
A case report of proboscis lateralis: emphasis on the reconstruction of the lacrimal drainage system
Highlight box
Key findings
• A case report which emphasizes the treatment of proboscis lateralis (PL) should pay attention to the reconstruction of nasolacrimal duct and the reconstruction of nose shape.
What is known and what is new?
• PL is a rare congenital malformation of the craniofacial structure.
• The management of patients with PL should be done while keeping in mind the associated ocular anomalies.
What is the implication, and what should change now?
• Optimal care of PL patients involves a more comprehensive and multidisciplinary approach.
Introduction
Proboscis lateralis (PL) is a rare congenital malformation of the craniofacial structure characterized by a rudimentary nose-like structure with the incidence being less than 1:100,000 to 1:1,000,000 live births (1,2). Commonly associated anomalies of the eyes, palate, and lip were used by Boo-Chai in 1985 as the criteria for the first classification system based on a compilation of 34 reported cases, and were classified into four distinct categories (3). The most common systemic abnormalities associated with PL are sinonasal deformity with 87.9%, and concomitant ocular anomalies reported at 44–70% (1). Management of patients with PL should follow an individualized approach because of the wide variability in facial anomalies and ocular abnormalities (4). It should also consider the associated ocular anomalies and emphasize lacrimal drainage reconstruction. Therefore, optimal patient care involves a multidisciplinary approach (5). Herein, we report a rare case of PL in a 20-month-old female patient. We present this case in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-501/rc).
Case presentation
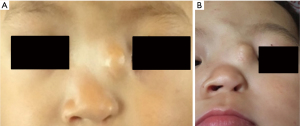
A 20-month-old girl was referred to our institution with a mass in the left medial canthal area, and ipsilateral symptomatic epiphora. On physical examination, the mass was found to be a cystic solid with no tenderness with a C-type old surgical scar on the surface. Facial dysmorphisms included mild hypertelorism and a depressed nasal bridge. The ipsilateral left nostril was patent but diminutive in size, lacking alar width (Figure 1). Nasal endoscopy revealed a narrow left internal nasal passage, but the nasal structure was not visible. A craniofacial computed tomography (CT) scan and magnetic resonance imaging (MRI) revealed that the left maxillary and ethmoid sinuses were not developed, and the left nasolacrimal duct had an expanded proximal region and a distal atresia. However, there was a bony passage extending into the left ethmoid sinus region, a cystic mass situated at the ipsilateral medial canthus of the affected eye, and the right lacrimal system and sinus were normal (Figures 2,3). Lacrimal irrigation was patent on the right side, whereas total regurgitation was observed on the left side of the fistula. Ultrasound showed an inhomogeneous hypoechoic liquid in the mass.


The patient was born with a congenital nasal appendage (a soft trunk-like process, approximately 3 cm long and 1 cm in diameter) originating from the left medial canthal region (Figure 4) with a patent tract transverse to the entire proboscis exuding discharge. No symptoms of left epiphora were observed. This child has no family history of PL and no other congenital conditions. Her mother also had no history of exposure to toxins or ionizing radiation during pregnancy.

At 4 months of age, the patient presented to another hospital with a diagnosis of PL based on the characteristic appearance of the anomaly. She underwent surgical removal of the appendage along the root and suturing of the incision by an otolaryngologist; however, the operative records did not describe probing of the lacrimal duct. The suture was removed 7 days postoperatively, and swelling of the left medial canthal region and left epiphora was noted. The local swelling gradually increased and intermittent purulent discharge was observed for 16 months (Figure 5).

