Laparoscopy or retroperitoneoscopy: which is the best approach in pediatric urology?
Introduction
Minimally invasive surgery has gained popularity in the last two decades due to numerous advantages. Compared to the adult population, the application of this approach in the pediatric population was somewhat delayed (1). Since then, minimally invasive surgery (MIS) has evolved and made remarkable progress. Its use in pediatric urology has revolutionized the diagnosis and treatment of many diseases. Two approaches have been described until now in this context: transperitoneal laparoscopy and retroperitoneoscopy. Both techniques have been used on children for a wide range of urological procedures such as in inguinal, renal, adrenal, upper and lower urinary tract surgery. However, few studies have been conducted concerning the comparison of these two approaches. This report aims to provide a review of the literature comparing the two minimally invasive surgical approaches in each of the above-mentioned topics of pediatric urology.
Inguinal surgery
Varicocele
For many years, the most popular technique for the treatment of varicocele in childhood has been the mass ligation of testicular vessels in the retroperitoneum above the internal ring (Palomo technique). Other techniques such as embolization, sclerotherapy and microsurgery have been described without great acceptance. Approximately 20 years ago, the laparoscopic repair of varicocele made its debut. The laparoscopic method was similar to the open technique, but many suggested only vein ligation and preservation of lymphatics to avoid testicular atrophy and postoperative hydrocele, respectively. Reduced operative time, decreased rate of complications, shorter hospital stay and improved cosmetic results are just some of the advantages of laparoscopic varicocelectomy (2), as confirmed by many authors. Podkamenev et al. underlined the reduced use of postoperative analgesia in the laparoscopic group (3) and Koyle et al. reported growth in 82% of testicles at one year with this method (4). In recent studies, the rate of hydrocele formation ranges between 0 and 2% (5). Similarly, the rates of recurrence are negligible.
In 2003, Valla et al. described the retroperitoneal approach for the treatment of varicocele (6). Using only one trocar, they performed 80 varicocelectomies with the lymphatic-sparing Palomo technique. The success rate was 94%, while the percentage of recurrence and hydrocele formation was 6% and 8%, respectively. No testicular atrophy was noted. The authors underlined the advantages of this approach that included the short operative time and feasibility of the anatomy (7). However, in another study conducted by Cobellis et al. the conversion rate was 17% (8).
Adrenal surgery
Adrenalectomy
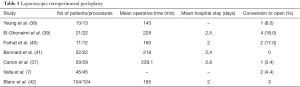
Experience regarding the application of minimally invasive methods in the treatment of pediatric oncological patients is limited. Laparoscopy is indicated for diagnostic and therapeutic purposes. Laparoscopic adrenalectomy can be performed safely and effectively in most cases, providing the advantages of laparoscopy such as short hospital stay, minimal blood loss, rapid recovery and excellent outcome (2). Many series (Table 1) have shown the efficacy and success of laparoscopy in adrenalectomy (9-13). On the other hand, retroperitoneoscopy does not allow visualization of the whole abdominal cavity. Furthermore, the limited working space makes extraction of the tumor impossible without fragmentation. Thus, the implementation of retroperitoneoscopy is limited to small-sized and benign tumors (7).
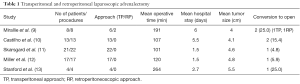
Full table
Renal surgery
Total nephrectomy
Total nephrectomy is indicated in children with non-functional kidneys. The etiology may be vesicoureteric reflux, obstructive uropathy, dysplasia and ectopic insertion of ureter. In recent years, the gold standard technique is laparoscopic nephrectomy using either transperitoneal or retroperitoneal approaches. Furthermore, retroperitoneoscopy can be performed with the patient in lateral or prone position. The first pediatric laparoscopic nephrectomy was described in 1993 by Das et al. (14). Since then, several studies (15) have shown the efficacy of each method (Table 2).
