
Exploring the association between pulmonary function and air pollution exposure in healthy children in Jinan, Shandong Province: based on a cross-sectional study
Highlight box
Key findings
• On the third day of exposure to air pollutants (lag 3 d), healthy children showed a decrease in lung function indices [forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), peak expiratory flow (PEF), forced expiratory flow at 25% (FEF25) and forced expiratory flow at 75% (FEF75)], which was also shown by the results of the multi-pollutant modeling.
What is known and what is new?
• Previous studies have linked air pollutant exposure to decreased lung function in children, but there has been limited research on this relationship among healthy children. These studies typically focused on a narrow range of lung function indicators, such as FVC, FEV1, and PEF, and primarily utilized single pollutant models.
• This study lies in its demonstration that short-term exposure to air pollutants not only affects FVC, FEV1, and PEF but also impacts FEF75 and FEF25 in healthy children. Additionally, a joint effect of multiple pollutants on lung function was observed.
What is the implication, and what should change now?
• This study raises alarm bells about the threat of air pollution to lung development in healthy schoolchildren. It could inform the development of preventive measures.
Introduction
Air pollutants pose a serious threat to human health. Among them, particulate matter with an aerodynamic diameter ≤2.5 µm (PM2.5) is of particular concern because it can penetrate deeper into the human respiratory tract and alveoli, and even further into the bloodstream, seriously damaging the respiratory system (1). Particulate matter with an aerodynamic diameter ≤10 µm (PM10) can also enter the respiratory tract below the larynx, posing a potential hazard to human health (2). Long-term exposure to these air pollutants, especially PM10, has been shown to be strongly associated with decreased lung function in non-asthmatic schoolchildren (3,4). Notably, even short-term exposure to high concentrations of nitrogen dioxide (NO2) is directly associated with acute decrease in lung function and is strongly linked to a significantly elevated risk of pneumonia in children (5,6).
Children are more sensitive to air pollutants as their immune and respiratory systems are not fully developed; they are also likely to inhale more air pollutants than adults during physical exercise (7-9). Due to the lower height of children, they are closer to the ground and are therefore more likely to inhale air containing higher concentrations of pollutants (10). Lung function is an important objective indicator of the health of the human respiratory system. Some studies have shown (11-13) that short-term exposure to air pollutants is associated with decreased lung function in children. Therefore, an in-depth investigation of the relationship between pollutants and children’s lung function may help to improve our understanding of the threats of air pollution to children’s respiratory health, which may provide a basis for the development of effective measures to protect children’s respiratory health.
Although prior studies have demonstrated an association between elevated pollutant concentrations over short periods of time and decreased lung function in children, these studies focused on children with medical conditions (14-16), which limits the applicability of the findings to the healthy children. And these studies also focused on a single indicator or a limited number of indicators of lung function, such as forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1) and peak expiratory flow (PEF) (17-19), whereas in reality lung function tests cover a much wider range of indicators, for example, also including forced expiratory flow at 25% (FEF25) and forced expiratory flow at 75% (FEF75). In addition, most studies have focused primarily on the effects of a single pollutant (20-22), with only a few studies focusing on the joint effects of multiple pollutants (23).
In view of this, we sought to explore the short-term and lagged effects of air pollutants on healthy children using five key lung function indices (FVC, PEF, FEV1, FEF25 and FEF75), and in addition to constructing a multi-pollutant model to investigate the joint effects of pollutants in order to gain a more comprehensive understanding of their potential impact on children’s health. We hope that this study will provide practical significance and scientific basis for the formulation of more effective policies to protect children’s respiratory health. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-24-438/rc).
Methods
Study area
The present study was based in Jinan City, one of the most heavily air-polluted cities in China. Jinan is an inland city in northern China and the capital of Shandong Province; it covers a total of 8,177.21 km2 and is divided into ten districts. It is located at 36.40°N latitude and 110.00°E longitude. As a northern inland city, the low temperatures in winter make it difficult for pollutants to disperse, and the burning of coal and other fossil fuels may also add to the air pollution (23). This city is also one of the important transportation hubs in east China, with its primary energy source dominated by coal. The climate there is a mid-latitude monsoon climate.