We concluded that the secondary sequelae resulted from the removal of the appendage in the first surgery while neglecting the reconstruction of the nasolacrimal duct. The second surgery to release the pressure on the lacrimal sac and reconstruct the lacrimal system involved a multidisciplinary approach that included an otolaryngologist, ophthalmologist, and plastic surgeon. External dacryocystorhinostomy (DCR) through the original external incision aided in nasal endoscopic examination. This was the best option owing to the narrow internal nasal passage and provided a direct view of the swelling of the anomalous lacrimal sac (Figure 6). The otolaryngologist reconstructed the bony passage between the nasal cavity and the lacrimal sac, and nasal endoscopy revealed a wide opening in the nasal cavity of at least 6 mm. The ophthalmologist was responsible for probing the lacrimal duct and ensuring patency of the lacrimal drainage system. At the end of surgery, subcuticular closure and medical glue were used to close the incision, with no need to remove any sutures postoperatively. The patient was stable and discharged the next day after surgery, and followed up regularly for up to 2 years. Her nasal airway was patent without swelling of the medial canthal area recurrence and epiphora symptoms (Figure 7). At present, the child has no plans to undergo the next stage of repair surgery, and future surgery arrangements may be based on the patient’s own wishes. We will follow up closely with this child. Considering the limitations of deformity correction due to age, we will recommend the timing of the next operation during the follow-up.


This case was approved by the Ethics Committee of Beijing Children’s Hospital, Capital Medical University (No. 2022-E-067-R). All procedures performed in this study were in accordance with the ethical standards of the Ethics Committee of Beijing Children’s Hospital and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In nasal malformations, PL is a rare congenital anomaly thought to be a variety of median clefts (6). Maldevelopment (or duplication) of the nasal placode can cause PL with variable expression of heminasal aplasia embryologically (7). In 1985, Khoo divided the PL into four groups: Group 1, the least common, is PL with a normal nose. Group 2 is the PL with an ipsilaterally deformed nose. Group 3 is PL with ipsilateral deformed nose with additional ocular adnexal deformities, and is the most common, involving 47 % of PL cases. Group 4 consists of deformities in Group 3 with the addition of a cleft lip or palate (3,8).
A distinguishable tubular appendage-may also be associated with abnormalities of the ipsilateral eye, orbit, or lacrimal duct system (9). About 44–70% of reported PL cases have been associated with various ocular adnexal deformities. The spectrum of ocular abnormalities includes eyelid coloboma (32.6%), hypertelorism (25.3%), iris coloboma (22.4%), lacrimal system abnormality (20.7%), malpositioned eyebrows (14.4%), and retinochoroidal coloboma (12.9%) (1). This suggests the need for adequate ophthalmic evaluations while screening for congenital deformities in patients with PL. CT scans play a crucial role in the diagnosis of congenital nasolacrimal canal dysplasia because it can exactly delineate the shape, direction, and abnormal structure of the bony nasolacrimal duct (10). Subsidiary MRI and ultrasound exams provided information for planning appropriate management about the mass and assessed the exact location and dimensions of the lacrimal drainage system.
Based on Khoo’s classification, we categorized our patient into Group 3 with PL, ipsilateral deformity of the nose, and lacrimal duct system deformity. The reported discharge from the proboscis before the first operation and the ipsilateral epiphora noted only after the operation, combined with the CT findings indicating atresia at the distal end of the bony nasolacrimal duct led us to speculate that the proboscis may be a natural drainage passage of the lacrimal duct.
Timing and treatment protocols for surgery are not agreed upon, and some earlier studies suggested delaying it until the nasal skeleton is fully developed, which could be at preschool age or even later (11,12). Most surgeons currently believe that surgical repair can be accomplished within the first year, with a different surgical strategy (5,13-15). According to the authors, it is important to start reconstruction early, taking into account the psychological well-being of both the patient and their family. A simple excision of the proboscis was recommended in the initial reports about PL treatment (16). However, due to the high degree of variability of associated anomalies, it may lead to complications; these include the recurrent sinusitis, infection of the lacrimal system, drainage issues with mucus, and lacrimal drainage problems (14). Recent studies have advocated that management of PL must be individualized and have a more comprehensive and multidisciplinary approach (1,13). The takeaway from our patient was that simply surgically excising the proboscis directly resulted in the atretic nasolacrimal duct. The subsequent accumulation of secretion in the dilation of the lacrimal sac led to the mass in the medial canthal region.
The standard treatment for nasolacrimal duct obstruction includes external or endoscopic DCR. A skin incision near the lacrimal sac is required for the external approach, while a nasal endoscope is used for the endoscopic approach (17,18). In this case, the previous operation may have aggravated or caused a certain degree of lacrimal drainage malformation. This, along with the narrow internal nasal passage, made it unfeasible to apply the endoscopic or external method alone. The external approach through the original external incision aided by the nasal endoscopic examination, and was a preferred option examination, and was a preferred option that could more fully expose and shape the lacrimal sac and the structure of the lacrimal duct, thus avoiding additional operation.