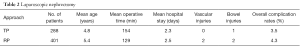
Full table
Gundeti et al. presented their experience of 100 consecutive laparoscopic nephrectomies, comparing the transperitoneal and posterior prone retroperitoneoscopic (PPR) approaches (16). They found no statistical difference in hospital stay (mean duration:1.5 day) or in the use of analgesics. The operative time in the transperitoneal group was significantly longer by comparison (112 vs. 96 min in PPR group) and the overall rate of complications was 6%. Conversion to open surgery was needed in one child in each group. They concluded that both methods can be applied in children, but the PPR approach has the added advantage of using two trocars instead of three and is more suitable in patients who require bilateral nephrectomy. Al-Hazmi et al. reported their experience in 35 patients who underwent laparoscopic lateral retroperitoneoscopic nephrectomy, the results of which were similar to those of previous studies (17). Valla et al. presented their first 100 cases of retroperitoneoscopic lateral nephrectomy. Their findings were consistent with those reported by other series. However, they underlined that the retroperitoneoscopic approach may not be suitable in cases where the ureter must be dissected near the ureterovesical junction or in cases of previous kidney inflammation, anatomical variations of the kidney and in children who require bilateral nephrectomy (7).
Partial nephrectomy, heminephrectomy and nephroureterectomy
The main indication for partial nephrectomy or heminephrectomy in children is the excision of a non-functioning upper or lower pole due to complicated duplex anomalies of the kidney. Obstruction and reflux, respectively, are the main reasons for the poor function of the upper and lower pole of the kidney. Transperitoneal laparoscopic partial nephrectomy was initially described by Jordan and Winslow in 1993 (18). Miyazato et al. first reported the retroperitoneal approach in pediatric heminephrectomy in 2000 (19). Since then, both procedures have been applied in children, although the technical difficulties that emerged, especially among the retroperitoneal group, inhibited their widespread use. Proponents of the transperitoneal approach disagreed that this method was easier to perform due to clearer anatomic views. On the other hand, direct access to renal vessels without violating the peritoneal cavity was the main advantage of the lateral or prone retroperitoneal method. Borzi and Yeung also advocated that the lateral position in retroperitoneoscopy is indicated in cases of ectopic kidneys and extended ureterectomy (20). Many series have proved the efficacy and disadvantages of each method (Table 3). It is important to note that in all patients, a ureteral catheter was placed preoperatively by cystoscopy in the ureter of healthy moiety in order to facilitate its recognition and avoid any inadvertent injury. In the majority of children, the dissection of parenchyma was made with the aid of specific hemostatic devices.
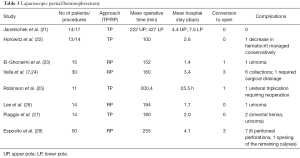
Full table
Esposito et al. compared laparoscopic and retroperitoneoscopic approaches regarding partial nephrectomy in the pediatric population (29). In this survey, 102 patients were recorded, of whom 52 underwent transperitoneal partial nephrectomy. The authors found significant statistical differences between the two groups regarding operative time (laparoscopic: 166.2 vs. retroperitoneoscopic: 255 min) and hospitalization (laparoscopic: 3.5 vs. retroperitoneoscopic: 4.1 days). No procedure was converted to open surgery and no deterioration in kidney function was noted for either group. However, it is remarkable that complications were fewer in the transperitoneal (19%) than in the retroperitoneoscopic group (30%). In the transperitoneal group, four urinomas, four urinary leakages and two symptomatic refluxing distal ureteral stumps were recorded, all of which were managed conservatively. In the retroperitoneoscopic group, six urinomas, one opening of remaining calyxes and eight symptomatic refluxing distal ureteral stumps were reported; reoperation was necessary in two patients in whom cyst and collection formation developed postoperatively. The authors recommended the transperitoneal approach for partial nephrectomy due to the facility and safety of the method. The larger working space and the ability to perform a complete ureterectomy in the case of complications are among the main advantages of the laparoscopic approach.
Dismembered pyeloplasty
The last two decades have witnessed a trend toward minimally invasive techniques in the treatment of pyeloureteral junction obstruction in children. In 1995, Peters et al. introduced laparoscopic pyeloplasty in the pediatric population (30). Although both the transperitoneal and retroperitoneal approaches have been used, few comparative studies have been published. Several articles have published the individual results from the application of each method (Tables 4,5).
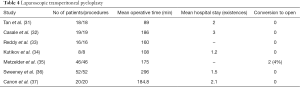
Full table
Full table
Based on the data collected, it is important to underline certain critical points. Valla et al. noted the longer laparoscopic time involved and the technical difficulties encountered in the retroperitoneoscopic group. The advantages of minimally invasive surgery are evident only in patients older than 6 years of age. As concerns the cosmetic result, the authors found the retroperitoneoscopic method superior to the transperitoneal approach (7).
