
Pain management after pediatric minimally invasive repair of pectus excavatum: a narrative review
Introduction
Pectus excavatum is the most common congenital chest wall deformity, affecting 1 in 400 births (1,2), and is characterized by a concave depression of the anterior chest wall (3). Pectus excavatum can be associated with significant psychosocial and clinical implications including cardiac and pulmonary compression, restrictive lung physiology, and significant body image concerns (2). The traditional open technique for repair of pectus excavatum, often called the modified Ravitch procedure, involves the subperichondrial resection of the affected costal cartilages and transverse osteotomy of the sternum in order to reshape the chest. This technique has largely been replaced with the minimally invasive repair of pectus excavatum (MIRPE), often called the Nuss procedure, which involves placing a substernal curved metal bar under thoracoscopic guidance without disrupting the sternum or rib attachments (2,4). While this technique uses smaller incisions and avoids the tissue disruption and scar formation associated with the open approach, it is perhaps the only minimally invasive operation that may result in increased postoperative pain than its open counterpart. This is thought to be due to the acute stretching of the intercostal nerves and chest wall, with prolonged mechanical loading of the chest wall by the substernal bar, until bone and cartilage remodeling occurs (5,6).
Effective postoperative pain management is crucial for not only improving patient comfort but also for facilitating earlier mobilization, shortening hospital length of stay (LOS), and reducing complications such as atelectasis or pneumonia (7). Traditionally, patient-controlled analgesia (PCA) and thoracic epidural analgesia (TEA)—techniques previously employed for open repair—were utilized for pain management after MIRPE. However, growing clinical experience with MIRPE revealed that these analgesia approaches were suboptimal given the degree and duration of postoperative pain with MIRPE. With the ongoing opioid epidemic, modern practice has emphasized targeted therapies and non-opioid pain medications. The majority of pain following MIRPE stems from the intercostal nerves. Local analgesia targeting these nerves has been the mainstay of management, including TEA, intercostal nerve cryoablation (INC), intercostal nerve blocks (INBs), and regional nerve catheter techniques (8-14). Enhanced recovery after surgery (ERAS) pathways have been implemented successfully after MIRPE (15-17) focusing on multimodal pain management to address physical and psychological pain and distress after surgery (18). ERAS is a patient-centered approach that employs strategies to help patients recover effectively from surgery by implementing steps such as early ambulation, oral intake, and removal of urinary catheters.
Overall, pain management techniques vary across institutions and there are limited randomized controlled trials and a lack of consensus for optimal technique following repair. This review aims to evaluate contemporary and historic pain management after MIRPE and provide an overview of the outcomes, advantages, limitations, and efficacy of various modalities. Through synthesizing current evidence and clinical experience, this article seeks to inform best practices on perioperative pain management for MIRPE. We present this article in accordance with the Narrative Review reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-24-339/rc).
Methods
This manuscript is a narrative review of the current literature on perioperative pain management surrounding MIRPE. Table 1 summarizes our search strategy which examines the study, analysis, and discussion of previously published journal articles specific to the perioperative pain management of pectus excavatum in pediatric patients. Our focus was on recent literature over the past 15 years, 2010–2024, however, additional studies were included when appropriate. Published material was found through the PubMed® (National Center for Biotechnology Information, United States National Library of Medicine, National Institutes of Health) database using combinations of the keywords: pectus excavatum, pediatric, pain management, minimally invasive repair of pectus excavatum (MIRPE), and enhanced recovery after surgery (ERAS). The initial and secondary searches were performed by the authors, and a certified librarian performed an additional search. The articles were then examined for relevancy and the references were also reviewed for additional citations. Only articles published or available in English were included. Case reports were only included when discussing first reported use or rare complications. The importance of the articles was based on the level of evidence. The authors evaluated each article and decided on article inclusion after analysis.
Table 1
| Items | Specification |
|---|---|
| Date of search | Initial search was conducted on April 25th, 2024. A secondary search was conducted on June 20th, 2024. A librarian search was conducted on July 18th, 2024 |
| Databases | PubMed |
| Search terms | Pectus excavatum, pediatric, pain management, minimally invasive repair of pectus excavatum (MIRPE), enhanced recovery after surgery (ERAS) |
| Timeframe | Focused on articles 2010–2024, additional studies included for relevance |
| Inclusion and exclusion criteria | Included randomized control trials, clinical trials, meta-analyses, cohort studies, and book chapters |
| Excluded articles not available in English or most case reports. Some case reports were included to discuss first reported use or rare complications | |
| Selection process | Initial and secondary searches were conducted by authors, additional search was conducted by a librarian. The final list was compiled and refined by the authors |
Considerations of perioperative pain management
Perioperative pain control after MIRPE is challenging given that pain management can be affected by a multitude of factors. With a shift to minimally invasive repair, patients experience pain disproportionate to their incision sizes from the instantaneous and extreme reshaping of their chest wall during the procedure. In addition, as the bony chest wall is not fractured or otherwise disrupted, the substernal bar placed during MIRPE exerts a significant and prolonged upward force on the chest wall, until remodeling of the chest wall occurs. Persistent postoperative pain is not uncommon and contributes to extended lengths of stay and increased postoperative opioid consumption (19,20). Inadequate pain control can have lasting negative consequences including pain memory, behavioral disorders, and chronic pain. Another consideration is that pain measurements are largely obtained through pain scoring which is a subjective measure and dependent on patient self-report. The current pain scales used in recent literature are the Visual Analog Scale (VAS) Pain Scale, the Faces Pain Scale-Revised, and the Numeric Rating Scale (14,19,21-26). This is an area where better tools may need to be developed to more accurately measure pain in the pediatric population (20). Pediatric pain evaluations should include functional assessments of movement (moving in bed, sitting up, walking, etc.) and PO (per os or by mouth) intake.
Additionally, pain pathways are complex. There has been a shift towards preventive analgesia, which blocks pain inputs prior to incision, to mitigate central sensitization of pain contributing to chronic pain. Given the current opioid epidemic, efforts have been made to decrease opioid dependence and associated hyperalgesia. Thus, a focus on multimodal analgesia has been emphasized to counter over-reliance on opioids. Multimodal pain management allows for lower doses of individual drugs, reducing side effects, but preserving overall efficacy. The goal of this practice is to reduce the chance of central sensitization, optimize pain control, and avoid the adverse effects of opioid overuse. Applications of this have been shown to be effective for several surgical procedures, including MIRPE (27-29). Multimodal analgesia strategies involve a combination of regional anesthesia, local infiltration anesthetic, and non-opioid systemic analgesic adjuvants over opioids (30,31). These regimens have become increasingly standardized, becoming a part of the ERAS pathways. We will be discussing each of these analgesic modalities, including epidurals, PCA, regional blocks, and additional analgesic adjuncts, as well as describing current efforts in standardized pain protocols and their efficacies.
