
Impact of the COVID-19 pandemic on the demographic and disease burden of pediatric malignant solid tumors in China: a single-center, cross-sectional study
Highlight box
Key findings
• The number of patients with malignant solid tumors from the northern region of China who attended Beijing Children’s Hospital increased during novel coronavirus disease 2019 (COVID-19) pandemic in China.
• Meanwhile, other demographic characteristics and disease burden did not change significantly.
What is known and what is new?
• The infection of COVID-19 not only directly threatened the lives of individuals but also affected public healthcare and the global economy.
• Our study indicated that the accessibility of equitable healthcare for pediatric patients diagnosed with malignant solid tumors in China during the COVID-19 pandemic did not appear to change.
What is the implication, and what should change now?
• Drawing on data from a high-tier institution, this study summarized the experiences, including the balanced development of regional medical institutions, internet hospital visits, outpatient chemotherapy, and the establishment of subcenters, to facilitate the provision of prompt and secure care to vulnerable child populations in future pandemics or other comparable national crises.
Introduction
In December 2019, there was a global outbreak of an unexplained pneumonia, later officially named the novel coronavirus disease 2019 (COVID-19) (1,2). This pandemic had an impact on healthcare systems and economies global, and on the day-to-day life of nearly every individual on the planet (3). Faced with enormous challenges, the Chinese government responded by adopting certain policies to mitigate the spread of the virus while preserving public health benefits as much as possible (3,4). Several studies around the world reported that there were concerns about the side effects of the pandemic on pediatric cancer care, such as prevention from early diagnosis, delayed chemotherapy, reduced access to surgery, radiotherapy, and supportive care (5,6). However, it is worth noting that there is a lack of research in this area in China.
Cancer is one of the leading causes of death and disease burden in children (7). In addition, the diagnostic and treatment process can create other sources of pressure for children and their families, such as physical pain, psychological distress, and financial burden (8). In terms of tumor types, neuroblastoma (NB) and central nervous system (CNS) tumors are the most common extracranial and intracranial solid tumors in children, accounting for 15–20% and 8–10% of childhood malignancies, respectively (9,10). A multicenter study by our team showed that rhabdomyosarcoma (RMS), Wilms tumor (WT), hepatoblastoma (HB), and Ewing sarcoma (ES) are also among the top 10 most common childhood-specific cancers (11). However, in the context of the COVID-19 pandemic, no cohort study in China on the demographics and disease burden of patients with these pediatric malignant solid tumors has been conducted.
The purpose of this study was to analyze the COVID-19-related changes in China concerning the demographics, clinical characteristics, and treatment costs for children with six common malignant solid tumors through data collected from the National Center for Children’s Health. With the summarization of experiences, this approach aims to facilitate the provision of prompt and secure care to vulnerable child populations in future pandemics or other comparable national crises. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-480/rc).
Methods
Study design and data sources
A cross-sectional study was conducted at Beijing Children’s Hospital (BCH) in Beijing, China. According to the statistics of the National Pediatric Cancer Surveillance Annual Report, among Chinese provinces, Beijing is the most common destination for patients with cancer seeking medical treatment outside of province, far exceeding the province in second position (12,13). All patients diagnosed with one of the six common solid tumors (i.e., NB, RMS, CNS tumor, WT, HB, ES) treated at the Medical Oncology Department of BCH between 2019 and 2021 were included in this study.
In accordance with the progression of the COVID-19 epidemic over the course of natural years, our attention was directed toward the outbreak year of 2019, as well as the preceding year of 2018 and the subsequent year of 2020 (1). This study retrospectively analyzed the changes in demographics and financial burden of children with solid tumors during the 2019–2021 pandemic period. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Beijing Children’s Hospital Institutional Ethics Committee (No. [2023]-E-031-R). Informed consent was acquired from all participants and their parents.