Blanc et al. placed patients over one year of age in the lateral retroperitoneal position. Infants under this age underwent open Hynes-Anderson pyeloplasty. According to their strategy, the transperitoneal approach was applied in children of all ages with pelvic or horseshoe kidney or in patients who required a reoperation. A statistically significant reduction in operative time was reported after the first 35 cases, which most likely reflects the learning curve for standardization of the technique. Although the transperitoneal method provides larger working space, the authors advocated that retroperitoneoscopy reduces the risk of intra-abdominal injury and renders access to the urinary tract easier and faster. Concerning the success rates, they found no difference in the transperitoneal method compared to the open approach (42).
Abraham et al. suggested the semi-prone position of the patient in retroperitoneoscopic pyeloplasty due to better exposure (43).
Canon et al. presented similar results comparing retroperitoneoscopic and laparoscopic dismembered pyeloplasty. No major complications were recorded and no difference was noted in analgesic requirements between the two methods. They concluded that the two techniques are comparable (37).
In 2011, Bird et al. compared 172 pyeloplasties, of which 98 were performed with the retroperitoneoscopic method and 74 with the laparoscopic approach. Both complications and outcome were similar for the two groups (44). In 2013, Riachy et al. (45) analyzed the data from 18 laparoscopic and 46 retroperitoneoscopic pyeloplasties. The mean age of the patients was eight years. Unlike other studies, the operation duration was statistically longer in the transperitoneal group (298 vs. 209 min).
Urolithiasis
Minimally invasive surgery presents an alternative in the treatment of pediatric urolithiasis. Both transperitoneal and retroperitoneal laparoscopic techniques have been used for urinary stone removal. In many instances, it has replaced conventional methods such as percutaneous nephrolithotomy, ureteroscopy, extracorporeal shock wave lithotripsy and most importantly open surgery. These methods have the advantage not only of stone removal, but also of allowing the surgeon the opportunity to treat a concomitant congenital anomaly at the same operative time.
Valla et al. operated on three patients using the retroperitoneoscopic approach (7). The procedures adopted by the authors were nephrolithotomy and pyelolithotomy for caliceal diverticulum and cystinic stone, respectively. It is important to note that in all cases, surgeons simultaneously managed the coexistence of an aberrant renal vessel.
A multicentric survey was conducted by Fragoso et al. in 2009 (46). This study proved the efficacy and safety of minimal invasive surgery in the management of urolithiasis in selected pediatric patients. Specifically, fifteen children underwent minimal invasive surgery for diagnosed urolithiasis that could not be managed with the other mentioned techniques. Six retroperitoneal and eleven transperitoneal (seven with suprapubic approach) procedures were performed and analyzed. In five patients, surgeons corrected a coexisting urologic abnormality. The success rate of these techniques reached 82%. In their opinion, the authors proposed the retroperitoneoscopic lateral approach for nephro- and pyelolithotomy, while suggesting the transperitoneal approach (with three trocars) for ureterolithotomy.
Discussion
Since making its first appearance, minimally invasive surgery has been very quickly adopted by the surgical community. The advantages of MIS, including less postoperative pain, rapid recovery, the reduced risk of adhesive formation and excellent cosmetic results, have nowadays established it as common surgical practice. General surgeons were the first to adopt this technique, and were later followed by pediatric surgeons. One of the reasons for the delay in its implementation in children was the lack of appropriate laparoscopic devices for pediatric patients. However, the revolution in technology eventually overcame this difficulty.
In this context, first laparoscopy and then retroperitoneoscopy were developed. Their usefulness in pediatric surgery, especially in pediatric urology, was quickly recognized and accepted. Initially, both techniques were used for diagnostic purposes in pediatric urology, but their application was soon to pass into the therapeutic field. The familiarization of pediatric surgeons with laparoscopic devices rendered laparoscopy the most attractive method. On the other hand, urologists seemed to prefer retroperitoneoscopy due to the better knowledge of the anatomy of the urinary tract system. Nevertheless, both accesses hold their position of worth in pediatric surgery in the management of a wide range of urological diseases.
