
Ulnar osteotomy between the proximal 1/3 and 1/5 provides a stable radiocapitellar joint in chronic Monteggia fracture
Highlight box
Key findings
• Ulnar osteotomy between the proximal 1/3 and 1/5 appears to provide a much safer and more stable radiocapitellar joint in chronic Monteggia fracture (CMF).
What is known and what is new?
• There is currently no consensus on the selection of the ulnar osteotomy site, and surgeons often choose different osteotomy locations based on their individual preferences.
• To our knowledge, this is the first study quantitatively analyzing the association between ulnar osteotomy position and redislocation in CMF.
What is the implication, and what should change now?
• Despite currently the lack of a unified consensus, we advocate for ulnar osteotomy to be performed within the proximal 1/5 to 1/3 of the ulna, as it is likely to yield a safer and more stable radiocapitellar joint.
Introduction
In 1814, Monteggia fracture-dislocation, which refers to a fracture of the proximal ulna associated with dislocation of the radial head was first described by Giovanni Monteggia (1). Appropriate closed reduction for Monteggia fracture-dislocation in the acute period could result in a better prognosis. However, missed diagnosis is still always encountered which may lead many of these cases to develop into chronic Monteggia fracture (CMF). For CMF cases, even over 3 weeks after injury, the attempt of trying to manage the dislocation by closed reduction may fail (2). Early intervention is urgently required for CMF in children as symptoms deteriorate over time. Even though the treatment strategy of CMF remains controversial, the most widely accepted concept is the open reduction of the radial head associated with an ulnar osteotomy to restore the ulnar length and alignment (3-6). The key determinant of a successful surgery is whether redislocation of the radiocapitellar joint can be avoided. Currently, there are many reported factors including the age of the patients, the interval from the initial injury, the presence of ulnar deformity, insufficient length, or angulation showing a relationship with recurrent dislocation, yet a final conclusion has not been reached (7). Another condition that may result in radial head subluxation/dislocation is multiple hereditary exostoses (MHE). In MHE, the radial head dislocates in the direction of the ulnar bow. In patients with CMF, the radial head dislocation follows the same pattern. Similar to CMF, shortening and angulation deformities of the ulna have been considered factors for radial head dislocation in MHE patients (8). Previous studies have shown that ulnar lengthening is an effective treatment for MHE deformities and the optimal site for ulnar osteotomy appears to be at the proximal 1/3 to 1/4 of the ulna (9). Clinically, we have observed that radial head reduction cannot always be achieved in some children despite successful lengthening and angulation correction of the ulna in CMF. Therefore, we hypothesize that the success of surgery may also depend on the location of the ulnar osteotomy. In this study, we aimed to investigate whether the level of osteotomy is a potential risk factor for radial head redislocation. We present this article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-477/rc).
Methods
Subjects
Consecutive patients with CMF from January 2008 to May 2019 were enrolled in our study. The inclusion criteria were as follows: (I) a history of more than 1 month from the initial injury; (II) ulnar osteotomy and fixed with plates and screws as the surgical strategy; (III) at least 3 years of follow-up. Children with pathological radial head dislocation or congenital diseases, a history of previous surgery, incomplete medical data, or loss of follow-up were excluded. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). The study was approved by the Human Research Ethics Committee at Children’s Hospital of Fudan University (No. 2020528), and informed written consent was obtained from the guardians of all children participating in the study.