Multimodal pain management
TEA and epidural catheters
Thoracic epidural catheters deliver local anesthetics and other analgesics into the thoracic epidural space, providing effective pain relief by targeting intercostal nerves. Historically, thoracic epidurals were the gold standard and most effective means of controlling pain after pectus excavatum repair (9,11,32-36). However, the benefits are not without risks as epidurals are associated with rare but serious complications including epidural hematoma, infection, and rare neurological paraplegias. In addition, epidurals have been shown to result in more calls to anesthesia providers, longer operative times, greater hospital charges, higher rates of infection, respiratory depression, hypotension, and greater urinary retention (6,26,36-39). Permanent neurological complications are very uncommon in children with only a few reported pediatric cases (40), but have a reported risk of around 0.04–0.07% in the adult population (41,42). Although epidurals are sufficient for pain management after MIRPE in some patients, a cohort study of 203 patients found that 65 of 188 patients who received epidural catheters had inadequate pain control (43). Many retrospective studies found epidurals to be inferior to newer analgesic modalities, either in analgesic effect or side effect profile, such as PCAs or regional pain blocks (6,44-51). Despite mixed study outcomes comparing epidurals and PCA for pain management after MIRPE (22,26,34), a 2014 survey of 108 pediatric hospitals in North America, Europe, Australia, and Asia showed that the majority of (91%) hospitals utilized thoracic epidurals with only 27% using concomitant PCA after MIRPE (6). Given the evolution of postoperative MIRPE pain management, TEA has become the control comparison in multiple cohort studies and referenced in a systematic review, which will be discussed later. While newer methods may have improved efficacy for pain control, indications for epidurals are still warranted, given patient factors, resource availability, and provider familiarity.
PCA
PCA allows patients to self-administer predetermined doses of analgesics providing personalized pain management tailored to the patients’ needs. PCAs have been used in place of or in addition to TEA after MIRPE. Studies looking at safety and efficacy outcomes have been mixed when compared to regional analgesia.
A cohort study showed that PCA compared to TEA decreased time to oral opioid transition, reduced postoperative opioid consumption, urinary catheterizations, and shortened hospital stays (52). However, a systematic review and meta-analysis from 2014 as well as several recent smaller reviews found that PCA may be less effective in relieving pain and reducing opioid use compared to epidural analgesia and nerve blocks (14,22,26,34,35,43,53). Additional concerns with PCA include respiratory depression, nausea, and vomiting associated with systemic opioid use, although select studies report similar rates of nausea and sedation between epidural analgesia and PCA (34,35). With this in mind, in comparison to TEA, many regard PCA as superior given that it is non-invasive, has low complication rates, and is more cost-effective (44). As multimodal regimens are being increasingly implemented, PCA, while not the sole mode of analgesia, remains an adjunct that has been utilized to achieve adequate pain control.
INC
The application of INC, as shown in Figure 1, in the Nuss procedure has revolutionized perioperative pain management since its first reported use in MIRPE in 2016, although historically it had been used since 1974 to prevent post-thoracotomy pain (54,55). Cryoablation induces Wallerian degeneration of nerve axons using extreme cold temperatures with a cryoprobe, halting pain transmission for approximately 4 to 6 weeks until the axons regenerate, with a recent study showing recovery from 3–6 months or longer (8,56,57). For MIRPE, cryoablation is typically performed for intercostal nerves 3–7 bilaterally. Keller and colleagues in 2016 were the first to utilize INC after the Food and Drug Administration (FDA) approved the first commercially available cryoablation probe in 2015. Its intended use was for temporary ablation of peripheral nerves. Keller et al. looked at its effects on postoperative analgesia compared to TEA through a multi-institutional review and found that it reduced hospital LOS from 3.73 to 1.88 days, and decreased intravenous narcotic use from 119.8 to 49.03 mg. The results were so promising that they reported eliminating the use of epidurals from their practice (58). Since 2016, there have been many studies highlighting the benefits of cryoablation including improved pain control, reduction of LOS, and minimized opioid requirement postoperatively (7-9,57-59) compared to TEA and regional catheters. In 2019, Graves and colleagues performed one of the first prospective randomized clinical trials looking at INC, which was consistent with Keller et al.’s findings that INC patients had decreased LOS (5 to 3 days), less inpatient opioid consumption (mean decrease of 416 MME) compared to TEA patients with equivalent pain control and no difference in adverse effects (8). Daemen et al. later on in 2020 incorporated this and 4 other observational studies as a systematic review and meta-analysis examining INC to thoracic epidurals after MIRPE, which found that INC was associated with reduced hospital LOS and decreased hospital opioid use (8,9,58,60,61). Additional studies found a reduction in complications such as ileus (8,9,62,63) and noted fewer risks related to sensory and motor function impairment in the lower limbs, reduced urinary retention, and reduced infection compared to TEA (61,64).

The primary risk of concern has been the reported incidences of postoperative neuropathic pain, primarily in adult patients. Zobel et al. (65) conducted a multicenter study of patients undergoing INC with MIRPE from 2015–2018, using a validated questionnaire for detecting neuropathic symptoms. Among patients over 21, however, 3 of 13 experienced neuropathic pain. Among patients under 21 years of age, zero patients experienced neuropathic pain (65). While neuropathic pain is a possible complication of INC, incidence in the pediatric population is lower, but should still be monitored postoperatively. Another consideration of the procedure is the cost of the cryoablation probe and equipment, as shown in Figure 1A-1C. The device studied most in the MIRPE population in the US is the Cryosphere device (Atricure, Inc., Mason, OH, USA), a disposable probe that is FDA-approved for patients 12 years of age and older. Also to note, there have been some studies that show increased operative times compared to other modalities, consistent with the time needed to perform cryoablation during the procedure (for the current generation Cryosphere+ device, it requires 90 seconds per nerve). However, despite an average increase in operating room time of 78 minutes, in a retrospective study, Aiken and colleagues (66) found that bilateral INC was associated with decreased resource utilization due to shorter hospital stay, with no effect on readmission rates. Additional manufactures, such as the Cryo-S Painless device with cryoprobe A-30/PEA/R/RF (Metrum Cryoflex, Blizne Laszczyn-skiego, Stare Babice, Poland), Cardioblate CryoFlex Surgical Ablation Console (Medtronic Inc., Minneapolis, MN, USA), and others, have created cheaper alternatives that have also been studied with similar results of shorter LOS and decreased postoperative opioid requirements (67) as well as shown that decreasing application time to 60 seconds from 120 seconds did not change pain control (68).