Nowadays, the gold standard for surgical repair of varicocele in adolescents is the lymphatic-sparing laparoscopic Palomo technique. The effectiveness of this method has been proved by many series. Short hospitalization, decreased rates of postoperative hydrocele formation and recurrence are just some of the benefits of this technique. Valla et al. and Cobellis et al. presented their findings using the retroperitoneoscopic access for the management of varicocele. Although the results were encouraging, the small number of patients does not allow safe conclusions to be drawn.
Minimally invasive techniques have become more popular in the field of oncology in the last fifteen years. Experience remains limited in children and their use lies mainly in the diagnosis and treatment of small, localized and benign tumors. Adrenalectomy is the most commonly performed procedure in children using either laparoscopy or retroperitoneoscopy. Comparing the two approaches, transperitoneal laparoscopy provides larger working space, allowing examination of the entire abdominal cavity. Retroperitoneoscopy has a limited range of applications, one of which is renal biopsy (47).
Nowadays, minimally invasive surgery for pediatric nephrectomies is established as routine practice. Transperitoneal and retroperitoneal are the two approaches for performing either total or partial nephrectomy. Transperitoneal laparoscopy can be performed in most cases using three trocars and the patient is placed in lateral position. In order to expose the right kidney, the surgeon must mobilize the hepatic flexure of the colon, while on the left side the splenic flexure and/or the spleen needs to be mobilized. This approach is easier compared to retroperitoneoscopy since it allows plenty of space, but it has an inherent risk of adhesion formation.
Retroperitoneoscopy can be accomplished placing the patient in lateral or prone position. This technique requires experience to find the way to the retroperitoneum. The main landmark during surgery is the psoas muscle. The prone approach is very versatile because it gives the surgeon the chance to reach the adrenal gland and the upper and lower urinary tract, and also allows a bilateral procedure to be achieved. Furthermore, this access leaves the kidney in place and has the advantage of a direct approach to the vessels. On the other hand, it is not the best option when mobilization of the lower ureter and urgent conversion are needed.
From the technical aspect, we should stress that in total nephrectomy the kidney must be left attached to the peritoneum until vessel division. Most surgeons recommend ureteric dissection down to the bladder in order to avoid problems with the stump postoperatively. Generally speaking, total nephrectomy is considered a simple procedure, though not in cases of small infants, recent pyelonephritis, or in the presence of massively dilated upper tract. The main principle in partial nephrectomies is to understand the anatomy of the area before doing anything. In addition, the learning curve for partial nephrectomy seems to be greater than that for total nephrectomy.
In pediatric urology, there is a shift toward the transperitoneal approach for difficult procedures such as partial nephrectomies. Comparing lateral or prone retroperitoneoscopy with the transperitoneal approach, many series detected significant differences in terms of ease of access and dissection, available working space and conversion rates. Faster access and easier dissection can be achieved with the retroperitoneal prone approach. Although gravity enlarges the space available with this method, transperitoneal laparoscopy remains the technique that ensures the best working field. Conversion to open surgery among the three groups has not reached a significant statistical difference.
Establishing the indications for using one or the other access in total and partial nephrectomy, we recommend that the retroperitoneal lateral approach be applied in straightforward cases. When bi-nephrectomy is needed, the retroperitoneal prone approach is the best option. Transperitoneal laparoscopy seems to be more appropriate for difficult and oncological cases. In uncomplicated cases of partial nephrectomy, retroperitoneoscopy is indicated while in specific situations, one should consider transperitoneal access.
Even now, open Hynes-Anderson pyeloplasty is the surgery of choice for senior residents and fellows in the treatment of ureteropelvic junction obstruction. Laparoscopic pyeloplasty is seen as a demanding procedure to be considered by senior and junior consultants. Both the transperitoneal and retroperitoneal approach have been established for laparoscopic pyeloplasty.
Transperitoneal pyeloplasty is most popular due to the available working space. In addition, it is considered appropriate for all cases. However, it is more painful in cases of leakage and is a very demanding procedure since a long suture line is required. The success rate of this access reaches 95%. As concerns technical details, an extra mesenteric route is preferable to a transmesenteric, so as to avoid the formation of adhesions and additional suturing. There is no contraindication for transperitoneal approach other than the event in which the renal pelvis is hidden deep in the parenchyma. In such a situation, the retroperitoneal approach is probably more suitable. The transperitoneal access is considered preferable to retroperitoneoscopy in children aged under two years, in obese patients, in the presence of anatomic variations and when a reoperation is required. Reduced operative time and lower conversion rates are some of the advantages of transperitoneal laparoscopy versus retroperitoneal.