Clinical characteristics and treatment procedure
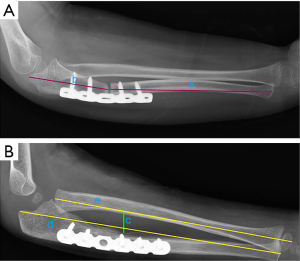
The clinical characteristics of our single-center case series and surgical strategy were described in our previous report (10). The medical records from the latest follow-up were updated and collected. In this study, we introduced a new parameter: proportional ulnar osteotomy (PUO). PUO is defined as the length of proximal part of the ulna divided by the total length of the ulna, which is used to describe the position of ulnar osteotomy (Figure 1A). In addition, we also recorded previously mentioned data like maximum interosseous distance (MID) and proportional ulnar length (PUL) (Figure 1B). The motivation to evaluate PUO stems from our knowledge about MHE, as the best therapeutic effect for reducing the dislocated radial head and improving elbow and wrist mobility is achieved with an osteotomy between the proximal one-third and one-fourth of the ulna (9).
Statistical analysis
General statistical analysis and further receiver operating characteristic (ROC) analysis were performed using software IBM SPSS statistics 20 (IBM SPSS Statistics, Chicago, IL, USA). Continuous variables were presented as mean ± standard deviation if normally distributed and compared by Student t-test, or were presented as median (interquartile range) and compared by Mann-Whitney U test if non-normally distributed. Normal distribution was assessed by use of the Kolmogorov-Smirnov (K-S) test. Categorical variables were presented as absolute numbers or percentages and compared using Pearson Chi-squared test. Predictive performance of PUO range and other characteristics were assessed by the ROC curves. Area under the ROC curve (AUC) was measured and compared using Delong’s test to evaluate the discriminatory power as well as the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with a 95% confidence interval (CI). Statistical significance was defined as a value of P<0.05.
Results
Patients’ baseline characteristics
Patients’ characteristics are summarized in Table 1. A total of 18 children (boy/girl: 15/3, age: 6.8±2.7 years) were enrolled in this study. According to the Bado classification, all patients were classified as type I. Among the patients, 8 (44.44%) had repositioned annular ligaments, while 10 (55.56%) had excised scar tissues without any reconstruction. Notably, three patients experienced nonunion after more than 6 months of follow-up, despite a mean ulnar lengthening of 1.52 cm and a mean angulation of 22.54°. Subsequently, reoperation and autogenous cancellous iliac crest bone graft insertion were performed. Eventually, the osteotomy site healed successfully. Two patients exhibited symptoms of radial nerve issues, which resolved several months later after surgery. In terms of the final reduction outcome, a good reduction (reduced group) was observed in 15 (83.33%) patients, while 3 (16.67%) patients had fair outcomes (redislocation group). The mean osteotomy angle was 12.88°±7.76°, and the mean amount of ulnar lengthening was 9.78±3.77 mm.
Table 1
| Characteristics | Data |
|---|---|
| Age (years), mean ± standard deviation | 6.8±2.7 |
| Sex, n (%) | |
| Boy | 15 (83.33) |
| Girl | 3 (16.67) |
| Injured side, n (%) | |
| Left | 7 (38.89) |
| Right | 11 (61.11) |
| Annular ligament, n (%) | |
| Excised scar tissue | 10 (55.56) |
| Reposition | 8 (44.44) |
| Ulnar osteotomy, n (%) | |
| Proximal site | 18 (100.00) |
| Bone graft, n (%) | |
| Iliac | 14 (77.78) |
| Allograft | 4 (22.22) |
| Final reduction status, n (%) | |
| Good | 15 (83.33) |
| Fair | 3 (16.67) |
| Arthrosis, mean ± standard deviation | |
| Lengthening (mm) | 9.78±3.77 |
| Osteotomy angle (°) | 12.88±7.76 |
Differences between reduced and redislocation group
The distribution of the appropriate PUO range (1/5< PUO <1/3) among patients in reduced group and redislocation group was 13 (86.7%) and 1 (33.3%), respectively, showing a statistically significant difference (P=0.043). There were no statistically significant differences in terms of age, sex, injured side, lengthening, osteotomy angle, post-PUL and post-MID between two groups (Table 2).