Another concern for INC is the risk of inadvertent lung injury from the cryoprobe as it is cooling. Once the probe is engaged in its desired location, the ablation cycle is started and once complete the probe is warmed to allow release from the area without traction (58). Thus, there is limited mobility of the cryoprobe during the ablation cycle, which if not able to create adequate exposure, can result in cryoinjury to the lung. In order to reduce this complication, lung isolation and controlled deflation are important in providing adequate exposure during INC. Many surgeons when performing INC have now opted for double-lumen endotracheal tube intubation to achieve this lung isolation (69).
Finally, a key limitation of INC is the delay in effect, as the axonal degeneration can take 12–24 hours to complete after INC. Thus, there has been shown to be a shift in opioid use to earlier in the admission period, with some studies noting up to 24 hours until the full effect of INC (7,60). One small prospective study by Velayos et al. in 2023 (70) examined this delay in analgesic effect comparing INC at the time of surgery or 48 hours before surgery and found that preoperative INC was associated with a lower number of continuous PCA use, rescue boluses, VAS pain scores, and lower median LOS. However, performing early preoperative INC involves an additional procedure with added anesthetic induction and duration (71). Additional studies to maximize the efficacy of cryoablation have included further study of the intercostal nerve by Talsma et al. in 2023, which found that the collateral branch of the intercostal nerve travels below the rib as opposed to the other two branches: the lateral cutaneous and anterior cutaneous branches. This has led to changes in technique and development of technology that target all three branches as well (72). Future research would benefit from additional multi-center, prospective randomized control trials to help us evaluate the efficacy and limitations of INC, as well as identify strategies to bridge the early postoperative analgesia gap after INC. While this need can be fulfilled with systemic opioids (i.e., PCA), growing evidence supports the use of regional blocks as an effective opioid-sparing method to bridge this gap.
Regional plane blocks: single or continuous infusion
Regional plane blocks have been shown to be an effective modality in pain management for MIRPE, either as a single dose or continuous infusion. These blocks include thoracoscopic or ultrasound-guided percutaneous INBs, serratus anterior plane blocks (SAPBs), paravertebral nerve blocks (PVBs), and erector spinae plane blocks (ESPBs), some of which are shown in Figures 2,3.


INB is the infiltration of local anesthetic (short or long-acting) directly into the plane between the parietal pleura and the intercostal muscles. This is performed at each intercostal level, usually levels 3 through 7 on each side, and can be performed via a trans-thoracic approach (Figure 2), or an external percutaneous approach. INB has been shown to result in lower central nervous system depression, reduced opioid use, and improved pulmonary mechanics (24,73). In a prospective randomized study by Luo et al. in 2017, pediatric patients with INB had decreased pain scores in the first 6 hours, decreased opioid use in the first 24 hours, and faster discharge compared to patients who received PCAs with a lower incidence of analgesia-associated side effects (14). This was further supported by a 2022 randomized, double-blind control trial by Ma et al., which found lower pain scores at postoperative days 1–3 and decreased opioid use 48 hours postoperatively in those receiving PCA and INB compared to PCA alone (74). There is limited literature in pediatric MIRPE comparing INB to other regional blocks. However, in a 2021 systematic review of adults undergoing thoracic surgery, INB was found to be associated with a reduction in pain in the first 24 hours after surgery and equivalent to TEA but was marginally inferior to PVB (12). While there are some studies supporting its benefits, further studies comparing INB to regional plane blocks in pediatric MIRPE will help us understand the best settings for the use of INB.
SAPBs are single or continuous regional pain blocks administered through an extrathoracic catheter, targeting T2 to T9 intercostal nerves traversing through the serratus anterior plane. Benefits of SAPB include extrathoracic administration without the need for a thoracoscopic approach, single-lung ventilation, and additional equipment and instrumentation. There have been limited studies showing its benefit; however, a single-center retrospective study in 2024 by Ka et al. revealed that it is superior to intravenous PCA and subcutaneous local anesthetic with significantly lower pain levels and lower morphine milligram equivalents (MMEs) at 72 hours postoperative (75). Another pending study by He and colleagues is looking to evaluate the effect of SAPB compared to PVB with a prospective, randomized, double-blind non-inferiority trial (76). Further studies like these will continue to help clinicians tailor postoperative pain management after MIRPE.
Compared to INBs and SAPBs, PVBs and ESPBs apply local anesthetic more proximally at the dorsal and ventral aspects of the spinal nerve as it emerges from the spine, as shown in Figure 3. These techniques are designed to block the nerve proximal to any peripheral branches, thus providing a denser and wider sensory block. A systematic review in 2020 on postoperative pain control following pectus repair concluded that opioid use decreased in 75% of studies evaluating PVB and INB compared to PCA (19,25). Chen et al. in 2023 also found that PVB reduced the hospital LOS and decreased postoperative nausea and vomiting compared to thoracic epidurals, indicating that although nerve blocks are not as efficacious for pain management compared to epidurals, they may lead to fewer side effects (45-48). While the 2021 review by Guerra-Londono et al. (12) found that PVB may be marginally superior to INB in the setting of adult thoracic surgery, there is again limited data directly comparing these blocks in pediatric MIRPE, however, recently there has been new literature comparing PVB to INC. In 2023, Zeineddin et al. found that PVB had longer LOS, higher hospital costs, and increased opioid use compared to INC with a minimal decrease in operating time (average of 9 minutes) (77). While not as effective as INC in direct comparison, research on the efficacy of PVB compared to other modalities is limited to institutional cohort studies with inherent risk for bias and lacking prospectives randomized control trials. However, the current evidence does suggest that PVB may be indicated given its benefits compared to historic regimens and may be utilized as an adjunct to INC.