Diagnostic criteria and management of tumor
All the enrolled patients were diagnosed via biopsy or surgical pathology or bone marrow examination for tumor cells. Two or more tier 3, grade A hospitals conducted pathological consultation for diagnosis to obtain consistent pathological results. The patients were evaluated after every two courses of chemotherapy and were followed up every 3 months for the first year after the therapy had finished, every 6 months for the second year, and every 6 months for the subsequent third and fourth year. The stage of NB was determined according to International Neuroblastoma Risk Group Staging System (INRGSS) criteria (14). Patients with NB were treated according to the NB protocol of BCH (BCH-NB-2007), which was developed based on Hong Kong NB Protocol 7 and the European Low and Intermediate-Risk (IR) NB protocol (15). The staging criteria for RMS adopted the postoperative pathological clinical grouping system of the Intergroup RMS study (IRS) in the United States combined with the clinical staging system [Tumor Node Metastasis-Union for International Cancer Control (TNM-UICC)] developed by the International Society of Paediatric Oncology (SIOP) based on pretreatment imaging (16). WT and HB were staged according to the clinical staging criteria of the Children’s Oncology Group (COG) and the Pretreatment Extent of Tumor (PRETEXT) system, respectively (17,18). CNS tumors were analyzed using the fifth edition of the World Health Organization (WHO) classification of CNS tumors (WHO-CNS5) (19).
Variables and outcomes
Information on sociodemographics, general clinical characteristics at onset and patients circumstances for hospitalization was retrospectively collected. The sociodemographic variables mainly included gender, age, origin, and hospital for first surgery of children with various tumors in the past 3 years. Patient origin was grouped into seven geographic areas: northeastern China, northern China, northwestern China, central China, eastern China, southern China, and southwestern China. General clinical characteristics included stage, risk group, pathological classification, genes associated with prognosis, primary site of tumor, and initial chief complaints, among others. The economic burden was specifically evaluated according to hospitalization frequency, number of hospitalizations per person per year, per-visit inpatient expense, and insurance status of real-time settlement. The cost per hospitalization was calculated as the average cost of each hospitalization per person using the follow formula: annual total hospitalization cost per person divided/hospitalizations in that year (exchange rate: USD $1 to CNY ¥6.85).
Statistical analysis
The data in a normal distribution are presented as the mean ± standard deviation (SD), while those in a nonnormal distribution data are presented as the median and interquartile range. Categorical variables are described in absolute percentages. Pearson χ2 test and the Mann-Whitney test were used as appropriate to analyze the differences between variables in the 3 years of the COVID-19 pandemic period. For multiple comparisons, P values were corrected with the Bonferroni method. A P value <0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 22 (IBM Corp., Armonk, NY, USA) and GraphPad Prism version 8 (GraphPad Software, San Diego, CA, USA).
Results
Basic demographic information of the participants
A total of 876 patients initially diagnosed with tumor during the 2019–2021 period were enrolled in the study (Figure 1A), including 479 (54.7%) cases of NB, 144 (16.4%) cases of RMS, 41 (4.7%) cases of WT, 88 (10.0%) cases of HB, 43 (4.9%) cases of ES, and 81 (9.2%) cases of CNS tumors. Among them, 463 (52.9%) were males and 413 (47.1%) were females (Table 1). The median age was 39 [interquartile range (IQR), 22–69] months. Patients originated from regions from all over China, with the most common being northern China (43.9%) and eastern China (25.8%), followed by northeastern China (9.7%), central China (9.1%), northwestern China (7.5%), southwestern China (2.7%), and southern China (1.1%). Tumor resection was performed in 796 children, 741 of whom had accurate data on the hospital of first surgery. Except for two children who underwent tumor resection at Mount Elizabeth Hospital, Singapore, all the children were operated on in China. Of these operations, 734 (99.1%) were performed in public tertiary-grade A hospitals, 2 (0.3%) in public secondary-grade A hospitals, and 3 (0.4%) in private hospitals. The ratio of first surgeries conducted in specialized hospitals to those performed in general hospitals was 656:85.