Study design and participants
This study was a longitudinal cross-sectional study. In this study, stratified random sampling was used to stratify the school’s students in grades 3 through 5 by grade level, with each grade level serving as a separate stratum. In December of each year between 2016 and 2020, one class from each grade level stratum was randomly selected for testing. This random sampling strategy ensured that each class in each grade level had the same probability of being selected, effectively reducing the impact of selection bias on the study results. Before performing the lung function tests, we first interviewed the parents of the students to rule out any children with underlying respiratory conditions. Second, we measured the body indices, including height (cm) and weight (kg), of all study participants who participated in the test, and recorded their sex and date of birth in detail. Finally, a professional technician verifies basic information about each subject and performs brief health screenings on all participating children to ensure that they do not have respiratory illnesses or symptoms on the day of the test. These screenings include asking children if they have symptoms such as fever, cough or shortness of breath, and if they have recently sought medical attention.
To ensure the reliability of the findings and the quality of the survey, the main content and precautions of the survey were explained to students, their guardians and school leaders before the survey was conducted, and parents were assured that the information they provided would be kept strictly confidential and would not be used for any other purposes. The survey was entirely voluntary and informed consent was obtained from all participants and their primary guardians. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shandong Second Medical University (No. 2021SDL188) and informed consent was taken from all the participants’ guardians.
Measurement of pulmonary function
All pulmonary function tests are performed by trained technicians in accordance with the 2005 Pulmonary Function Test Standards published by the American Thoracic Society (ATS) and the European Respiratory Society (ERS) (24). The spirometer was calibrated before the test. During the test, the child stood, wore a nose clip, and blew at least three times into a portable spirometer (Pony FX, Italy) with a disposable mouthpiece. If the difference between the two highest FVC and FEV1 values was less than 150 mL (or within 5%) and the difference between the maximum and minimum PEF values was less than 0.67 L/s, the reproducibility of the test result was acceptable. For those children whose pulmonary function results did not meet this criterion, up to eight breath tests were required. Pulmonary function indices include FVC, FEV1, PEF, FEF75, FEF25.
Air pollution exposure
Air quality data for Jinan during the study period were obtained from the National Urban Air Quality Real-time Distribution Platform operated by the China Environmental Monitoring Centre (https://www.cnemc.cn). The platform ensured that the data were updated daily and the nearest national control station to the study site was selected to obtain 24-hour air pollutant averages. Air pollutants include PM2.5, PM10, SO2, NO2, CO and O3-8h. Concurrent weather data, including average temperature (Temp, ℃) and relative humidity (RH, %), were sourced from the Jinan Meteorological Bureau’s official website (http://jnqx.jinan.gov.cn).
Statistical analysis
Descriptive analysis was conducted for air quality indicators, weather conditions, subject characteristics, and pulmonary function indicators. Chi-squared tests were used for sex and age distributions. Spearman’s correlation analysis assessed the relationships between pollutant concentrations, lung function indicators, and meteorological factors (temperature and humidity). Body mass index (BMI) was calculated as weight divided by height squared. Multiple linear regression models were established to evaluate the impact of elevated air pollutant concentrations on lung function, adjusting for age, sex, height, weight, temperature, and humidity. Separate subgroup analyses were also performed for male and female students. Stepwise regression was used to select the optimal model based on the lowest Akaike Information Criterion (AIC) value. The results were presented as changes in pulmonary function indicators per 10 µg/m3 increase in the concentration of different air pollutants and the corresponding 95% confidence interval (95% CI).
To explore whether there was a lagged effect of different air pollutants on the pulmonary function of children, we analyzed the lagged effect of each pollutant independently in the model at a single lag (lag0–lag5) and cumulative lags (lag05), with lag0 referring to the pollutant concentration on the day of the pulmonary function test, Lag1 referring to the pollutant concentration on the day before the pulmonary function test and so on; Lag05 referring to the cumulative mean on the day of the pulmonary function test and the previous 5 days.
We constructed a multi-pollutant model to analyze the joint effects of multiple pollutants on lung function by selecting the pollutant with statistically significant differences (NO2) as the main model in the single-pollutant model, and then adding the other pollutants (PM2.5, SO2, and O3-8 h) to NO2, respectively. Since the correlation coefficients between NO2 and PM10 and between NO2 and CO were very high, which may indicate a multicollinearity problem. Therefore, we only included PM2.5, SO2 and O3 in the multi-pollutant model for data analysis.