Table 2
| Index | Reduced (n=15) | Redislocation (n=3) | P value |
|---|---|---|---|
| Age | 6.73 (5.14, 8.32) | 7.00 (2.70, 11.30) | 0.88 |
| Time interval | 10.70 (2.04, 19.36) | 13.33 (−35.43, 62.10) | 0.8 |
| Lengthening | 10.18 (8.18, 12.18) | 7.77 (−3.91, 19.45) | 0.374 |
| Angle | 14.19 (9.84, 18.55) | 6.33 (2.54, 10.13) | 0.108* |
| Post-PUL | 1.11 (1.08, 1.13) | 1.07 (1.02, 1.13) | 0.12* |
| Post-MID | 1.31 (1.16, 1.46) | 1.21 (1.05, 1.37) | 0.722 |
| PUO | 25.55 (23.16, 27.94) | 26.28 (4.78, 47.77) | 0.767 |
| Sex, n (%) | 0.396 | ||
| Girl | 3 (20.0) | 0 | |
| Boy | 12 (80.0) | 3 (100.0) | |
| Side, n (%) | 0.829 | ||
| Left | 6 (40.0) | 1 (33.3) | |
| Right | 9 (60.0) | 2 (66.7) | |
| PUO range, n (%) | 0.043# | ||
| Appropriate | 13 (86.7) | 1 (33.3) | |
| Inappropriate | 2 (13.3) | 2 (66.7) |
Continuous variables were presented as mean (mean − standard deviation, mean + standard deviation). #, P<0.05; *, P<0.15. PUL, proportional ulnar length; MID, maximum interosseous distance; PUO, proportional ulnar osteotomy.
Predictive performance of predictors
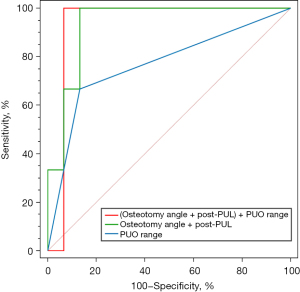
For characteristics with a P value <0.15 between two groups, different models of ROC curves were employed to evaluate the predictive performance of combined characteristics in a stepwise fashion. The AUC of the model of combination of osteotomy angle and post-PUL (0.933, 95% CI: 0.813–1.000, P<0.001) showed no statistical discrepancies with the model combining PUO range, osteotomy angle, and post-PUL (0.933, 95% CI: 0.807–1.000, P<0.001). However, both of these models yielded significantly higher AUC values compared to PUO range alone (0.767, 95% CI: 0.428–1.000, P=0.123) (Table 3). The logistic model involving PUO range, osteotomy angle, and post-PUL enhanced accuracy and specificity in comparison to the model combining only osteotomy angle and post-PUL (without PUO range) (accuracy, 94.44% vs. 83.33%; specificity, 93.33% vs. 86.67%, P=0.008). This indicates that the additive predictive value of PUO range in determining the prognosis of CMF (Figure 2).
Table 3
| Index | AUC (95% CI) | Sensitivity, % (95% CI) |
Specificity, % (95% CI) |
PPV, % (95% CI) |
NPV, % (95% CI) |
Accuracy, % |
|---|---|---|---|---|---|---|
| PUO range | 0.767 (0.428–1.000) |
66.67 (12.53–98.23) |
86.67 (58.39–97.66) |
50.0 (9.19–90.81) |
92.86 (64.17–99.63) |
83.33 |
| Angle + post-PUL | 0.933 (0.813–1.000) |
100.00 (40.00–100.00) |
86.67 (58.39–97.66) |
60.00 (17.04–92.74) |
100.00 (71.66–100.00) |
88.89 |
| Angle + post-PUL + PUO range | 0.933 (0.807–1.000) |
100.00 (40.00–100.00) |
93.33 (66.03–99.65) |
75.00 (21.94–98.68) |
100.00 (73.23–100.00) |
94.44 |
CMF, chronic Monteggia fracture; AUC, area under the curve; CI, confidence interval; PPV, positive predictive value; NPV, negative predictive rate; PUL, proportional ulnar length; PUO, proportional ulnar osteotomy.