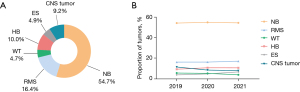
Table 1
| Characteristic | N | 2019 | 2020 | 2021 | χ2 | P value |
|---|---|---|---|---|---|---|
| Percent of sample, n (%) | 876 | 336 (38.4) | 216 (24.6) | 324 (37.0) | ||
| Sex, n (%) | 1.5211 | 0.4681 | ||||
| Male | 463 (52.9) | 178 (53.0) | 107 (49.5) | 178 (54.9) | ||
| Female | 413 (47.1) | 158 (47.0) | 109 (50.5) | 146 (45.1) | ||
| Age (years), n (%) | 5.2461 | 0.5321 | ||||
| <1.5 | 183 (20.9) | 72 (21.4) | 42 (19.4) | 69 (21.3) | ||
| 1.5–4 | 437 (49.9) | 159 (47.3) | 107 (49.5) | 171 (52.8) | ||
| 5–9 | 191 (21.8) | 83 (24.7) | 48 (22.2) | 60 (18.5) | ||
| ≥10 | 65 (7.4) | 22 (6.5) | 19 (8.8) | 24 (7.4) | ||
| Area, n (%) | 31.8861, 13.2892, 7.5663, 23.1944 | 0.0011**, 0.1172, 0.2363, 0.0034** | ||||
| Northeastern China | 85 (9.7) | 23 (6.8) | 18 (8.3) | 44 (13.6) | ||
| Northern China | 385 (43.9) | 133 (39.6) | 106 (49.1) | 146 (45.1) | ||
| Northwestern China | 66 (7.5) | 23 (6.8) | 22 (10.2) | 21 (6.5) | ||
| Central China | 80 (9.1) | 42 (12.5) | 17 (7.9) | 21 (6.5) | ||
| Eastern China | 226 (25.8) | 95 (28.3) | 46 (21.3) | 85 (26.2) | ||
| Southern China | 10 (1.1) | 8 (2.4) | 1 (0.5) | 1 (0.3) | ||
| Southwestern China | 24 (2.7) | 12 (3.6) | 6 (2.8) | 6 (1.9) | ||
| First surgical hospital5, n (%) | 3.7781 | 0.1581 | ||||
| Specialized hospital | 656 (88.5) | 253 (85.8) | 160 (90.4) | 243 (90.3) | ||
| General hospital | 85 (11.5) | 42 (14.2) | 17 (9.6) | 26 (9.7) |
Data were assessed with the chi-squared test. For multiple comparisons, P values were corrected with the Bonferroni method. **, P<0.01; 1, 2019 vs. 2020 vs. 2021; 2, 2019 vs. 2020; 3, 2021 vs. 2020; 4, 2019 vs. 2021; 5, there were 135 unknown cases that were not included in the statistics. COVID-19, coronavirus disease 2019.
Comparison of patient demographics during COVID-19 according to type of pediatric tumor
In general, the number of children with tumors who visited BCH in 2020 (24.6%) after the outbreak decreased significantly compared with that in 2019 (38.3%) before the epidemic and gradually increased in 2021 (37.1%). None of the enrolled children were infected with COVID-19. The age, gender, region, and first surgical hospital of all enrolled patients over the 3 years are shown in Table 1. The regional origin of the patients showed significant variation after the outbreak (P=0.001). With the outbreak of COVID-19, the number of patients in northern China and northeastern China who came to our center increased, while the number of patients in the central China, southern China, and southwestern China decreased. However, there was no change in the gender of patients (P=0.468) and whether they were operated on in specialized hospitals (P=0.158) during the epidemic. The age of onset of children with tumors was most common in those 1.5–4 years old, followed by those younger than 1.5 years and those 5–10 years old, with no significant differences over the 3 years (P=0.532; Figure S1).
There was no significant change in the tumor category of patients during the COVID-19 pandemic. Over the 3 years, the most common tumor was NB, and the proportion of each tumor did not change significantly (χ2=6.99; P=0.726; Figure 1B). Compared to 2019, 2020 showed a notable decrease in the number of male patients diagnosed with HB in the year, and there was a subsequent return to this number observed in 2021 (P=0.033; Table S1). The regional origin in children with CNS tumors changed significantly over the 3 years (P=0.017). In addition, there were significant differences during the pandemic in terms of first surgery in specialist or general hospitals for children with RMS (P=0.007) or CNS tumors (P<0.001). The demographic characteristics of patients with other tumor types did not change significantly over the 3 years.