Data analysis was performed using the R software (version 4.2.3). We used the “dplyr” data processing package in R to calculate the lagged effects of pollutant exposure and further derived the cumulative lagged effects by accumulating multiple lagged values. All the tests were two-tailed, and a P value of less than 0.05 was indicative of statistical significance.
Results
General information
In this study, a total of 791 children participated in the initial survey. After screening, children with respiratory diseases such as asthma, pneumonia, bronchitis or colds, and those who were unable to attend school for the test due to leave of absence, totaling 11, were excluded. Eventually, a total of 780 children were included in the study and underwent pulmonary function tests, including 412 boys and 368 girls. There were no significant differences in gender (χ2=5.449, P>0.05) and age (χ2=0.580, P>0.05) across test years (Table 1).
Table 1
| Variable | Male | Female | Total | χ2 | P value |
|---|---|---|---|---|---|
| Year | 5.449 | >0.05 | |||
| 2016 | 85 (48.30) | 91 (51.70) | 176 | ||
| 2017 | 82 (51.25) | 78 (48.75) | 160 | ||
| 2018 | 90 (56.60) | 69 (43.40) | 159 | ||
| 2019 | 83 (59.29) | 57 (40.71) | 140 | ||
| 2020 | 72 (49.66) | 73 (50.34) | 145 | ||
| Age (years) | 0.580 | >0.05 | |||
| 7–9 | 222 (53.75) | 191 (46.25) | 413 | ||
| 10–11 | 190 (51.77) | 177 (48.23) | 367 |
Data are presented as n (%).
The general characteristics and pulmonary function indicators of the subjects and meteorological factors are shown in Table 2. The mean height of the 780 children was 141.52 cm, the mean height was 38.94 kg, and the mean BMI was 19.13 kg/m2. The mean FVC was 2.03 L [standard deviation (SD) =0.44], the mean FEV1 was 1.73 L (SD =0.38), and the mean PEF was 2.95 L/s (SD =0.93). According to the Ambient Air Quality Standards GB 3095-2012, the PM2.5 concentration exceeded the secondary standard limits during the survey, with a mean PM2.5 concentration of 88.83 µg/m3 (SD =51.08) (Table 2).
Table 2
| Variable | Mean ± SD | Percentile | ||||
|---|---|---|---|---|---|---|
| Min | Max | 25th | 50th | 75th | ||
| Characteristics | ||||||
| Height (cm) | 141.52±8.79 | 120 | 177 | 135 | 140 | 147 |
| Weight (kg) | 38.94±11.79 | 18.40 | 85.20 | 30 | 36.60 | 45.58 |
| BMI (kg/m2) | 19.13±4.15 | 12.16 | 33.59 | 15.90 | 18.27 | 21.88 |
| Lung function parameters | ||||||
| FVC (L) | 2.03±0.44 | 1.00 | 4.02 | 1.73 | 1.98 | 2.27 |
| FEV1 (L) | 1.73±0.38 | 0.63 | 3.36 | 1.47 | 1.69 | 1.97 |
| PEF (L/s) | 2.95±0.93 | 0.67 | 5.78 | 2.28 | 2.89 | 3.54 |
| FEF75 (L/s) | 1.19±0.36 | 0.27 | 2.80 | 0.92 | 1.16 | 1.40 |
| FEF25 (L/s) | 2.78±0.90 | 0.65 | 5.75 | 2.17 | 2.73 | 3.38 |
| Air pollutants | ||||||
| PM2.5 (µg/m3) | 88.83±51.08 | 18.87 | 256.17 | 48.98 | 81.45 | 119.33 |
| PM10 (µg/m3) | 147.58±63.23 | 49.30 | 335.74 | 100.58 | 138.69 | 184.13 |
| SO2 (µg/m3) | 28.11±15.72 | 7.09 | 78.48 | 16.65 | 23.13 | 36.89 |
| NO2 (µg/m3) | 59.98±18.31 | 13.33 | 112.52 | 47.16 | 60.67 | 70.60 |
| CO (mg /m3) | 1.40±0.52 | 0.47 | 2.99 | 1.03 | 1.32 | 1.78 |
| O3 (µg/m3) | 27.50±17.37 | 4.46 | 95.05 | 16.93 | 22.63 | 35.77 |
| Weather conditions | ||||||
| Temp/℃ | 3.03±4.06 | −6.8 | 18 | −0.6 | 4.3 | 5.85 |
| RH/% | 47.35±22.55 | 11.1 | 91 | 27 | 42.50 | 69 |
BMI, body mass index; CO, carbon monoxide; FEF25, forced expiratory flow at 25%; FEF75, forced expiratory flow at 75%; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; NO2, nitrogen dioxide; O3, ozone; PEF, peak expiratory flow; PM2.5, particulate matter with an aerodynamic diameter ≤2.5 μm; PM10, particulate matter with an aerodynamic diameter ≤10 μm; RH, relative humidity; SD, standard deviation; SO2, sulphur dioxide; Temp, temperature.
