the affected side during the operation. Resection of these abnormal hyperplasic lesser wings could help to achieve an increase in intracranial volume. Intraoperative overcorrection of fronto-orbital deformities can achieve better postoperative results and avoid postoperative deformity recurrence (34). No bone traction or helmet fixation was necessary with our treatment. Overall, our study demonstrates that more comprehensive surgical release offers favorable outcomes in intracranial volume expansion and fronto-orbital symmetry. A more comprehensive surgical release may offer better neurodevelopment and cognitive functioning outcomes later in life.
Limitations and future research
Despite the encouraging results, the number of cases selected for enrollment in our study was small; furthermore, neurodevelopmental outcomes were not assessed. Going forward, well-powered, multicenter long-term studies are certainly warranted by the encouraging results described above. The quest for more tailored surgical planning of children with craniosynostosis might also lead to the consideration for the use of gradient echo black-bone and zero time echo magnetic resonance imaging (MRI) sequences (35) in the diagnostic and treatment stages to significantly reduce the exposure to ionizing radiation and facilitate the preparation for challenging calvarial remodeling such as that described in this study.
Conclusions
For the treatment of UCS, the choice of bilateral fronto-orbital advancement combined with CVR + FFBF technique offers favorable outcomes both in terms of expansion of intracranial volume and achievement of an optimal fronto-orbital symmetry. The appearance and functional outcomes provided by such surgical strategy allow making a strong call for the adoption of CVR + FFBF in challenging craniofacial cases due to nonsyndromic UCS.
Acknowledgments
Mr. M.G.’s contribution to this article was made in the context of the Oxford Global Neurosurgery Initiative.
Funding: This work was supported by a grant from
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-495/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-495/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-495/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-495/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Shanghai Children’s Medical Center Review Board (No. SCMCIRB-K2022035-1). Written consent was obtained from patients’ parents or guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bellaire CP, Devarajan A, Napoli JG, et al. Craniofacial Dysmorphology in Infants With Non-Syndromic Unilateral Coronal Craniosynostosis. J Craniofac Surg 2022;33:1903-8. [Crossref] [PubMed]
- Tamburrini G, Caldarelli M, Massimi L, et al. Intracranial pressure monitoring in children with single suture and complex craniosynostosis: a review. Childs Nerv Syst 2005;21:913-21. [Crossref] [PubMed]
- Ganau M, Magdum SA, Calisto A. Pre-operative imaging and post-operative appearance of standard paediatric neurosurgical approaches: a training guide for neuroradiologists. Transl Pediatr 2021;10:1231-43. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Rangel SJ, Kelsey J, Colby CE, et al. Development of a quality assessment scale for retrospective clinical studies in pediatric surgery. J Pediatr Surg 2003;38:390-6; discussion 390-6. [Crossref] [PubMed]
- Chibbaro S, Cebula H, Todeschi J, et al. Evolution of Prophylaxis Protocols for Venous Thromboembolism in Neurosurgery: Results from a Prospective Comparative Study on Low-Molecular-Weight Heparin, Elastic Stockings, and Intermittent Pneumatic Compression Devices. World Neurosurg 2018;109:e510-6. [Crossref] [PubMed]
- Yin H, Dong X, Yang B. A new three-dimensional measurement in evaluating the cranial asymmetry caused by craniosynostosis. Surg Radiol Anat 2015;37:989-95. [Crossref] [PubMed]
- Tomita Y, Kameda M, Senoo T, et al. Growth Curves for Intracranial Volume and Two-dimensional Parameters for Japanese Children without Cranial Abnormality: Toward Treatment of Craniosynostosis. Neurol Med Chir (Tokyo) 2022;62:89-96. [Crossref] [PubMed]
- Singer S, Bower C, Southall P, et al. Craniosynostosis in Western Australia, 1980-1994: a population-based study. Am J Med Genet 1999;83:382-7. [Crossref] [PubMed]
- Morris L. Management of Craniosynostosis. Facial Plast Surg 2016;32:123-32. [Crossref] [PubMed]
- Kalmar CL, Lang SS, Heuer GG, et al. Neurocognitive outcomes of children with non-syndromic single-suture craniosynostosis. Childs Nerv Syst 2022;38:893-901. [Crossref] [PubMed]
- Da Costa AC, Anderson VA, Holmes AD, et al. Longitudinal study of the neurodevelopmental characteristics of treated and untreated nonsyndromic craniosynostosis in infancy. Childs Nerv Syst 2013;29:985-95. [Crossref] [PubMed]
- Osborn AJ, Roberts RM, Dorstyn DS, et al. Sagittal Synostosis and Its Association With Cognitive, Behavioral, and Psychological Functioning: A Meta-analysis. JAMA Netw Open 2021;4:e2121937. [Crossref] [PubMed]
- Collett BR. Heterogeneity in Neurodevelopmental Outcomes Associated With Isolated Sagittal Craniosynostosis. JAMA Netw Open 2021;4:e2122991. [Crossref] [PubMed]
- Korpilahti P, Saarinen P, Hukki J. Deficient language acquisition in children with single suture craniosynostosis and deformational posterior plagiocephaly. Childs Nerv Syst 2012;28:419-25. [Crossref] [PubMed]
- Speltz ML, Kapp-Simon KA, Cunningham M, et al. Single-suture craniosynostosis: a review of neurobehavioral research and theory. J Pediatr Psychol 2004;29:651-68. [Crossref] [PubMed]
- Stanton E, Urata M, Chen JF, et al. The clinical manifestations, molecular mechanisms and treatment of craniosynostosis. Dis Model Mech 2022;15:dmm049390. [Crossref] [PubMed]
- Osborn AJ, Roberts RM, Mathias JL, et al. Cognitive, behavioral and psychological functioning in children with metopic synostosis: a meta-analysis examining the impact of surgical status. Child Neuropsychol 2019;25:263-77. [Crossref] [PubMed]
- Bottero L, Lajeunie E, Arnaud E, et al. Functional outcome after surgery for trigonocephaly. Plast Reconstr Surg 1998;102:952-8; discussion 959-60.