Changes in the clinical characteristics of patients with various tumors before and after the epidemic
In this study, 479 children with NB were enrolled, including 183 (38.2%) in 2019, 119 (24.8%) in 2020, and 177 (37.0%) in 2021. The median age at diagnosis was 38 (IQR, 20–56) months. Compared with 2019, 2020 showed a slight decrease in the proportion of children with NB at stage M and an increase in the number of children at stage L2, but these differences were not statistically significant (P=0.079; Table 2). In the comparison of pre- and post-pandemic variables in children with NB, there were no changes in risk group (P=0.099), MYCN status (P=0.391), or primary tumor site (P=0.174). A total of 144 patients with RMS were enrolled in our study, including 54 (37.5%) in 2019, 35 (24.3%) in 2020, and 55 (38.2%) in 2021. Their median age at first diagnosis was 57 (IQR, 26–102) months. Similarly to NB, children with RMS showed no differences over the 3 years in terms of TNM staging (P=0.219), risk group (P=0.292), pathological classification (P=0.169), FOXO1 status (P=0.946), or tumor primary site (P=0.396) (Table 3). The most common CNS tumors before and after the epidemic both were medulloblastoma (34.6%) and astrocytoma (27.2%). These tumors most commonly originated in the ventricles (32.1%), followed by the lobe of the brain (14.8%; Table S2). The characteristics of children with other tumors (CNS, WT, HB and ES) did not change significantly over the course of the COVID-19 pandemic (Tables S2,S3).
Table 2
| Characteristic | N | 2019 | 2020 | 2021 | χ2 | P value |
|---|---|---|---|---|---|---|
| Percent of sample, n (%) | 479 | 183 (38.2) | 119 (24.8) | 177 (37.0) | ||
| Staging, n (%) | 5.082 | 0.079 | ||||
| L1–L2/Ms | 277 (57.8) | 94 (51.4) | 74 (62.2) | 109 (61.6) | ||
| M | 202 (42.2) | 89 (48.6) | 45 (37.8) | 68 (38.4) | ||
| Risk group, n (%) | 7.816 | 0.099 | ||||
| LR | 145 (30.3) | 55 (30.1) | 32 (26.9) | 58 (32.8) | ||
| IR | 140 (29.2) | 44 (24.0) | 45 (37.8) | 51 (28.8) | ||
| HR | 194 (40.5) | 84 (45.9) | 42 (35.3) | 68 (38.4) | ||
| MYCN status1, n (%) | 1.878 | 0.391 | ||||
| Amplification | 68 (14.4) | 31 (17.0) | 16 (13.8) | 21 (12.0) | ||
| Not amplification | 405 (85.6) | 151 (83.0) | 100 (86.2) | 154 (88.0) | ||
| Primary tumor site, n (%) | 11.517 | 0.174 | ||||
| Retroperitoneum and adrenal glands | 302 (63.0) | 125 (68.3) | 76 (63.9) | 101 (57.1) | ||
| Mediastinum | 152 (31.7) | 49 (26.8) | 38 (31.9) | 65 (36.7) | ||
| Neck | 15 (3.1) | 8 (4.4) | 3 (2.5) | 4 (2.3) | ||
| Pelvic cavity | 4 (0.8) | 0 | 1 (0.8) | 3 (1.7) | ||
| Other sites | 6 (1.3) | 1 (0.5) | 1 (0.8) | 4 (2.3) |
Data were assessed with chi-squared test. 1, there were 6 unknown cases that were not included in the statistics. COVID-19, coronavirus disease 2019; LR, low-risk; IR, intermediate-risk; HR, high-risk; MYCN, amplification of the MYCN gene.