Conclusions
In conclusion, the management of patients with PL should consider the ocular anomalies and should emphasize the lacrimal drainage reconstructions. The optimal care of PL patients requires a comprehensive multidisciplinary approach that may involve an otolaryngologist, plastic surgeon, and ophthalmologist.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-501/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-501/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-501/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This case was approved by the Ethics Committee of Beijing Children’s Hospital, Capital Medical University (No. 2022-E-067-R). All procedures performed in this study were in accordance with the ethical standards of the Ethics Committee of Beijing Children’s Hospital and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sahu ES, Shroff PH, Sahu A, et al. Ophthalmic manifestations of proboscis lateralis. BMJ Open Ophthalmol 2021;6:e000558. [Crossref] [PubMed]
- Bothra N, Naik M, Ali MJ. Multiple lacrimal drainage anomalies in proboscis lateralis. Orbit 2021;40:255-7. [Crossref] [PubMed]
- Martin S, Hogan E, Sorenson EP, et al. Proboscis lateralis. Childs Nerv Syst 2013;29:885-91. [Crossref] [PubMed]
- Guerrero JM, Cogen MS, Kelly DR, et al. Proboscis lateralis. Arch Ophthalmol 2001;119:1071-4. [PubMed]
- Kolluru V, Coumary S. Proboscis Lateralis : A Rare Bilateral Case in Association with Holoprosencephaly. J Clin Diagn Res 2015;9:QD03-4. [Crossref] [PubMed]
- Acarturk S, Kivanc K, Atilla E, et al. Proboscis lateralis: evaluation of the anomaly and a review of two cases. Plast Reconstr Surg 2006;117:140e-6e. [Crossref] [PubMed]
- Shaye DA, Hakizimana A, Ndamyiyumva E, et al. Proboscis Lateralis: A Unique Window into Nasal Embryology. Facial Plast Surg Aesthet Med 2020;22:307-8. [Crossref] [PubMed]
- Khoo BC. The proboscis lateralis--a 14-year follow-up. Plast Reconstr Surg 1985;75:569-77. [Crossref] [PubMed]
- Engström O, Svee A, Hakelius M. Proboscis Lateralis: A Novel Surgical Technique Using Tape Elongation and One-Stage Tunneling. J Craniofac Surg 2022;33:e438-9. [Crossref] [PubMed]
- Zhang C, Cui Y, Wu Q, et al. Computed tomography for guidance in the diagnosis and surgical correction of recurrent pediatric acute dacryocystitis. Pediatr Investig 2019;3:39-44. [Crossref] [PubMed]
- Yildirim SV, Unal M, Barutçu O. Proboscis lateralis: a case report. Int J Pediatr Otorhinolaryngol 2001;61:179-82. [Crossref] [PubMed]
- Michelotti B, Mackay D. Nasal reconstruction. Clin Anat 2012;25:86-98. [Crossref] [PubMed]
- Galiè M, Clauser LC, Tieghi R, et al. The arrhinias: Proboscis lateralis literature review and surgical update. J Craniomaxillofac Surg 2019;47:1410-3. [Crossref] [PubMed]
- David LR, Sanger C, Fisher D, et al. Proboscis lateralis: a rare craniofacial anomaly, reconstruction, and long-term evaluation. J Craniofac Surg 2008;19:1107-13. [Crossref] [PubMed]
- Eroğlu L, Uysal OA. Proboscis lateralis: report of two cases. Br J Plast Surg 2003;56:704-8. [Crossref] [PubMed]
- Denecke, HJ, Meyer R. Plastic Surgery of Head and Neck. Vol. 1. New York: Springer-Verlag; 1967:292-8.
- Keren S, Abergel A, Manor A, et al. Endoscopic dacryocystorhinostomy: reasons for failure. Eye (Lond) 2020;34:948-53. [Crossref] [PubMed]
- Quaranta-Leoni FM, Verrilli S, Leonardi A. Surgical outcome and unusual complications of paediatric external dacryocystorhinostomy. Orbit 2019;38:187-91. [Crossref] [PubMed]