Discussion
The diagnosis of Monteggia lesions is difficult and can’t always easily be noticed especially when the radial dislocation is minimal and hidden by the more obvious ulnar fracture. Between 20% and 50% of Monteggia lesions are reported to be initially misdiagnosed, leading to chronic lesions, disabling sequelae and even potential medico-legal consequences (11). In the current series, significant improvement in elbow function was observed; however, successful reduction of the radial head was not achieved in all cases. Radial head redislocation was found in 16.6% (3/18), which is consistent with the results of a meta-analysis that encompassed 30 studies involving 600 patients. This meta-analysis reported radial head reduction was achieved in 83.7% (95% CI, 80.5–86.5%) of the patients (12). Persistent radial head dislocation in CMF may lead to loss of flexion and rotation due to the destruction or malformation of the radial head. Therefore, establishing stable radiocapitellar joint is the key point.
Factors associated with redislocation of CMF have been extensively studied, including age, time from injury to surgery, radial osteotomy, annular ligament repair/reconstruction, radiocapitellar pinning, and restoration of ulnar length and axis. In addition, the controversy remains regarding optimal ulnar osteotomy placement, magnitude, and direction of bony correction, type of fixation, and need for annular ligament repair or reconstruction. The risk factors for recurrent radiocapitellar redislocation vary to a large extent in different studies (4,5,13-18).
Numerous studies, including our previous research, have affirmed the significance of ulnar osteotomy in achieving and maintaining radiocapitellar joint reduction in CMF (10,12). Furthermore, we found that with the prolonged interval from the initial injury, the necessity to increase the lengthening and angulation of the ulna seems more warranted (10). However, regarding the specific level of ulnar osteotomy, we have only previously described the use of proximal osteotomy without quantitative analysis. While several studies have demonstrated that proximal osteotomies contributed to the achievement of a better reduction of radial head, different scholars might prefer alternative positions of osteotomy based on different principles. For instance, Xu et al. conducted open reduction with center of rotation of angulation (CORA)-based osteotomy of the ulna in the treatment of Bado-type I Monteggia injuries considering that an anterior bowing ulna is one of the obstacles of radial head reduction (19). Especially in pronation, the apex of the anterior ulnar deformity approaches the radius and acts as a fulcrum pushing the radial head anteriorly then increasing the risk of redislocation. Those who recommend osteotomy at the CORA site postulate that this method can not only eliminate the fulcrum effect of ulna but also restore the normal width and tension of the interosseous membrane by posterior angulation reconstruction (20,21). Clinically, it is not uncommon that the CORA occurs at a distal diaphysis of the ulna (5), given the potential challenges of CORA identification and the risk of delayed healing, an ulnar osteotomy site located at the proximal metaphysis is more advocated (22-24). To achieve lengthening and angulation of the ulna, Rajasekaran introduced the concept of sliding angulation osteotomy, which involves a sagittal oriented Z-shaped osteotomy of the ulna. A critical aspect of this approach is that the osteotomy site should be situated at the proximal metaphysis of the ulna (25).