Table 3
| Characteristic | N | 2019 | 2020 | 2021 | χ2 | P value |
|---|---|---|---|---|---|---|
| Percent of sample, n (%) | 144 | 54 (37.5) | 35 (24.3) | 55 (38.2) | ||
| TNM staging1, n (%) | 8.265 | 0.219 | ||||
| 1 | 29 (21.5) | 13 (24.1) | 6 (17.1) | 10 (21.7) | ||
| 2 | 11 (8.1) | 3 (5.6) | 1 (2.9) | 7 (15.2) | ||
| 3 | 63 (46.7) | 26 (48.1) | 21 (60.0) | 16 (34.8) | ||
| 4 | 32 (23.7) | 12 (22.2) | 7 (20.0) | 13 (28.3) | ||
| Risk group1, n (%) | 7.321 | 0.292 | ||||
| LR | 12 (8.7) | 6 (11.1) | 2 (5.7) | 4 (8.2) | ||
| IR | 70 (50.7) | 27 (50.0) | 21 (60.0) | 22 (44.9) | ||
| HR | 25 (18.1) | 8 (14.8) | 3 (8.6) | 14 (28.6) | ||
| CNS invasion | 31 (22.5) | 13 (24.1) | 9 (25.7) | 9 (18.4) | ||
| Pathological classification1, n (%) | 6.430 | 0.169 | ||||
| Embryonal | 83 (58.5) | 30 (55.6) | 18 (51.4) | 35 (66.0) | ||
| Alveolar | 57 (40.1) | 24 (44.4) | 17 (48.6) | 16 (30.2) | ||
| Pleomorphic/anaplastic | 2 (1.4) | 0 | 0 | 2 (3.8) | ||
| FOXO1 status1, n (%) | 0.112 | 0.946 | ||||
| + | 46 (62.9) | 19 (62.0) | 13 (61.8) | 14 (65.0) | ||
| − | 78 (37.1) | 31 (38.0) | 21 (38.2) | 26 (35.0) | ||
| Primary tumor site, n (%) | 8.392 | 0.396 | ||||
| Head and neck | 65 (45.1) | 28 (51.9) | 17 (48.6) | 20 (36.4) | ||
| Urogenital system | 18 (12.5) | 3 (5.6) | 5 (14.3) | 10 (18.2) | ||
| Abdominal and pelvic cavities | 27 (18.8) | 12 (22.2) | 4 (11.4) | 11 (20.0) | ||
| Limbs | 15 (10.4) | 5 (9.3) | 5 (14.3) | 5 (9.1) | ||
| Other sites | 19 (13.2) | 6 (11.1) | 4 (11.4) | 9 (16.4) |
Data were assessed with the chi-squared test. 1, there were 9, 6, 2, 20 unknown cases in TNM staging, risk group, pathological classification, FOXO1 status respectively, which were not included in the statistics. COVID-19, coronavirus disease 2019; TNM, Tumor Node Metastasis; LR, low-risk; IR, intermediate-risk; HR, high-risk; CNS, central nervous system.
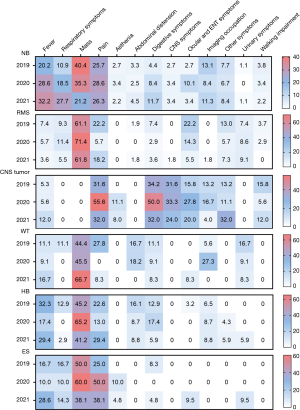
The chief complaints at initial hospital admission are summarize in Figure 2. Presence of a mass, fever, respiratory symptoms, and pain were the main onset symptoms in children with NB. Of these, mass presence was the most common in the 2019–2020 period, and fever was the most common in 2021. Meanwhile, mass presence and pain were always the most common symptom of children with the other five tumor types (i.e., RMS, CNS tumors, WT, HB, and ES) over the 3 years. Compared to that in 2019, the proportion of fever and respiratory symptoms in children with NB increased in 2020, while that in children with the other tumor types remained unchanged or even decreased.
Medical expenses and costs for patients with solid tumors in the 2019–2021 period
To further assess the impact of the epidemic on the economic burden related to pediatric tumors in China, the hospitalization of all children with the aforementioned six tumor types during the 3-year period (before, during, and after the outbreak) were analyzed. From 2019 to 2021, a total of 3,380, 2,836, and 3,094 hospitalization records were queried, respectively; that is, the annual hospitalization frequency was determined. The median number of hospitalizations per person per year over the 3 years was 5 (IQR, 3–8), which did not represent a significant difference (χ2=0.888; P=0.641; Figure 3A). Similarly, the average single hospitalization cost per person during the COVID-19 period did not change significantly over this period, with costs being USD $1,273.8 (IQR, 862.7–2,169.4), USD $1,283.8 (IQR, 866.8–1,789.1), and USD $1,293.0 (IQR, 924.8–1,944.7) for the years from 2019 to 2021, respectively (χ2=2.038; P=0.361; Figure 3B). In response to the pandemic, China implemented a range of medical insurance policies aiming at providing financial assistance to families affected by cancer, thereby alleviating the burden of treatment costs. The medical insurance coverage of real-time settlement is shown in Figure 3C. Our analysis indicated that the out-of-pocket ratio dropped from 42.7% in 2019 to 19.0% in 2021, while the health insurance coverage ratio rose from 57.3% to 81.0% in this same period (χ2=149.47; P<0.0001).