Finally, ESPBs are single or continuous regional pain blocks that deliver local anesthetics to the paraspinal fascial plane between the erector spinae muscle and the thoracic transverse processes targeting the dorsal and ventral rami for analgesia of the lateral, anterior, and posterior thoracic walls, seen in Figure 3 (10). Since Nardiello and Herlitz first used ESPBs for the Nuss procedure with reported success in 2018 (78), ESPBs have been utilized as the primary modality for postoperative chest surgery pain management as well as a bridge until the full effect of INC is achieved. A number of cohort studies have found that patients undergoing surgery for pectus excavatum who received these were faster to achieve pain relief, stop opioid use, and reach independent physical activity and rehabilitation compared to those that received TEA without any ESPB-related complications (71,79), providing evidence that ESPB can be a safe alternative to TEA. In a systematic review by Chen et al. in 2023, they found a reduction in hospital LOS and decreased postoperative nausea and vomiting compared to TEA (45,49-51). However, this review was limited due to small number of studies with no randomized control trials. Additionally, ESPBs were also shown to be an effective adjunct with INC compared to INC alone (80). Although promising as a pain management modality with some literature in adult thoracic surgery finding similar efficacy with PVB and fewer side effects, such as hypotension (81), there is still limited literature on the comparison of ESPBs with other regional blocks in pediatric MIRPE outside of institutional cohort studies. Future research will be important in further establishing ESPB as an effective postoperative pain management modality for pediatric MIRPE.
With the implementation of these regional pain blocks, another avenue of interest has been the composition of the local anesthetic agent administered. The half-life of local anesthetics is relatively short and may not provide durable pain coverage after surgery. Thus, there has been expansion into looking at a mixture of traditional local anesthetics with adjuvants such as epinephrine, clonidine, nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and more to help prolong the duration of analgesia, either to address post-MIRPE pain definitively, or to serve as a bridge until INC onset. Multiple of these adjuvants have been utilized and shown effective in prolonging analgesic duration in peripheral nerve blocks (82). Bhatnagar et al. in 2006 found that the addition of clonidine to PVB lowered pain scores at multiple time points in patients undergoing thoracotomy (83). However, it has more recently been of interest in the setting of regional pain blocks in MIRPE given the increased use of INC and the need for additional adjuncts within the first 24 to 48 hours. In 2024, Li and colleagues found the use of a cocktail of dexamethasone, sodium bicarbonate, magnesium sulfate, dexmedetomidine, methylprednisolone, and ropivacaine to be more effective in analgesia after discharge compared to traditional pain block cocktails with fewer analgesic-related adverse events (84). While promising, further studies regarding these adjuncts in regional plane blocks need to be explored to better understand their implications in MIRPE pain management.
Additional treatment adjuncts
In addition to many of these treatments, many patients are given non-opioid multimodal oral and intravenous analgesic medications, including but not limited to acetaminophen, NSAIDs, magnesium, alpha-2 agonists, N-methyl-D-aspartate (NMDA) receptor antagonists, gabapentinoids, glucocorticoids/corticosteroids, anti-anxiolytics, and anesthetics (i.e., ketamine) (30). To combat some side effects associated with narcotic use, patients are often given a standard bowel regimen and naloxone (85,86).
More recently, methadone has begun to be introduced into multimodal analgesic methods. As a long-acting opioid with a half-life of 24 to 36 hours, it is an effective adjunct after surgery and a bridge for INC. Singhal et al. in 2016 (87) sought to evaluate its use in MIRPE and found that a single intraoperative dose of methadone was shown to reduce total opioid use, time with uncontrolled pain, and LOS compared to epidural with general anesthesia and multimodal analgesia without any significant difference in adverse events. Sadhasivam et al. in 2021 looked further into methadone treatment in pediatrics, specifically studying dosage-dependent effects with multiple small perioperative methadone doses, and found it resulted in lower blood methadone levels that was previously associated with side effects, such as respiratory depression and QT interval prolongation, and still maintained significant opioid-sparing analgesia (88). With the implementation of INC, a more recent study in 2024 looked at its use with INC to bridge the time until its onset and found a trend towards improved pain control within the first 24 hours after Nuss procedure (13). While its use in perioperative pain management continues to expand, not only in MIRPE but in other fields as well (89,90), larger randomized trials are needed to elucidate its efficacy.
Finally, local subcutaneous injections at sites of surgery/chest tubes are widely used. However, its benefits may not be as profound as other pain management modalities given that the pain is due to the stretching of the intercostals that is not incisional in nature. With little drawback and as part of the standard of care, local subcutaneous analgesia at surgical sites is routinely performed.
ERAS
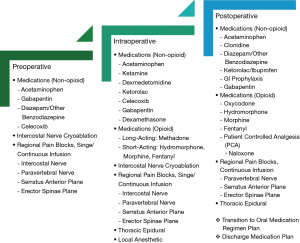
Given MIRPE’s unique considerations in pain management, an increasing number of centers are implementing ERAS pathways. These protocols are usually focused on three stages of interventions: preoperative, intraoperative, and postoperative, using a combination of multimodal agents and postoperative recovery initiatives (85,91). Standardization of this perioperative care has been known to lead to improved surgical outcomes, especially in adult populations (16,27,91). For example, in adults undergoing MIRPE, there is evidence to support the use of ERAS in conjunction with cryoablation compared to previous groups of TEAs and other continuous subcutaneous catheters. ERAS and cryoablation were associated with decreased LOS, reduction in opioid use, and lower incidence of opioid-related complications including constipation and ileus (61). Given that many institutions implemented ERAS pathways concurrently with cryoablation, it is difficult to see the effect of an ERAS pathway alone. However, it is evident that these pathways are effective and becoming increasingly accepted. Overall benefits of transitioning to an ERAS pathway or standardized protocol include reduced hospital LOS, immediate postoperative pain scores, opioid use, and nausea/vomiting (85) without an increase in readmissions or emergency room visits (16). Additional technology using eHealth has also enhanced some clinical pathways with at-home monitoring (18), although generalizable benefits and resource utilization need to be further studied. Overall, the development of an ERAS pathway focus should be on preventative, multimodal, and patient-centered analgesia. We have provided a compiled list of considerations and options for multimodal agents at each stage for reference in Figure 4, as well as a list of other practice considerations as part of ERAS for MIRPE in Figure 5 (13,15-18,27,63,87,91-94). Through this review, our institution has incorporated some of these considerations with our institutional workflow and resources in mind to update our ERAS protocol after MIRPE, as shown in Figure 6 with the full protocol as Appendix 1. Given these broad considerations, we understand that this pathway may look different in varying clinical settings due to resource, staffing, supply chain, and patient insurance limitations as well as practice patterns per individual institution. As more avenues of pain management are studied, these protocols need to be continuously updated.