In this study, we observed distinct distribution patterns of PUO range, with a notably higher number of patients undergoing osteotomy at proximal 1/5 to 1/3 of the ulna in the reduced group. As we all know, the overall stability of the forearm depends on the integrity of radioulnar articulations, encompassing the proximal radioulnar joint (PRUJ) and the distal radioulnar joint (DRUJ). These constructs are connected by the tough inelastic fibrous interosseous membrane (IOM) complex (26). IOM consists of five distinct components: the central band (CB); the accessory band (AB); the distal oblique bundle (DOB); the proximal oblique cord (POC), and the dorsal oblique cord (27). As the most functionally important component, CB has an average of 21° proximal-radial to distal-ulnar orientation to the longitudinal axis of the ulna (28). The ligamentous attachments of the CB are located at 53–64% of the radial length as measured from the distal radius, and the ulnar attachment at 29–44% of the ulnar length, as measured from the distal ulna. The ligamentous attachments of the proximal AB lie at 1/5 of the proximal radius and 1/3 of the proximal ulna (Figure 3A). Even though the AB contains less fibrous tissue than the CB, it is consistently present in all specimens studied by Skahen et al. Its oblique orientation parallels that of the CB and serves a similar function. The POC originates from the anterolateral aspect of the coronoid process, nearly 1/5 of the proximal ulna and inserts just oblique distal to the radial bicipital tuberosity (28). The tilted orientation of these fibers indicates the stabilizing effect of two directions: the vertical carrier resist the longitudinal dissociation force, and the horizontal carrier limits the horizontal radioulnar splaying during the axial load (29). The biomechanical role of the IOM offers new perspectives for treating CMF, particularly concerning the position of ulnar osteotomy.
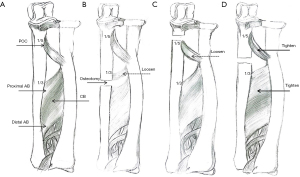
In theory, if the ulna osteotomy site is positioned distally to the 1/3 of the proximal ulna (the attachment point of AB), the force propelling the radius distally will weaken during ulnar distraction, because the tension of the proximal osteotomy interosseous membrane will decrease and the traction effect transmitted to the radius via the fibrous structures will reduce (Figure 3B). This effect will become more pronounced the closer the osteotomy is to the distal site. Consistent with this theory, our findings also revealed that one out of the three patients experiencing redislocation had undergone ulnar osteotomy at 34.26% of the proximal ulna. In the in-position group, no case had an osteotomy position exceeding the 1/3 mark of proximal ulna.
One of the redislocated patients (1/3) had an osteotomy at 17.08%, which is less than 1/5 of proximal ulna and proximal to POC attachment point following autologous bone transplantation and lengthening, the attachment point of the POC at the ulnar side shifted towards the distal end. Consequently, the tension of the POC inevitably reduced, potentially exerting a negative impact on the PRUJ stability (Figure 3C). Among the patients in the reduced group, with the exception of one case who underwent an osteotomy at 19.62% of proximal ulna, all the remaining patients had ulnar osteotomies positioned within the proximal 1/3 to 1/5 range.
To evaluate the predictive value of redislocation, various models of ROC curves were employed. It is well known that the extent of required lengthening and angulation is determined by the success of radial head reduction. Precise adjustment of lengthening and angulation directly impacts the stability of the radiocapitellar joint. In this study, we also observed that apart from PUO, only Osteotomy angle and post-PUL (a more indicative measure of ulnar lengthening) demonstrated a difference with P<0.15. Comparing the combination of Osteotomy angle and post-PUL with the addition of PUO range, we found an enhancement in accuracy and specificity, accompanied by an incremental improvement in discriminatory power. This outcome underscores the importance of considering all three factors: osteotomy angle, post-PUL, and PUO range, in prediction. This holistic approach will aid in developing standardized procedures and specifications for CMF surgery in the future. In a word, from the perspective of anatomy and biomechanics, the proximal 1/3 and 1/5 of the ulna appears to be a safe region for osteotomy. Within this range, both AB and POC experience maximum tension and can effectively exert the best function of stability in cases of CMF (Figure 3D). To this end, our results showed the significance of the osteotomy position of the ulna and once again emphasized the pivotal role of the IOM in maintaining the radial head in position.
Osteotomy performed at the proximal 1/3 to 1/5 of the ulna offers another significant advantage. The proportion of cancellous bone is much higher in this region which is more osteogenic than cortical bone (30). Thus, bone healing after osteotomy will be more favorable and nonunion will be less likely to happen, when osteotomy is performed at this region. Although the proximal 1/5 of the ulna is also cancellous bone, the challenges of achieving proper angulation and steel plate fixation are often encountered due to spatial limitations.