Discussion
To our knowledge, this is one of few studies to summarize the data on the demographics and economic burden of children with malignant solid tumors in China during the COVID-19 pandemic. We conducted this study at the National Center for Children’s Health, one of the most authoritative centers for treating childhood cancer in China.
The COVID-19 pandemic has posed an unprecedented global threat to the safe, effective, and timely care of children with cancer (20-22). Along with the physical, psychological, and financial impact of the pandemic, pediatric oncologists around the world face numerous challenges, including staffing shortages and occupational safety issues (23). After the outbreak, China introduced a series of policies to control the source of infection in order to ensure the safety of its people. As a consequence, hospitals across the country had to strictly check the nucleic acid status of hospitalized children with tumors for the COVID-19 virus. Therefore, we aimed to determine whether the demographics, clinical characteristics, and disease burden of children with solid tumors had been affected by the policies of pandemic control with China during the 2019–2021 period.
Statistics from our study indicated that the total number of children with solid tumors treated in our center in the outbreak year [2020] decreased compared with that of 2019, and soon returned to normal in 2021. This constituted a change in the number of patients treated at a single center visits rather than a shift in the national incidence. Significant differences were found mainly in the regional origin of patients, with patients visiting BCH after the epidemic mainly being from northern China. Facing the possible impact of the pandemic, the Chinese government and hospitals responded quickly after the outbreak, increasing internet hospital visits, outpatient chemotherapy, and the establishment of subcenters to ensure that children with tumors received timely diagnosis and treatment. It is worth noting that, notwithstanding the alterations in the manner in which children were treated for, BCH continued to uphold the diagnostic and therapeutic protocol established prior to the outbreak. The above-mentioned changes might be related not only to the migration between cities during the pandemic in China but also to the development of other regional medical centers in the country. Based on data obtained from the National Cancer for Pediatric Cancer Surveillance, the mean percentage of those selecting Beijing as a medical treatment destination outside of one’s province declined from 59.2% during the 2017–2018 period to 44.2% in the 2019–2020 period, while the percentage for the selection of other provinces increased (11,12). Meanwhile, there was no change in gender, age, tumor type, staging, risk grouping, pathological type, primary site, or prognosis-related genes of patients with the six included tumors in the study. Additionally, the first symptoms of children remained the presence of a mass and pain, which were the most typical tumor symptoms before the epidemic. These findings initially indicate that in China, COVID-19 had no significant impact on the timely treatment of children with tumors in large specialized centers. Accelerating the regional balance of medical institutions may thus be one means for developing countries to cope with COVID-19 pandemic or similar crises.
Some studies have examined whether the COVID-19 pandemic increased the psychosocial and economic stress in families affected by cancer (24,25). Families of children with cancer are often already at high risk of increased material and financial difficulties (26,27). Our study examined the effect of COVID-19 on the financial strain experienced by children with tumors by using the yearly hospitalization costs per person as a metric for analysis. The results suggested that the number of hospitalizations per person per year and the average cost per person per hospitalization did not change significantly over the 3-year pandemic period and that treatments were administered regularly. This demonstrated that within the context of pandemic, the timely establishment of subtreatment centers, along with standardized diagnosis and treatment management by oncologists, was conducive to balancing the financial burden.
Chinese citizens have the opportunity to consistently reduce their medical expenses through real-time settlement at discharge and reimbursement after discharge depending on the type of insurance they hold. In this study, the coverage of medical insurance visits with real-time settlement was found to have increased significantly year-over-year from 2019 to 2021, suggesting that Medicare is becoming increasingly convenient and can aid in reducing the burden of disease in China.
The COVID-19 pandemic has been one of the greatest global challenges faced by children with cancer in search of equitable treatment over the past decades, and oncology teams must adapt to this challenging new era. Soon after the COVID-19 outbreak, the SIOP, COG, the St. Jude Global Alliance, and Childhood Cancer International came together to provide practical advice for adjusting the care of children with cancer during the pandemic (28). Within this context, medical team were required to adjust the oncology treatment plan and prioritize the patients based on their response and prognosis (25). Moreover, the use of telehealth to optimize clinical care has become a powerful tool in response to COVID-19 (29). These events prove that global healthcare for childhood oncology has a certain degree of resilience in the face of pressures from major crises, such as epidemics (30).