- Collett BR, Kapp-Simon KA, Wallace E, et al. Attention and executive function in children with and without single-suture craniosynostosis. Child Neuropsychol 2017;23:83-98. [Crossref] [PubMed]
- Kapp-Simon KA, Speltz ML, Cunningham ML, et al. Neurodevelopment of children with single suture craniosynostosis: a review. Childs Nerv Syst 2007;23:269-81. [Crossref] [PubMed]
- Kapp-Simon KA, Wallace E, Collett BR, et al. Language, learning, and memory in children with and without single-suture craniosynostosis. J Neurosurg Pediatr 2016;17:578-88. [Crossref] [PubMed]
- Kelleher MO, Murray DJ, McGillivary A, et al. Behavioral, developmental, and educational problems in children with nonsyndromic trigonocephaly. J Neurosurg 2006;105:382-4. [Crossref] [PubMed]
- Sidoti EJ Jr, Marsh JL, Marty-Grames L, et al. Long-term studies of metopic synostosis: frequency of cognitive impairment and behavioral disturbances. Plast Reconstr Surg 1996;97:276-81. [Crossref] [PubMed]
- Brooks ED, Beckett JS, Yang J, et al. The Etiology of Neuronal Development in Craniosynostosis: A Working Hypothesis. J Craniofac Surg 2018;29:49-55. [Crossref] [PubMed]
- Barone CM, Jimenez DF. Endoscopic craniectomy for early correction of craniosynostosis. Plast Reconstr Surg 1999;104:1965-73; discussion 1974-5. [Crossref] [PubMed]
- Bir SC, Ambekar S, Notarianni C, et al. Odilon Marc Lannelongue (1840-1911) and strip craniectomy for craniosynostosis. Neurosurg Focus 2014;36:E16. [Crossref] [PubMed]
- Sauerhammer TM, Seruya M, Ropper AE, et al. Craniectomy gap patency and neosuture formation following endoscopic suturectomy for unilateral coronal craniosynostosis. Plast Reconstr Surg 2014;134:81e-91e. [Crossref] [PubMed]
- Isaac KV, MacKinnon S, Dagi LR, et al. Nonsyndromic Unilateral Coronal Synostosis: A Comparison of Fronto-Orbital Advancement and Endoscopic Suturectomy. Plast Reconstr Surg 2019;143:838-48. [Crossref] [PubMed]
- Sunaga A, Sugawara Y, Gomi A, et al. Multidirectional cranial distraction osteogenesis technique for treating bicoronal synostosis. J Craniomaxillofac Surg 2019;47:1436-40. [Crossref] [PubMed]
- Iwasaki N, Hamano K, Okada Y, et al. Volumetric quantification of brain development using MRI. Neuroradiology 1997;39:841-6. [Crossref] [PubMed]
- Reiss AL, Abrams MT, Singer HS, et al. Brain development, gender and IQ in children. A volumetric imaging study. Brain 1996;119:1763-74. [Crossref] [PubMed]
- Bao N, Chu J, Wang X, et al. Extensive cranioplasty for sagittal synostosis in young children by preserving multiple cranial bone flaps adhered to the dura mater: experience with 63 cases. Zhonghua Zheng Xing Wai Ke Za Zhi 2016;32:9-13.
- Engel M, Castrillon-Oberndorfer G, Hoffmann J, et al. Long-term results in nonsyndromatic unilateral coronal synostosis treated with fronto-orbital advancement. J Craniomaxillofac Surg 2013;41:747-54. [Crossref] [PubMed]
- Ganau M, Syrmos NC, Magdum SA. Imaging in Craniofacial Disorders With Special Emphasis on Gradient Echo Black-Bone and Zero Time Echo MRI Sequences. J Pediatr Neurosci 2022;17:S14-20. [Crossref] [PubMed]