With the advancement of multimodal analgesia, incorporation of INC, introduction of multiple regional pain blocks, and protocolization of perioperative pain management, implementation of ERAS or institutional protocols has significantly shortened hospital lengths of stay from 4–5 days as described by Nuss and Kelly in 2010 (38) to now same-day discharge in 2022 by Rettig et al. (95,96) and in 2023 by Akinboro et al. (97), as well as decreased opioid use without additional increases in the cost of hospital stay (65). Since the development of the Nuss procedure in 1987 (4), all of these advancements in perioperative pain management have revolutionized the postoperative course for patients undergoing MIRPE.
Conclusions
While the unique breadth and duration of postoperative pain after MIRPE presents a particular challenge, the anatomic advantage of accessible segmental nerve supply to the affected area has created an opportunity for innovation in regional pain management techniques. Contemporary cornerstones of pain management after MIRPE include INC, regional nerve block techniques, and multimodal opioid-sparing strategies. ERAS pathways and institutional protocols are now becoming increasingly popular and transforming postoperative MIRPE pain management. Future research should be focused on randomized control trials on the comparison of these multimodal agents, large scale prospective studies regarding standardized protocols and their long-term outcomes, and improved methods of assessing pain, with the aim to continue improving overall patient outcomes and experience after MIRPE.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-24-339/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-24-339/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-24-339/coif). F.R.D. serves as an unpaid editorial board member of Translational Pediatrics from February 2023 to January 2025. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from all patients’ parents or legal guardians for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Obermeyer RJ, Goretsky MJ. Chest wall deformities in pediatric surgery. Surg Clin North Am 2012;92:669-84. ix. [Crossref] [PubMed]
- Scalise PN, Demehri FR. The management of pectus excavatum in pediatric patients: a narrative review. Transl Pediatr 2023;12:208-20. [Crossref] [PubMed]
- Fokin AA, Steuerwald NM, Ahrens WA, et al. Anatomical, histologic, and genetic characteristics of congenital chest wall deformities. Semin Thorac Cardiovasc Surg 2009;21:44-57. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 1998;33:545-52. [Crossref] [PubMed]
- Ghionzoli M, Brandigi E, Messineo A, et al. Pain and anxiety management in minimally invasive repair of pectus excavatum. Korean J Pain 2012;25:267-71. [Crossref] [PubMed]
- Muhly WT, Maxwell LG, Cravero JP. Pain management following the Nuss procedure: a survey of practice and review. Acta Anaesthesiol Scand 2014;58:1134-9. [Crossref] [PubMed]
- Breglio AM, Fitzgerald TN, Moore CB, et al. Evaluation of Analgesic Practice Changes Following the Nuss Procedure in Pediatric Patients. J Surg Res 2023;291:289-95. [Crossref] [PubMed]
- Graves CE, Moyer J, Zobel MJ, et al. Intraoperative intercostal nerve cryoablation During the Nuss procedure reduces length of stay and opioid requirement: A randomized clinical trial. J Pediatr Surg 2019;54:2250-6. [Crossref] [PubMed]
- Harbaugh CM, Johnson KN, Kein CE, et al. Comparing outcomes with thoracic epidural and intercostal nerve cryoablation after Nuss procedure. J Surg Res 2018;231:217-23. [Crossref] [PubMed]
- Forero M, Adhikary SD, Lopez H, et al. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med 2016;41:621-7. [Crossref] [PubMed]
- Densmore JC, Peterson DB, Stahovic LL, et al. Initial surgical and pain management outcomes after Nuss procedure. J Pediatr Surg 2010;45:1767-71. [Crossref] [PubMed]
- Guerra-Londono CE, Privorotskiy A, Cozowicz C, et al. Assessment of Intercostal Nerve Block Analgesia for Thoracic Surgery: A Systematic Review and Meta-analysis. JAMA Netw Open 2021;4:e2133394. [Crossref] [PubMed]
- Rook JM, Lee LK, Wagner JP, et al. Six Years of Quality Improvement in Pectus Excavatum Repair: Implementation of Intercostal Nerve Cryoablation and ERAS Protocols for Patients Undergoing Nuss Procedure. J Pediatr Surg 2024;S0022-3468(24)00430-5.
- Luo M, Liu X, Ning L, et al. Comparison of Ultrasonography-guided Bilateral Intercostal Nerve Blocks and Conventional Patient-controlled Intravenous Analgesia for Pain Control After the Nuss Procedure in Children: A Prospective Randomized Study. Clin J Pain 2017;33:604-10. [Crossref] [PubMed]
- Yu P, Wang G, Zhang C, et al. Clinical application of enhanced recovery after surgery (ERAS) in pectus excavatum patients following Nuss procedure. J Thorac Dis 2020;12:3035-42. [Crossref] [PubMed]
- Wharton K, Chun Y, Hunsberger J, et al. Successful use of an enhanced recovery after surgery (ERAS) pathway to improve outcomes following the Nuss procedure for pectus excavatum. J Pediatr Surg 2020;55:1065-71. [Crossref] [PubMed]
- Cramm SL, Luckhurst C, Galls A, et al. Thoracic epidural-based Enhanced Recovery After Surgery (ERAS) pathway for Nuss repair of pectus excavatum shortened length of stay and decreased rescue intravenous opiate use. Pediatr Surg Int 2021;37:1191-9. [Crossref] [PubMed]
- Wildemeersch D, D'Hondt M, Bernaerts L, et al. Implementation of an Enhanced Recovery Pathway for Minimally Invasive Pectus Surgery: A Population-Based Cohort Study Evaluating Short- and Long-Term Outcomes Using eHealth Technology. JMIR Perioper Med 2018;1:e10996. [Crossref] [PubMed]