Our study provides a preliminary review of the diagnosis and treatment of pediatric tumors in China under the challenge of the pandemic to a certain extent. However, as a single-center study, our research might have produced results different from those of a national multicenter study. The indirect effects of vulnerable groups of children with cancer during the COVID-19 pandemic, such as quality of life, increased transportation, absenteeism expenses, and decreased availability of family members, were not addressed in the present study (31,32). Furthermore, the long-term outcomes of the children with solid tumors still require additional investigation (33,34).
Conclusions
The opportunity for timely and fair care for children with tumors did not appear to change within the context of COVID-19 control in China. Oncology healthcare systems have the capacity to respond to large-scale crises through certain measures developed in China, such as the balanced development of regional medical institutions, internet hospital visits, outpatient chemotherapy, and the establishment of subcenters.
Acknowledgments
We would like to thank the participating patients and their families.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-480/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-480/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-480/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-480/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507-13. [Crossref] [PubMed]
- The Health Foundation. COVID-19: five dimensions of impact, 2020. Available online: https://www.health.org.uk/news-and-comment/blogs/covid-19-five-dimensions-of-impact
- Qi J, Zhang D, Zhang X, et al. Short- and medium-term impacts of strict anti-contagion policies on non-COVID-19 mortality in China. Nat Hum Behav 2022;6:55-63. [Crossref] [PubMed]
- Graetz D, Agulnik A, Ranadive R, et al. Global effect of the COVID-19 pandemic on paediatric cancer care: a cross-sectional study. Lancet Child Adolesc Health 2021;5:332-40. [Crossref] [PubMed]
- Katato GK, Sitaula P, Gupte A, et al. The Impact of COVID-19 on Pediatric Malignancy Diagnosis and Treatment: Never the Same but Lessons Learned. Vaccines (Basel) 2023;11:667. [Crossref] [PubMed]
- Nikte V, Patil S, Chaudhari H, et al. Financial toxicity and its implication on quality of life in patients attending the palliative care department in a regional cancer centre: An observational study. J Cancer Policy 2024;39:100460. [Crossref] [PubMed]
- Schepers SA, Sint Nicolaas SM, Maurice-Stam H, et al. Parental distress 6 months after a pediatric cancer diagnosis in relation to family psychosocial risk at diagnosis. Cancer 2018;124:381-90. [Crossref] [PubMed]
- Udaka YT, Packer RJ. Pediatric Brain Tumors. Neurol Clin 2018;36:533-56. [Crossref] [PubMed]
- Su Y, Qin H, Chen C, et al. Treatment and outcomes of 1041 pediatric patients with neuroblastoma who received multidisciplinary care in China. Pediatr Investig 2020;4:157-67. [Crossref] [PubMed]
- Ni X, Li Z, Li X, et al. Socioeconomic inequalities in cancer incidence and access to health services among children and adolescents in China: a cross-sectional study. Lancet 2022;400:1020-32. [Crossref] [PubMed]
- Ni X, Li Z, Xu X, et al. National Pediatric Cancer Surveillance Annual Report 2020. Beijing: People’s Medical Publishing House; 2021:90.
- Ni X, Li Z, Xu X, et al. National Pediatric Cancer Surveillance Annual Report 2022. Beijing: People’s Medical Publishing House; 2022:44.
