
Acral persistent papular mucinosis: a rare child case report and literature review
Highlight box
Key findings
• Clinical diagnostic criteria should be reassessed because there is a variety of clinical manifestations. It is suggested that pathological findings should be used as the gold standard for diagnosis.
What is known and what is new?
• Acral persistent papular mucinosis (APPM) is still a rare disease and characterized by flesh-colored asymptomatic multiple papules on the back of the hands, wrists and distal forearms, most of the cases occur in adults, its pathogenesis is unclear.
• We present an APPM case of a 7-year-old boy with a solitary skin-colored nodule on the radial side of the middle segment of his right index finger.
What is the implication, and what should change now?
• Doctors should pay attention to APPM especially for pediatric patients and should not ignore it just because it is a skin disorder. More cases should be studied to reveal the pathogenesis of APPM and to evaluate the effects of treatment.
Introduction
Acral persistent papular mucinosis (APPM) is a rare localized form of lichen myxedematosus first described in 1986 by Rongioletti et al. (1) and colleagues. It is characterized by flesh-colored asymptomatic papules on the back of the hands, wrists, and distal forearms. Histologic examination shows deposition of mucin in the papillary and reticular dermis, sparing the deep dermis, fibroblastic proliferation is variable, while usually fibroblasts are not increased in number and fibrosis is absent. No systemic disease is identified, and its prognosis is invariably good. Its etiology is unknown. Therapeutic options are limited. The small number of reported cases makes the accomplishment of therapeutic trials difficult.
To date, there have been less than 41 APPM cases reported in the worldwide medical literature, not including some unpublished local literature (2,3). We present a child case and review the literature on this topic. According to PubMed, this is the rare case of child APPM reported in the world. We present this article in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-607/rc).
Case presentation
Chief complaints
A 7-year-old boy presented with a solitary skin-colored nodule on the radial side of the middle segment of his right index finger.
History of present illness
The papule gradually grew from rashes and mung bean sizes to soybean and peanut sizes within 5 years in this case. The enlarged papule affected the flexion movement of the middle segment and gradually affected the pen holding and writing of the child.
History of past illness
The patient was asymptomatic and did not complain of pruritus or pain. He denied previous insect bites, injuries, or trauma to the affected sites. There was no relationship with sun exposure. No other family member was affected. He had no past medical history. He denied any recent exposure to topical medications.
Physical examination
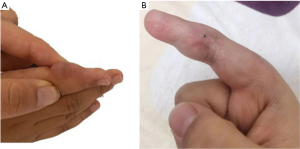
Physical examination revealed approximately 2 cm firm round skin-colored papules located exclusively on the middle segment of the right index finger (Figure 1A). Figure 1B provides a comparison of the fingers after therapy.
Laboratory examinations
The results of laboratory investigations, including routine blood examination, liver enzymes, renal function, serum protein analysis, immunoglobulin levels, thyroid studies (FT3, FT4, thyroid-stimulating hormone) and autoantibody profile were normal or negative.
Imaging examinations
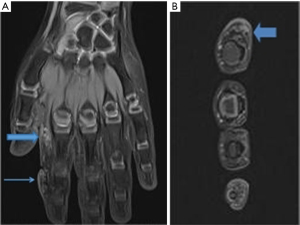
ultrasound: subcutaneous solid mass was found on the affected area of the right index finger. Magnetic resonance imaging (MRI): local subcutaneous soft tissue thickening was found around the proximal and middle phalanx of the second digit of the right hand, with internal inhomogeneity around the proximal phalanx of the right thumb, including slightly longer T1 signal and T2 signal shadow (Figure 2A,2B).
Treatment
Surgical procedure: after incision of the epidermis, the dermis was found to be thickened, and the dermis and subcutaneous tissue were disordered and interwoven in clump. The diseased tissue was gradually peeled along its surface until normal skin and subcutaneous tissue were revealed at all levels. The diseased tissue and the attached skin were excised, and the remaining two ends of the skin were sutured (Figure 1B).