The retroperitoneal lateral approach for the repair of ureteropelvic junction obstruction is also an acceptable method. With regard to the technique, it is vital to underline that the key points of pyeloplasty are the traction sutures and identification of the most dependent point of the lower pole. The most important landmark during surgery is the psoas muscle. According to the majority of studies, urinary diversion, usually with an external stent, is only needed in severe hydronephrosis, in older children and in the case of redo surgery. The cosmetic result is superior in retroperitoneoscopy and the need for reoperation is also reduced in comparison with the transperitoneal approach. The duration of hospital stay is approximately the same for both groups, but the learning curve is greater in retroperitoneoscopy.
In summary, the authors advocate the following proposed algorithm for the treatment of ureteropelvic junction obstruction. In infants under 1 year of age, posterior lombotomy is the safest approach, while lateral retroperitoneoscopy is preferable when anatomical anomalies coexist. In children over 1 year of age, lateral retroperitoneal laparoscopy is the intended method. In the presence of an ectopic pelvic or horseshoe kidney or in the case of redo surgery, transperitoneal laparoscopy is the suggested technique.
Despite the fact that in the majority of the patients with urinary tract stone disease, the first choice of treatment is non-surgical and includes modalities such as extracorporeal shock wave lithotripsy, percutaneous nephrolithotomy and ureteroscopy, surgical removal of stones is required in many cases. Minimally invasive techniques may substitute both the classic open approach in some instances with similar efficacy and the above-mentioned methods of treatment. The lack of technical equipment and specialization in endoscopic treatments and the possible presence of stones in the bladder may be indications for the application of MIS.
Furthermore, laparoscopy and retroperitoneoscopy allow the surgeon to simultaneously repair concomitant urological abnormalities such as calyceal diverticulum, obstructive megaureter and ureteropelvic junction obstruction. On the other hand, large renal and bladder stones may be a problem in laparoscopy. In nephrolithotomy and pyelolithotomy, the retroperitoneoscopic lateral access provides better exposure than the transperitoneal approach. Conversely, transperitoneal access seems to be a better option when ureterolithotomy is anticipated.
In conclusion, both laparoscopy and retroperitoneoscopy have their own advantages and drawbacks. Both techniques have their own place in the treatment of urological diseases. Consequently, the dilemma which of the two is better does not exist. At the start of their career, surgeons should be trained and acquire familiarity with both approaches. Only in this way will the surgeon be in a position to evaluate and select the appropriate method for each case.
Acknowledgements
The authors thank Mrs. Gina St John for language editing assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Colodny AH. Laparoscopy in pediatric urology: too much of a good thing? Semin Pediatr Surg 1996;5:23-9. [PubMed]
- Smaldone MC, Polsky E, Ricchiuti DJ, et al. Advances in pediatric urologic laparoscopy. ScientificWorldJournal 2007;7:727-41. [Crossref] [PubMed]
- Podkamenev VV, Stalmakhovich VN, Urkov PS, et al. Laparoscopic surgery for pediatric varicoceles: Randomized controlled trial. J Pediatr Surg 2002;37:727-9. [Crossref] [PubMed]
- Koyle MA, Oottamasathien S, Barqawi A, et al. Laparoscopic Palomo varicocele ligation in children and adolescents: results of 103 cases. J Urol 2004;172:1749-52; discussion 1752.
- Kocvara R, Dvorácek J, Sedlácek J, et al. Lymphatic sparing laparoscopic varicocelectomy: a microsurgical repair. J Urol 2005;173:1751-4. [Crossref] [PubMed]
- Valla JS. Retroperitoneoscopic Varicocelectomy in Children and Adolescents. In: Caione P, Kavoussi LR, Micali F. editors. Retroperitoneoscopy and Estraperitoneal Laparoscopy in Pediatric and Adult Urology. Milan: Springer, 2003:163-72.