- Monclair T, Brodeur GM, Ambros PF, et al. The International Neuroblastoma Risk Group (INRG) staging system: an INRG Task Force report. J Clin Oncol 2009;27:298-303. [Crossref] [PubMed]
- Ma X, Duan C, Cai S, et al. The development and initial evaluation of referral flowchart for suspected neuroblastoma for pediatricians in nononcology clinics in China. Pediatr Blood Cancer 2021;68:e28869. [Crossref] [PubMed]
- Rudzinski ER, Anderson JR, Hawkins DS, et al. The World Health Organization Classification of Skeletal Muscle Tumors in Pediatric Rhabdomyosarcoma: A Report From the Children's Oncology Group. Arch Pathol Lab Med 2015;139:1281-7. [Crossref] [PubMed]
- Lopes RI, Lorenzo A. Recent advances in the management of Wilms' tumor. F1000Res 2017;6:670. [Crossref] [PubMed]
- Towbin AJ, Meyers RL, Woodley H, et al. 2017 PRETEXT: radiologic staging system for primary hepatic malignancies of childhood revised for the Paediatric Hepatic International Tumour Trial (PHITT). Pediatr Radiol 2018;48:536-54. [Crossref] [PubMed]
- Louis DN, Perry A, Wesseling P, et al. The 2021 WHO Classification of Tumors of the Central Nervous System: a summary. Neuro Oncol 2021;23:1231-51. [Crossref] [PubMed]
- Ding YY, Ramakrishna S, Long AH, et al. Delayed cancer diagnoses and high mortality in children during the COVID-19 pandemic. Pediatr Blood Cancer 2020;67:e28427. [Crossref] [PubMed]
- Chiaravalli S, Ferrari A, Sironi G, et al. A collateral effect of the COVID-19 pandemic: Delayed diagnosis in pediatric solid tumors. Pediatr Blood Cancer 2020;67:e28640. [Crossref] [PubMed]
- Wiphatphumiprates PP, Graetz DE, Ferrara G, et al. The COVID-19 Pandemic's impact on sustainability and expansion of a Pediatric Early Warning System in resource-limited hospitals. Cancer Med 2023;12:11878-88. [Crossref] [PubMed]
- Jazieh AR, Coutinho AK, Bensalem AA, et al. Impact of the COVID-19 Pandemic on Oncologists: Results of an International Study. JCO Glob Oncol 2021;7:242-52. [Crossref] [PubMed]
- Kahn AR, Schwalm CM, Wolfson JA, et al. COVID-19 in Children with Cancer. Curr Oncol Rep 2022;24:295-302. [Crossref] [PubMed]
- Gilbert R, Bates CR, Khetawat D, et al. Risk and Resilient Functioning of Families of Children with Cancer during the COVID-19 Pandemic. Int J Environ Res Public Health 2023;20:5208. [Crossref] [PubMed]
- Bona K, London WB, Guo D, et al. Trajectory of Material Hardship and Income Poverty in Families of Children Undergoing Chemotherapy: A Prospective Cohort Study. Pediatr Blood Cancer 2016;63:105-11. [Crossref] [PubMed]
- Huang HY, Shi JF, Guo LW, et al. Expenditure and Financial Burden for Common Cancers in China: a Hospital-based Multicentre Cross-sectional Study. Lancet 2016;388:S10.
- Sullivan M, Bouffet E, Rodriguez-Galindo C, et al. The COVID-19 pandemic: A rapid global response for children with cancer from SIOP, COG, SIOP-E, SIOP-PODC, IPSO, PROS, CCI, and St Jude Global. Pediatr Blood Cancer 2020;67:e28409. [Crossref] [PubMed]
- Kotecha RS. Challenges posed by COVID-19 to children with cancer. Lancet Oncol 2020;21:e235. [Crossref] [PubMed]
- Graetz DE, Sniderman E, Villegas CA, et al. Resilient health care in global pediatric oncology during the COVID-19 pandemic. Cancer 2022;128:797-807. [Crossref] [PubMed]
- Carai A, Locatelli F, Mastronuzzi A. Delayed referral of pediatric brain tumors during COVID-19 pandemic. Neuro Oncol 2020;22:1884-6. [Crossref] [PubMed]
- Wimberly CE, Towry L, Caudill C, et al. Impacts of COVID-19 on caregivers of childhood cancer survivors. Pediatr Blood Cancer 2021;68:e28943. [Crossref] [PubMed]
- Vasquez L, Sampor C, Villanueva G, et al. Early impact of the COVID-19 pandemic on paediatric cancer care in Latin America. Lancet Oncol 2020;21:753-5. [Crossref] [PubMed]
- Dominguez-Rojas JÁ, Vásquez-Hoyos P, Pérez-Morales R, et al. Association of Cancer Diagnosis and Therapeutic Stage With Mortality in Pediatric Patients With COVID-19, Prospective Multicenter Cohort Study From Latin America. Front Pediatr 2022;10:885633. [Crossref] [PubMed]
(English Language Editor: J. Gray)