Final diagnosis
Histopathological examination showed a focal and well-circumscribed deposit of mucin in the upper reticular dermis. The deposit never extended deeply into the reticular dermis. Mucin spared a subepidermal area in the papillary dermis. Alcian blue stains can highlight the mucin. fibroblastic proliferation is variable (Figure 3A,3B). The patient was diagnosed with APPM.

Outcome and follow-up
The wound gradually healed after the operation, and no obvious recurrence, scar or other discomfort was observed during follow-up so far.
Ethical consideration
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
APPM is diagnosed by its’ clinical and pathological features based on Rongioletti’s discovery in 1986. Forty-one cases have been reported in the literature up to date, 5 of which did not strictly fit the clinical characteristics of the location and the color of the disease (3-7). The etiopathogenesis is unclear, 10 of 41 cases have associated comorbidities, the others have no associated comorbidities (3,4,8-14) (Table 1).
Table 1
| No. | Gender | Age/duration (years) | Association | Evolution of the lesions | Therapy | Past-history (comorbidities) | Study |
|---|---|---|---|---|---|---|---|
| 1 | Male | 70/– | – | – | Intralesional triamcinolone injection (2.5 mg/mL) | Psoriasis | Park et al. (3) |
| 2 | Female | 60/years | – | – | ErbiumYAG laser | Hypertension | Graves et al. (4) |
| 3 | Female | 60/5 | – | Slow increase in number | – | Uterine carcinoma | Naeyaert et al. (8) |
| 4 | Female | 54/2.5 | – | Slow increase | – | Breast cancer | Gartner et al. (9) |
| 5 | Female | 55/5 | – | Increase in number | – | Hypertension and dermatitis | Harris et al. (10) |
| 6 | Male | 61/5 | – | Gradual increase | – | Papillary thyroid carcinoma | Kineston et al. (11) |
| 7 | Male | 62/– | – | Slow spread | – | Type II diabetes mellitus | Sebastian et al. (12) |
| 8 | Female | 52/5 | – | Progress | – | Breast carcinoma | Cervigón-González et al. (13) |
| 9 | Female | 31/10 | – | Gradual increase | Electrofulguration | Benign thyroid tumour | Luo et al. (14) |
| 10 | Male | 7/5 | Dysfunction | – | Surgery | Vascular malformation | Present study |
Diagnosis
The features of APPM papule are an important aspect of diagnosis. Among the 41 cases, all the cases have the same pathological characteristics such as a focal and well-circumscribed deposit of mucin in the upper reticular dermis and variable fibroblast proliferation was usually absent, while partial cases have individuation in clinical feature (3-7). APPM had not been considered before pathologic examination in this case, because the papule characteristics were not strictly consistent with the clinical characteristics of APPM, such as being multiple, 2–5 mm. Park et al. (3) reported the first case of a Korean APPM presenting as a solitary pinkish papule on the dorsum of patient’s right hand (base of thumb) in 2023, it is different from conventional diagnosis. The papule was also isolated in this case and located in the middle segment of the right index finger. This is the second patient of APPM reported so far with isolated papules. These two solitary papules are located close to the finger, and the finger flexion movement has a squeezing and rubbing effect on the papules, and the papules are larger. Papules near the joints of the fingers may be more likely to develop into larger solitary nodules. The constant occurrence of solitary papules suggests that doctors need to expand their understanding of APPM, accept the diversity of its papules, and take the pathological characteristics of papules as the gold standard for diagnosis. The mean age of the patients was 48 years (15). There were two patients under the age of 18, aged 14 (16) and 17 years (17), and plus this case, there were three patients who developed the disease before the age of 18 years. All of the three patients had no history of other medical problems, and had no obvious cause at the time of onset. Considering that the patient is in the growth and development stage, the disease will affect the health of the child with the growth and development. Preoperative B-ultrasonography showed solid nodules, and MRI results indicated that the local subcutaneous soft tissue of the proximal segment of the right index finger and the proximal segment of the right thumb had the same signal as the affected area, while the clinical manifestations of these two areas of the child’s skin were not with obvious abnormalities, and no papules were found. Whether or not APPM papules will develop in these two places is a question to be explored. The progression of these two potential lesions is important for exploring the pathogenesis of APPM. If both potential lesions progress to papules, that means removing of the first papule has no effect on the growth of subsequent nodules. APPM may be a kind of systemic disease. On the contrary, if the potential lesions are gradually degraded, it indicates that early diagnosis and early surgery may inhibit the course of APPM. Further studies are required to confirm the regulatory mechanisms of multiple papules or isolated.