- Valla JS. Retroperitoneoscopic surgery in children. Semin Pediatr Surg 2007;16:270-7. [Crossref] [PubMed]
- Cobellis G, Mastroianni L, Cruccetti A, et al. Retroperitoneoscopic varicocelectomy in children and adolescents. J Pediatr Surg 2005;40:846-9. [Crossref] [PubMed]
- Mirallié E, Leclair MD, de Lagausie P, et al. Laparoscopic adrenalectomy in children. Surg Endosc 2001;15:156-60. [Crossref] [PubMed]
- Castilho LN, Castillo OA, Dénes FT, et al. Laparoscopic adrenal surgery in children. J Urol 2002;168:221-4. [Crossref] [PubMed]
- Skarsgard ED, Albanese CT. The safety and efficacy of laparoscopic adrenalectomy in children. Arch Surg 2005;140:905-8; discussion 909. [Crossref] [PubMed]
- Miller KA, Albanese C, Harrison M, et al. Experience with laparoscopic adrenalectomy in pediatric patients. J Pediatr Surg 2002;37:979-82; discussion 979-82. [Crossref] [PubMed]
- Stanford A, Upperman JS, Nguyen N, et al. Surgical management of open versus laparoscopic adrenalectomy: outcome analysis. J Pediatr Surg 2002;37:1027-9. [Crossref] [PubMed]
- Das S, Keizur JJ, Tashima M. Laparoscopic nephroureterectomy for end-stage reflux nephropathy in a child. Surg Laparosc Endosc 1993;3:462-5. [PubMed]
- Kim C, McKay K, Docimo SG. Laparoscopic nephrectomy in children: systematic review of transperitoneal and retroperitoneal approaches. Urology 2009;73:280-4. [Crossref] [PubMed]
- Gundeti MS, Patel Y, Duffy PG, et al. An initial experience of 100 paediatric laparoscopic nephrectomies with transperitoneal or posterior prone retroperitoneoscopic approach. Pediatr Surg Int 2007;23:795-9. [Crossref] [PubMed]
- Al-Hazmi HH, Farraj HM. Laparoscopic retroperitoneoscopic nephrectomy and partial nephrectomy in children. Urol Ann 2015;7:149-53. [Crossref] [PubMed]
- Jordan GH, Winslow BH. Laparoendoscopic upper pole partial nephrectomy with ureterectomy. J Urol 1993;150:940-3. [PubMed]
- Miyazato M, Hatano T, Miyazato T, et al. Retroperitoneoscopic heminephrectomy of the right upper collecting system emptying into an ectopic ureterocele in a 5-year-old girl: a case report. Hinyokika Kiyo 2000;46:413-6. [PubMed]
- Borzi PA, Yeung CK. Selective approach for transperitoneal and extraperitoneal endoscopic nephrectomy in children. J Urol 2004;171:814-6; discussion 816. [Crossref] [PubMed]
- Janetschek G, Seibold J, Radmayr C, et al. Laparoscopic heminephroureterectomy in pediatric patients. J Urol 1997;158:1928-30. [Crossref] [PubMed]
- Horowitz M, Shah SM, Ferzli G, et al. Laparoscopic partial upper pole nephrectomy in infants and children. BJU Int 2001;87:514-6. [Crossref] [PubMed]
- El-Ghoneimi A, Farhat W, Bolduc S, et al. Retroperitoneal laparoscopic vs open partial nephroureterectomy in children. BJU Int 2003;91:532-5. [Crossref] [PubMed]
- Valla JS, Breaud J, Carfagna L, et al. Treatment of ureterocele on duplex ureter: upper pole nephrectomy by retroperitoneoscopy in children based on a series of 24 cases. Eur Urol 2003;43:426-9. [Crossref] [PubMed]
- Robinson BC, Snow BW, Cartwright PC, et al. Comparison of laparoscopic versus open partial nephrectomy in a pediatric series. J Urol 2003;169:638-40. [Crossref] [PubMed]
- Lee RS, Retik AB, Borer JG, et al. Pediatric retroperitoneal laparoscopic partial nephrectomy: comparison with an age matched cohort of open surgery. J Urol 2005;174:708-11; discussion 712. [Crossref] [PubMed]
- Piaggio L, Franc-Guimond J, Figueroa TE, et al. Comparison of laparoscopic and open partial nephrectomy for duplication anomalies in children. J Urol 2006;175:2269-73. [Crossref] [PubMed]