Previous management of the CMF is focused on the restoration of the anatomy of ulnar length and alignment, with limited attention given to the potential impact of the position of ulnar osteotomy on the longitudinal and transverse stability of the forearm. To our knowledge, this is the first study quantitatively analyzing the association between ulnar osteotomy position and redislocation in CMF.
Limitation
This study is subjected to several limitations due to its retrospective nature and relatively small sample size. A more extensive prospective randomized controlled study involving a larger patient cohort is warranted for further validation. Second, an extended follow-up period is essential to verify the potential occurrence of delayed redislocation and to evaluate the long-term quality of life and patient-centered outcomes. Finally, it is important to acknowledge that this study focus on a specific surgical approach at a single center, which may limit the generalizability of the results to other techniques or units.
Conclusions
Identifying the risk factors for radial head subluxation/dislocation holds significant importance as it offers surgeons a chance to intervene preemptively. Drawing from the findings of this study, we advocate for ulnar osteotomy to be performed within the proximal 1/5 to 1/3 of the ulna, as it is likely to yield a safer and more stable radiocapitellar joint.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-477/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-477/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-477/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-477/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013). This study was approved by the Human Research Ethics Committee at Children’s Hospital of Fudan University (No. 2020528), and informed written consent was obtained from the guardians of all children participating in the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ring D, Jupiter JB, Waters PM. Monteggia fractures in children and adults. J Am Acad Orthop Surg 1998;6:215-24. [Crossref] [PubMed]
- Singh V, Dey S, Parikh SN. Missed Diagnosis and Acute Management of Radial Head Dislocation With Plastic Deformation of Ulna in Children. J Pediatr Orthop 2020;40:e293-9. [Crossref] [PubMed]
- Bae DS. Successful Strategies for Managing Monteggia Injuries. J Pediatr Orthop 2016;36:S67-70. [Crossref] [PubMed]
- Nakamura K, Hirachi K, Uchiyama S, et al. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg Am 2009;91:1394-404. [Crossref] [PubMed]
- Park H, Park KW, Park KB, et al. Impact of Open Reduction on Surgical Strategies for Missed Monteggia Fracture in Children. Yonsei Med J 2017;58:829-36. [Crossref] [PubMed]
- Miller TC, Fishman FG. Management of Monteggia Injuries in the Pediatric Patient. Hand Clin 2020;36:469-78. [Crossref] [PubMed]
- Kim HT, Park BG, Suh JT, et al. Chronic radial head dislocation in children, Part 2: results of open treatment and factors affecting final outcome. J Pediatr Orthop 2002;22:591-7. [Crossref] [PubMed]
- Peterson HA. Deformities and problems of the forearm in children with multiple hereditary osteochondromata. J Pediatr Orthop 1994;14:92-100. [Crossref] [PubMed]
- Yan G, Nan G. Modified osteotomy for treatment of forearm deformities (Masada IIb) in hereditary multiple osteochondromas: a retrospective review. BMC Musculoskelet Disord 2021;22:943. [Crossref] [PubMed]
- Xu P, Zhang Z, Ning B, et al. Outcomes and experience after open reduction for chronic Monteggia fracture in children. Transl Pediatr 2022;11:1122-9. [Crossref] [PubMed]