- Archer V, Robinson T, Kattail D, et al. Postoperative pain control following minimally invasive correction of pectus excavatum in pediatric patients: A systematic review. J Pediatr Surg 2020;55:805-10. [Crossref] [PubMed]
- Manworren RCB, Di Franco MV, Mishra T, et al. Pain Quality After Pediatric Pectus Excavatum Repair. Pain Manag Nurs 2022;23:811-8. [Crossref] [PubMed]
- Bryskin RB, Robie DK, Mansfield FM, et al. Introduction of a novel ultrasound-guided extrathoracic sub-paraspinal block for control of perioperative pain in Nuss procedure patients. J Pediatr Surg 2017;52:484-91. [Crossref] [PubMed]
- Butkovic D, Kralik S, Matolic M, et al. Postoperative analgesia with intravenous fentanyl PCA vs epidural block after thoracoscopic pectus excavatum repair in children. Br J Anaesth 2007;98:677-81. [Crossref] [PubMed]
- Cha MH, Eom JH, Lee YS, et al. Beneficial effects of adding ketamine to intravenous patient-controlled analgesia with fentanyl after the Nuss procedure in pediatric patients. Yonsei Med J 2012;53:427-32. [Crossref] [PubMed]
- Lukosiene L, Rugyte DC, Macas A, et al. Postoperative pain management in pediatric patients undergoing minimally invasive repair of pectus excavatum: the role of intercostal block. J Pediatr Surg 2013;48:2425-30. [Crossref] [PubMed]
- Qi J, Du B, Gurnaney H, et al. A prospective randomized observer-blinded study to assess postoperative analgesia provided by an ultrasound-guided bilateral thoracic paravertebral block for children undergoing the Nuss procedure. Reg Anesth Pain Med 2014;39:208-13. [Crossref] [PubMed]
- St Peter SD, Weesner KA, Weissend EE, et al. Epidural vs patient-controlled analgesia for postoperative pain after pectus excavatum repair: a prospective, randomized trial. J Pediatr Surg 2012;47:148-53. [Crossref] [PubMed]
- Leeds IL, Boss EF, George JA, et al. Preparing enhanced recovery after surgery for implementation in pediatric populations. J Pediatr Surg 2016;51:2126-9. [Crossref] [PubMed]
- Wren AA, Ross AC, D'Souza G, et al. Multidisciplinary Pain Management for Pediatric Patients with Acute and Chronic Pain: A Foundational Treatment Approach When Prescribing Opioids. Children (Basel) 2019;6:33. [Crossref] [PubMed]
- Wang AWT, Chhina H, Cooper AP. Multimodal Analgesia for Paediatric Patients Undergoing Lower Limb Reconstruction with External Fixators: A Prospective Case Series of Post-operative Pain and Functional Goals. Strategies Trauma Limb Reconstr 2023;18:140-7. [PubMed]
- O'Neill A, Lirk P. Multimodal Analgesia. Anesthesiol Clin 2022;40:455-68. [Crossref] [PubMed]
- Vadivelu N, Mitra S, Schermer E, et al. Preventive analgesia for postoperative pain control: a broader concept. Local Reg Anesth 2014;7:17-22. [PubMed]
- McBride WJ, Dicker R, Abajian JC, et al. Continuous thoracic epidural infusions for postoperative analgesia after pectus deformity repair. J Pediatr Surg 1996;31:105-7; discussion 107-8. [Crossref] [PubMed]
- Futagawa K, Suwa I, Okuda T, et al. Anesthetic management for the minimally invasive Nuss procedure in 21 patients with pectus excavatum. J Anesth 2006;20:48-50. [Crossref] [PubMed]
- Weber T, Mätzl J, Rokitansky A, et al. Superior postoperative pain relief with thoracic epidural analgesia versus intravenous patient-controlled analgesia after minimally invasive pectus excavatum repair. J Thorac Cardiovasc Surg 2007;134:865-70. [Crossref] [PubMed]
- Soliman IE, Apuya JS, Fertal KM, et al. Intravenous versus epidural analgesia after surgical repair of pectus excavatum. Am J Ther 2009;16:398-403. [Crossref] [PubMed]
- Chen SY, Mack SJ, Stein JE, et al. Intercostal Nerve Cryoablation is Associated with Reduced Opioid Use in Pediatric Oncology Patients. J Surg Res 2023;283:377-84. [Crossref] [PubMed]
- Kelly RE Jr, Obermeyer RJ, Goretsky MJ, et al. Recent Modifications of the Nuss Procedure: The Pursuit of Safety During the Minimally Invasive Repair of Pectus Excavatum. Ann Surg 2022;275:e496-502. [Crossref] [PubMed]
- Nuss D, Kelly RE Jr. Indications and technique of Nuss procedure for pectus excavatum. Thorac Surg Clin 2010;20:583-97. [Crossref] [PubMed]
- Cashman JN, Dolin SJ. Respiratory and haemodynamic effects of acute postoperative pain management: evidence from published data. Br J Anaesth 2004;93:212-23. [Crossref] [PubMed]
- Meyer MJ, Krane EJ, Goldschneider KR, et al. Case report: neurological complications associated with epidural analgesia in children: a report of 4 cases of ambiguous etiologies. Anesth Analg 2012;115:1365-70. [Crossref] [PubMed]
- Giebler RM, Scherer RU, Peters J. Incidence of neurologic complications related to thoracic epidural catheterization. Anesthesiology 1997;86:55-63. [Crossref] [PubMed]
- Brull R, McCartney CJ, Chan VW, et al. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg 2007;104:965-74. [Crossref] [PubMed]
- St Peter SD, Weesner KA, Sharp RJ, et al. Is epidural anesthesia truly the best pain management strategy after minimally invasive pectus excavatum repair? J Pediatr Surg 2008;43:79-82; discussion 82. [Crossref] [PubMed]
- Bhatnagar V, Kumar R, Singh A, et al. Comparative Study Between Intravenous Patient-Controlled Analgesia Morphine and Computerized Ambulatory Delivery Device Epidural Morphine for Post Operative Analgesia for Nuss Procedure in Pectus Excavatum: A Retrospective Analysis. Cureus 2023;15:e41301. [Crossref] [PubMed]
- Chen LJ, Chen SH, Hsieh YL, et al. Continuous nerve block versus thoracic epidural analgesia for post-operative pain of pectus excavatum repair: a systematic review and meta-analysis. BMC Anesthesiol 2023;23:266. [Crossref] [PubMed]