- Esposito C, Miyano G, Caione P, et al. Retroperitoneoscopic Heminephrectomy in Duplex Kidney in Infants and Children: Results of a Multicentric Survey. J Laparoendosc Adv Surg Tech A 2015;25:864-9. [Crossref] [PubMed]
- Esposito C, Escolino M, Miyano G, et al. A comparison between laparoscopic and retroperitoneoscopic approach for partial nephrectomy in children with duplex kidney: a multicentric survey. World J Urol 2016;34:939-48. [Crossref] [PubMed]
- Peters CA, Schlussel RN, Retik AB. Pediatric laparoscopic dismembered pyeloplasty. J Urol 1995;153:1962-5. [Crossref] [PubMed]
- Tan HL. Laparoscopic Anderson-Hynes dismembered pyeloplasty in children. J Urol 1999;162:1045-7; discussion 1048. [Crossref] [PubMed]
- Casale P, Grady RW, Joyner BD, et al. Comparison of dismembered and nondismembered laparoscopic pyeloplasty in the pediatric patient. J Endourol 2004;18:875-8. [Crossref] [PubMed]
- Reddy M, Nerli RB, Bashetty R, et al. Laparoscopic dismembered pyeloplasty in children. J Urol 2005;174:700-2. [Crossref] [PubMed]
- Kutikov A, Resnick M, Casale P. Laparoscopic pyeloplasty in the infant younger than 6 months--is it technically possible? J Urol 2006;175:1477-9; discussion 1479. [Crossref] [PubMed]
- Metzelder ML, Schier F, Petersen C, et al. Laparoscopic transabdominal pyeloplasty in children is feasible irrespective of age. J Urol 2006;175:688-91. [Crossref] [PubMed]
- Sweeney DD, Ost MC, Schneck FX, et al. Laparoscopic pyeloplasty for ureteropelvic junction obstruction in children. J Laparoendosc Adv Surg Tech A 2011;21:261-5. [Crossref] [PubMed]
- Canon SJ, Jayanthi VR, Lowe GJ. Which is better--retroperitoneoscopic or laparoscopic dismembered pyeloplasty in children? J Urol 2007;178:1791-5; discussion 1795.
- Yeung CK, Tam YH, Sihoe JD, et al. Retroperitoneoscopic dismembered pyeloplasty for pelvi-ureteric junction obstruction in infants and children. BJU Int 2001;87:509-13. [Crossref] [PubMed]
- El-Ghoneimi A, Farhat W, Bolduc S, et al. Laparoscopic dismembered pyeloplasty by a retroperitoneal approach in children. BJU Int 2003;92:104-8; discussion 108. [Crossref] [PubMed]
- Farhat W, Afshar K, Papanikolaou F, et al. Retroperitoneal-assisted laparoscopic pyeloplasty in children: initial experience. J Endourol 2004;18:879-82. [Crossref] [PubMed]
- Bonnard A, Fouquet V, Carricaburu E, et al. Retroperitoneal laparoscopic versus open pyeloplasty in children. J Urol 2005;173:1710-3; discussion 1713.
- Blanc T, Muller C, Abdoul H, et al. Retroperitoneal laparoscopic pyeloplasty in children: long-term outcome and critical analysis of 10-year experience in a teaching center. Eur Urol 2013;63:565-72. [Crossref] [PubMed]
- Abraham MK, Viswanath N, Bindu S, et al. Retroperitoneoscopic Surgery in Children - An Overview. JIMSA 2014;27:108-10.
- Bird VG, Leveillee RJ, Eldefrawy A, et al. Comparison of robot-assisted versus conventional laparoscopic transperitoneal pyeloplasty for patients with ureteropelvic junction obstruction: a single-center study. Urology 2011;77:730-4. [Crossref] [PubMed]
- Riachy E, Cost NG, Defoor WR, et al. Pediatric standard and robot-assisted laparoscopic pyeloplasty: a comparative single institution study. J Urol 2013;189:283-7. [Crossref] [PubMed]
- Fragoso AC, Valla JS, Steyaert H, et al. Minimal access surgery in the management of pediatric urolithiasis. J Pediatr Urol 2009;5:42-6. [Crossref] [PubMed]
- Caione P, Micali S, Rinaldi S, et al. Retroperitoneal laparoscopy for renal biopsy in children. J Urol 2000;164:1080-2; discussion 1083. [Crossref] [PubMed]