- Basile G, Fozzato S, Bianco Prevot L, et al. Monteggia fracture associated with ipsilateral intercondylar distal humeral fracture with posterior interosseous nerve palsy: case report, medico-legal implications, and methodological assessment analysis. Eur Rev Med Pharmacol Sci 2023;27:5614-9. [PubMed]
- Tan SHS, Low JY, Chen H, et al. Surgical Management of Missed Pediatric Monteggia Fractures: A Systematic Review and Meta-Analysis. J Orthop Trauma 2022;36:65-73. [Crossref] [PubMed]
- Stragier B, De Smet L, Degreef I. Long-term follow-up of corrective ulnar osteotomy for missed Monteggia fractures in children. J Shoulder Elbow Surg 2018;27:e337-43. [Crossref] [PubMed]
- Chin K, Kozin SH, Herman M, et al. Pediatric Monteggia Fracture-Dislocations: Avoiding Problems and Managing Complications. Instr Course Lect 2016;65:399-407. [PubMed]
- Garg P, Baid P, Sinha S, et al. Outcome of radial head preserving operations in missed Monteggia fracture in children. Indian J Orthop 2011;45:404-9. [Crossref] [PubMed]
- Shinohara D, Yasuda T, Arai M, et al. A Long-standing Monteggia Fracture in a Child who underwent Bone Lengthening and Annular Ligament Reconstruction: A Case Report. J Orthop Case Rep 2019;9:30-3. [PubMed]
- Liao S, Pan J, Lin H, et al. A new approach for surgical treatment of chronic Monteggia fracture in children. Injury 2019;50:1237-41. [Crossref] [PubMed]
- Rahbek O, Deutch SR, Kold S, et al. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J Child Orthop 2011;5:449-57. [Crossref] [PubMed]
- Xu Z, Li Y, Wang Z, et al. Open reduction combined with CORA-based osteotomy of the ulna in the treatment of missed Bado type I Monteggia injury: A retrospective study of 5 cases. Medicine (Baltimore) 2017;96:e8609. [Crossref] [PubMed]
- Wang MN, Chang WN. Chronic posttraumatic anterior dislocation of the radial head in children: thirteen cases treated by open reduction, ulnar osteotomy, and annular ligament reconstruction through a Boyd incision. J Orthop Trauma 2006;20:1-5. [Crossref] [PubMed]
- Best TN. Management of old unreduced Monteggia fracture dislocations of the elbow in children. J Pediatr Orthop 1994;14:193-9. [Crossref] [PubMed]
- Ray R, Gaston M. Treatment of late-presenting Monteggia variant with an isolated, simple flexion ulnar osteotomy. J Pediatr Orthop B 2014;23:472-6. [Crossref] [PubMed]
- Lu X, Kun Wang Y, Zhang J, et al. Management of missed Monteggia fractures with ulnar osteotomy, open reduction, and dual-socket external fixation. J Pediatr Orthop 2013;33:398-402. [Crossref] [PubMed]
- Lädermann A, Ceroni D, Lefèvre Y, et al. Surgical treatment of missed Monteggia lesions in children. J Child Orthop 2007;1:237-42. [Crossref] [PubMed]
- Belangero WD, Livani B, Zogaib RK. Treatment of chronic radial head dislocations in children. Int Orthop 2007;31:151-4. [Crossref] [PubMed]
- Masouros PT, Apergis EP, Mavrogenis AF, et al. Reconstruction of the forearm interosseous membrane: a biomechanical study of three different techniques. J Hand Surg Eur Vol 2020;45:360-8. [Crossref] [PubMed]
- Noda K, Goto A, Murase T, et al. Interosseous membrane of the forearm: an anatomical study of ligament attachment locations. J Hand Surg Am 2009;34:415-22. [Crossref] [PubMed]
- Skahen JR 3rd, Palmer AK, Werner FW, et al. The interosseous membrane of the forearm: anatomy and function. J Hand Surg Am 1997;22:981-5. [Crossref] [PubMed]
- Soubeyrand M, Wassermann V, Hirsch C, et al. The middle radioulnar joint and triarticular forearm complex. J Hand Surg Eur Vol 2011;36:447-54. [Crossref] [PubMed]
- Khan SN, Cammisa FP Jr, Sandhu HS, et al. The biology of bone grafting. J Am Acad Orthop Surg 2005;13:77-86. [Crossref] [PubMed]