- Hall Burton DM, Boretsky KR. A comparison of paravertebral nerve block catheters and thoracic epidural catheters for postoperative analgesia following the Nuss procedure for pectus excavatum repair. Paediatr Anaesth 2014;24:516-20. [Crossref] [PubMed]
- Loftus PD, Elder CT, Russell KW, et al. Paravertebral regional blocks decrease length of stay following surgery for pectus excavatum in children. J Pediatr Surg 2016;51:149-53. [Crossref] [PubMed]
- Beltran R, Veneziano G, Bhalla T, et al. Postoperative pain management in patients undergoing thoracoscopic repair of pectus excavatum: A retrospective analysis of opioid consumption and adverse effects in adolescents. Saudi J Anaesth 2017;11:427-31. [Crossref] [PubMed]
- Bliss DP Jr, Strandness TB, Derderian SC, et al. Ultrasound-guided erector spinae plane block versus thoracic epidural analgesia: Postoperative pain management after Nuss repair for pectus excavatum. J Pediatr Surg 2022;57:207-12. [Crossref] [PubMed]
- Santana L, Driggers J, Carvalho NF. Pain management for the Nuss procedure: comparison between erector spinae plane block, thoracic epidural, and control. World J Pediatr Surg 2022;5:e000418. [Crossref] [PubMed]
- Walter CM, Lee CS, Moore DL, et al. Retrospective study comparing outcomes of multimodal epidural and erector spinae catheter pain protocols after pectus surgery. J Pediatr Surg 2023;58:397-404. [Crossref] [PubMed]
- Kirupaharan S, Briatico D, Robinson T, et al. Postoperative management of pediatric patients undergoing minimally invasive repair of pectus excavatum: Where are we now? J Pediatr Surg 2022;57:927-31. [Crossref] [PubMed]
- Stroud AM, Tulanont DD, Coates TE, et al. Epidural analgesia versus intravenous patient-controlled analgesia following minimally invasive pectus excavatum repair: a systematic review and meta-analysis. J Pediatr Surg 2014;49:798-806. [Crossref] [PubMed]
- Nelson KM, Vincent RG, Bourke RS, et al. Intraoperative intercostal nerve freezing to prevent postthoracotomy pain. Ann Thorac Surg 1974;18:280-5. [Crossref] [PubMed]
- Kim S, Idowu O, Palmer B, et al. Use of transthoracic cryoanalgesia during the Nuss procedure. J Thorac Cardiovasc Surg 2016;151:887-8. [Crossref] [PubMed]
- Moorjani N, Zhao F, Tian Y, et al. Effects of cryoanalgesia on post-thoracotomy pain and on the structure of intercostal nerves: a human prospective randomized trial and a histological study. Eur J Cardiothorac Surg 2001;20:502-7. [Crossref] [PubMed]
- Eldredge RS, Ochoa B, Khoury E, et al. Long-Term Sensory Function 3 years after Minimally Invasive Repair of Pectus Excavatum with Cryoablation. J Pediatr Surg 2024;59:379-84. [Crossref] [PubMed]
- Keller BA, Kabagambe SK, Becker JC, et al. Intercostal nerve cryoablation versus thoracic epidural catheters for postoperative analgesia following pectus excavatum repair: Preliminary outcomes in twenty-six cryoablation patients. J Pediatr Surg 2016;51:2033-8. [Crossref] [PubMed]
- Sun RC, Mehl SC, Anbarasu CR, et al. Intercostal cryoablation during Nuss procedure: A large volume single surgeon's experience and outcomes. J Pediatr Surg 2021;56:2229-34. [Crossref] [PubMed]
- Dekonenko C, Dorman RM, Duran Y, et al. Postoperative pain control modalities for pectus excavatum repair: A prospective observational study of cryoablation compared to results of a randomized trial of epidural vs patient-controlled analgesia. J Pediatr Surg 2020;55:1444-7. [Crossref] [PubMed]
- Daemen JHT, de Loos ER, Vissers YLJ, et al. Intercostal nerve cryoablation versus thoracic epidural for postoperative analgesia following pectus excavatum repair: a systematic review and meta-analysis. Interact Cardiovasc Thorac Surg 2020;31:486-98. [Crossref] [PubMed]
- Jaroszewski DE, Bostoros P, Farina JM, et al. Evolution of Pain Control for Adult Pectus Excavatum Repair. Ann Thorac Surg 2024;117:829-37. [Crossref] [PubMed]
- DiFiore JW, Robertson JO, Chhabada S, et al. Next day discharge after the Nuss procedure using intercostal nerve cryoablation, intercostal nerve blocks, and a perioperative ERAS pain protocol. J Pediatr Surg 2022;57:213-8. [Crossref] [PubMed]
- Perez MN, Ferrantella A, Johnson KN, et al. Intercostal spinal nerve cryoablation for analgesia following pectus excavatum repair. Semin Pediatr Surg 2024;33:151382. [Crossref] [PubMed]
- Zobel MJ, Ewbank C, Mora R, et al. The incidence of neuropathic pain after intercostal cryoablation during the Nuss procedure. Pediatr Surg Int 2020;36:317-24. [Crossref] [PubMed]
- Aiken TJ, Stahl CC, Lemaster D, et al. Intercostal nerve cryoablation is associated with lower hospital cost during minimally invasive Nuss procedure for pectus excavatum. J Pediatr Surg 2021;56:1841-5. [Crossref] [PubMed]
- Toselli L, Gigena C, Bellia-Munzon G, et al. Lessons Learned after 176 Patients Treated with a Standardized Procedure of Thoracoscopic Cryoanalgesia during Minimally Invasive Repair of Pectus Excavatum. J Pediatr Surg 2024;59:372-8. [Crossref] [PubMed]
- Zacha S, Lopez M, Bilas J, et al. One- versus Two-Minute Intercostal Nerve Cryoanalgesia in Children Undergoing Surgery for Funnel Chest Deformity. J Pers Med 2024;14:875. [Crossref] [PubMed]
- McCoy N, Hollinger L. Cryoanalgesia and Lung Isolation: A New Challenge for the Nuss Procedure Made Easier With the EZ-Blocker™. Front Pediatr 2021;9:791607. [Crossref] [PubMed]
- Velayos M, Alonso M, Estefanía K, et al. Ultrasound-Guided Percutaneous Cryoanalgesia for Pectus Excavatum: When Should It be Applied? Eur J Pediatr Surg 2023;33:61-7. [Crossref] [PubMed]
- Zacha S, Jarosz K, Kokot K, et al. Benefits of the Erector Spinae Plane Block before Cryoanalgesia in Children Undergoing Surgery for Funnel Chest Deformity. J Pers Med 2023;13:1696. [Crossref] [PubMed]