Therapy and prognosis
Therapeutic options are limited, and there is no specific treatment. The small number of reported cases makes the accomplishment of therapeutic trials also difficult (15). There are anecdotal reports of treatment with topical or intralesional steroids (18) and tacrolimus (3-7) and electrosurgery (19), and erbium-YAG (yttrium aluminum garnet) laser (4) with variable results. These treatments are still in the exploratory stage, and their effects have not been widely recognized and are not reproducible. The papule gradually grew from rashes and mung bean sizes to soybean and peanut sizes within 5 years in this case. The enlarged papule affected the flexion movement of the middle segment and gradually affect the pen holding and writing of the child. The skin and subcutaneous tissue of the nodules were surgically removed, and elastic bandages were used to press the nodules. Follow-up has been performed so far, and the patients’ families are satisfied.
Etiopathogenesis
The etiology and pathogenesis of APPM are still unknown. Most patients with APPM acquire the disease independently. They had no history of medical problems and reported no use of oral or topical medications. They reported no previous injuries or trauma to the affected sites and they could establish no relationship with sun exposure (15). Among the 41 patients reported in the past, 10 had a history of disease, as shown in Table 1. There is a report of cutaneous mucinosis developing after using a biological agent, such as a tumor necrosis factor (TNF)-α inhibitor, in patients with psoriasis, however, the direct link between cutaneous mucinosis and psoriasis is not well-known, with no reported literature, five cases had a history of malignant tumor, one case was accompanied by chronic hyperlipidemia, one patient had a history of hypertension, one patient had a history of benign thyroid tumor. The possible link between APPM and malignancies has not been clarified and is probably only coincidental (15). So if it is the immune system involved in APPM? Does immune dysfunction contribute to APPM, or is the body itself immune deficient? This is a meaningful research direction. The remaining 30 cases had no obvious inducement to APPM papule, and it was not excluded that the body has a certain immune deficiency. The small number of reported cases makes the accomplishment of relationship between immunity and APPM pathogenesis trials so difficult. However, this provides a direction of research on the pathogenesis of APPM. Further studies are necessary to confirm this because of the small number of samples. The root of the affected finger was excised for vascular malformations (mainly small veins) at the age of 2, and rash-like APPM papule appeared in the middle segment of the affected finger. There is no evidence to speculate whether this history is associated with the onset of APPM. Although the etiology of APPM is yet unknown, some patients showed familial occurrence and it raises the possibility of the genetic role in APPM pathogenesis along with previous reports of familial occurrences. Family cases have shown that genetic and environmental factors play an important role (16). Our patient was at school-age, the absence of obvious predisposing factors in school-age patients also supports the suggestion that the disease is closely related to genes. Our case gives some notable points on the pathophysiology of APPM, and we hope that this case may add to the growing body of literature of APPM.
Patient perspective
The boy’s mother involved heavily in the whole process. We had a conversation with the mother before, during and after surgery in detail. She said that she understood the general treatment experience of the disease around the world, and was satisfied with the treatment process and surgical results. She was very eager to ask how to avoid recurrence after surgery, how to care to avoid the disease in daily life, what are the genetic characteristics of the disease. She is very much looking forward to more research from doctors around the world to relieve the pain caused by APPM to her child, while guiding fertility to avoid affecting the next generation.
Conclusions
APPM is still a rare disease, its pathogenesis is unclear. There is a variety of clinical manifestations. It is suggested that pathological findings should be used as the gold standard for diagnosis. When the lesion papules are located in the finger and the age of the patient is young, active treatment should be taken to avoid the finger function of the child being affected. As APPM is a skin disorder that may easily be ignored by both patients and doctors, we believe that it is more common than the number of cases being reported in the literature. We urge everyone to be vigilant for pediatric patients. Considering the factors of growth and development, any neglected disease can cause harm to the health of the child. This is worrying and anxious. A longer follow-up is needed and more cases should be studied to reveal the pathogenesis of APPM and to evaluate the effects of treatment. Since it is a rare disease, we report this case to contribute to future research on the diagnosis and pathogenesis of APPM.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-607/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-607/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-607/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s legal guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rongioletti F, Rebora A, Crovato F. Acral persistent papular mucinosis: a new entity. Arch Dermatol 1986;122:1237-9.