- Talsma J, Kusakavitch M, Lee D, et al. Forgotten Branch of the Intercostal Nerve: Implication for Cryoablation Nerve Block for Pectus Excavatum Repair. J Pediatr Surg 2023;58:2435-40. [Crossref] [PubMed]
- Kopacz DJ, Thompson GE. Intercostal blocks for thoracic and abdominal surgery. Tech Reg Anesth Pain Manage 1998;2:25-9. [Crossref]
- Ma B, Sun Y, Hao C, et al. Patient-Controlled Intravenous Analgesia with or without Ultrasound-Guided Bilateral Intercostal Nerve Blocks in Children Undergoing the Nuss Procedure: A Randomized, Double-Blinded, Controlled Trial. Pain Res Manag 2022;2022:5776833. [Crossref] [PubMed]
- Ka ES, Rim GM, Kang S, et al. Serratus Anterior Plane Block: A Better Modality of Pain Control after Pectus Excavatum Repair. J Chest Surg 2024;57:291-9. [Crossref] [PubMed]
- He Y, Xu M, Jiang X, et al. Comparing postoperative analgesia of bilateral serratus anterior plane block and thoracic paravertebral block for children following the Nuss procedure: protocol for a randomised, double-blind, non-inferiority clinical trial. BMJ Paediatr Open 2023;7:e002128. [Crossref] [PubMed]
- Zeineddin S, Goldstein SD, Linton S, et al. Effectiveness of one minute per level intercostal nerve cryoablation for postoperative analgesia after surgical correction of pectus excavatum. J Pediatr Surg 2023;58:34-40. [Crossref] [PubMed]
- Nardiello MA, Herlitz M. Bilateral single shot erector spinae plane block for pectus excavatum and pectus carinatum surgery in 2 pediatric patients. Rev Esp Anestesiol Reanim (Engl Ed) 2018;65:530-3. [Crossref] [PubMed]
- Wu S, Wu J, Zhang X. Application of an ultrasound-guided bilateral erector spinae plane block after the Nuss procedure for pectus excavatum in children: a retrospective cohort study with propensity score matching. Front Pediatr 2023;11:1201604. [Crossref] [PubMed]
- Aranda-Valderrama P, Greenberg RS, Vecchione TM, et al. Combined erector spinae plane block with surgical intercostal nerve cryoablation for Nuss procedure is associated with decreased opioid use and length of stay. Reg Anesth Pain Med 2024;49:248-53. [Crossref] [PubMed]
- Chin KJ. Thoracic wall blocks: From paravertebral to retrolaminar to serratus to erector spinae and back again - A review of evidence. Best Pract Res Clin Anaesthesiol 2019;33:67-77. [Crossref] [PubMed]
- Marri SR. Adjuvant agents in regional anesthesia. Anesthesia Intensive Care Med 2012;13:559-62. [Crossref]
- Bhatnagar S, Mishra S, Madhurima S, et al. Clonidine as an analgesic adjuvant to continuous paravertebral bupivacaine for post-thoracotomy pain. Anaesth Intensive Care 2006;34:586-91. [Crossref] [PubMed]
- Li J, Dong Y, Guo J, et al. Thoracoscopic Intercostal Nerve Block with Cocktail Analgesics for Pain Control After Video-Assisted Thoracoscopic Surgery: A Prospective Cohort Study. J Pain Res 2024;17:1183-96. [Crossref] [PubMed]
- Cockrell HC, Hrachovec J, Schnuck J, et al. Implementation of a Cryoablation-based Pain Management Protocol for Pectus Excavatum. J Pediatr Surg 2023;58:1239-45. [Crossref] [PubMed]
- Froehling NM, Martin JA, Miles MVP, et al. Intraoperative Methadone Reduces Postoperative Opioid Requirements in Nuss Procedure for Pectus Excavatum. Am Surg 2023;89:984-9. [Crossref] [PubMed]
- Singhal NR, Jones J, Semenova J, et al. Multimodal anesthesia with the addition of methadone is superior to epidural analgesia: A retrospective comparison of intraoperative anesthetic techniques and pain management for 124 pediatric patients undergoing the Nuss procedure. J Pediatr Surg 2016;51:612-6. [Crossref] [PubMed]
- Sadhasivam S, Aruldhas BW, Packiasabapathy S, et al. A Novel Perioperative Multidose Methadone-Based Multimodal Analgesic Strategy in Children Achieved Safe and Low Analgesic Blood Methadone Levels Enabling Opioid-Sparing Sustained Analgesia With Minimal Adverse Effects. Anesth Analg 2021;133:327-37. [Crossref] [PubMed]
- Jin Z, Lin EJ, He Y, et al. Intraoperative methadone for postoperative pain management - systematic review protocol. Int J Physiol Pathophysiol Pharmacol 2019;11:220-3. [PubMed]
- Goldblatt J, Crawford L, Ross J, et al. The influence of preoperative or intraoperative methadone on postcardiac surgery pain and opioid administration: a systematic review and meta-analysis. Cardiothorac Surg 2024;32:8. [Crossref]
- Litz CN, Farach SM, Fernandez AM, et al. Enhancing recovery after minimally invasive repair of pectus excavatum. Pediatr Surg Int 2017;33:1123-9. [Crossref] [PubMed]
- Holmes DM, Polites SF, Roskos PL, et al. Opioid use and length of stay following minimally invasive pectus excavatum repair in 436 patients - Benefits of an enhanced recovery pathway. J Pediatr Surg 2019;54:1976-83. [Crossref] [PubMed]
- Wharton K, Chidiac C, Lopez C, et al. Enhanced Recovery After Surgery 2.0: Optimizing Pain Management in Nuss Procedure: Cryoablation and Nerve Block Strategies for Reduced Opioid Use. J Surg Res 2024;301:563-71. [Crossref] [PubMed]
- Mangat S, Hance L, Ricketts KJ, et al. The impact of an enhanced recovery perioperative pathway for pediatric pectus deformity repair. Pediatr Surg Int 2020;36:1035-45. [Crossref] [PubMed]
- Rettig RL, Rudikoff AG, Lo HYA, et al. Same day discharge for pectus excavatum-is it possible? J Pediatr Surg 2022;57:34-8. [Crossref] [PubMed]
- Rettig RL, Rudikoff AG, Annie Lo HY, et al. Same-day discharge following the Nuss repair: A comparison. J Pediatr Surg 2022;57:135-40. [Crossref] [PubMed]
- Akinboro S, John R, Reyna T, et al. A pilot study of multi-modal pain management for same-day discharge after minimally invasive repair of pectus excavatum (Nuss procedure) in children. Pediatr Surg Int 2023;39:159. [Crossref] [PubMed]