- Mori A, Shinkuma S, Mitsui Y, et al. Acral persistent papular mucinosis: A case report and summary of 24 Japanese cases. J Dermatol 2021;48:1574-8. [Crossref] [PubMed]
- Park YJ, Shin HY, Choi WK, et al. Solitary acral persistent papular mucinosis nodule: A case report and summary of eight Korean cases. World J Clin Cases 2023;11:3086-91. [Crossref] [PubMed]
- Graves MS, Lloyd AA, Ross EV. Treatment of acral persistent papular mucinosis using an Erbium-YAG laser. Lasers Surg Med 2015;47:467-8. [Crossref] [PubMed]
- Madan V, Gangopadhyay M, Dawn G. Multiple asymptomatic papules on the legs. Clin Exp Dermatol 2007;32:773-4. [Crossref] [PubMed]
- Jun JY, Oh SH, Shim JH, et al. Acral Persistent Papular Mucinosis with Partial Response to Tacrolimus Ointment. Ann Dermatol 2016;28:517-9. [Crossref] [PubMed]
- Navarrete-Dechent C, Bajaj S, Marghoob A, et al. Acral persistent papular mucinosis (APPM): Dermoscopy of an uncommon disease. J Am Acad Dermatol 2017;76:S10-1. [Crossref] [PubMed]
- Naeyaert JM, Geerts ML, Kudsi S, et al. Acral persistent papular mucinosis: a peculiar variant of the discrete papular form of lichen myxedematosus. Arch Dermatol 1990;126:1372-4.
- Gartner S, Schoppelrey HP, Agathos M, et al. Acral papular lichen myxedematosus. Hautarzt 1998;49:855-8. [Crossref] [PubMed]
- Harris JE, Purcell SM, Griffin TD. Acral persistent papular mucinosis. J Am Acad Dermatol 2004;51:982-8. [Crossref] [PubMed]
- Kineston DP, Willard RJ, Krivda SJ. Flesh-colored papules on the wrists of a 61-year-old man. Arch Dermatol 2004;140:121-6. [Crossref] [PubMed]
- Sebastian S, Zlotoff B, DeSantis E. 'Spreading bumps' on hands of a Native American. Clin Exp Dermatol 2008;33:225-7. [Crossref] [PubMed]
- Cervigón-González I, Torres-Iglesias LM, Palomo-Arellano A, et al. Papules on the dorsum of the hands. Actas Dermosifiliogr 2008;99:731-2.
- Luo DQ, Wu LC, Liu JH, et al. Acral persistent papular mucinosis: a case report and literature review. J Dtsch Dermatol Ges 2011;9:354-9. [Crossref] [PubMed]
- Rongioletti F, Ferreli C, Atzori L. Acral persistent papular mucinosis. Clin Dermatol 2021;39:211-4. [Crossref] [PubMed]
- Menni S, Cavicchini S, Brezzi A, et al. Acral persistent papular mucinosis in two sisters. Clin Exp Dermatol 1995;20:431-3. [Crossref] [PubMed]
- Barba A, Maruccia A, D'Onghia FS. Persistent acral papulous mucinosis. Ann Dermatol Venereol 1996;123:256-8.
- Iglesias-Plaza A, Melé-Ninot G, Pérez-Muñoz N, et al. Acral persistent papular mucinosis with pruritic skin lesions. An Bras Dermatol 2018;93:769-70. [Crossref] [PubMed]
- André Jorge F, Mimura Cortez T, Guadalini Mendes F, et al. Treatment of acral persistent papular mucinosis with electrocoagulation. J Cutan Med Surg 2011;15:227-9. [Crossref] [PubMed]