Correlation analysis
All the pollutants were found to be positively correlated with Temp, with NO2 showing the greatest correlation with Temp (ρ=0.444, P<0.01) and O3 showing the minimum correlation with Temp (ρ=0.250, P<0.01) (Table 3). All pollutants except O3 were positively correlated with RH, with PM2.5 having the greatest correlation with RH (ρ=0.642, P<0.01).
Table 3
| Variable | PM2.5 | PM10 | SO2 | NO2 | CO | O3 | Temp | RH |
|---|---|---|---|---|---|---|---|---|
| PM2.5 | 1.000 | |||||||
| PM10 | 0.907** | 1.000 | ||||||
| SO2 | 0.438** | 0.561** | 1.000 | |||||
| NO2 | 0.684** | 0.802** | 0.697** | 1.000 | ||||
| CO | 0.888** | 0.845* | 0.498** | 0.773* | 1.000 | |||
| O3 | −0.231* | −0.265** | −0.063 | −0.429** | −0.350** | 1.000 | ||
| Temp | 0.402** | 0.435* | 0.341** | 0.444* | 0.400** | 0.250** | 1.000 | |
| RH | 0.642** | 0.521* | 0.123 | 0.326** | 0.550** | −0.331** | 0.159 | 1.000 |
*, significant correlation at the level of α=0.05; **, significant correlation at the level of α=0.01. CO, carbon monoxide; NO2, nitrogen dioxide; O3, ozone; PM2.5, particulate matter with an aerodynamic diameter ≤2.5 μm; PM10, particulate matter with an aerodynamic diameter
≤10 μm; RH, relative humidity; SO2, sulphur dioxide; Temp, temperature.
The associations between air pollution exposure and pulmonary function parameters are presented in Table S1. Correlation analyses showed that air pollutants were negatively correlated with lung function indices on the day of exposure (lag0), on the third day of lag (lag3), and cumulative lag exposure up to 5 days (lag05).
Association between pollutant exposure and lung function
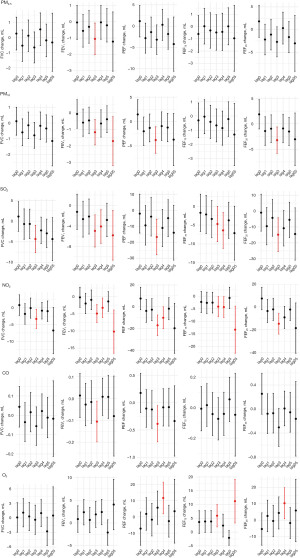
Single-pollutant model
The single-pollutant model showed varying degrees of lagged and cumulative lagged effects of air pollutants on children’s lung function, with significant decreases in lung function FEV1 and PEF (Figure 1, Table S2). At lag3, FEV1 decreased by 1.05 mL (95% CI: −2.02, −0.08), 1.18 mL (95% CI: −1.94, −0.42), 4.96 mL (95% CI: −8.08, −1.84), 4.94 mL (95% CI: −7.59, −2.28) and 0.11 mL (95% CI: −0.20, −0.01) for every 10 µg/m3 increase for PM2.5 , PM10, SO2 , NO2 , and CO, respectively; for every 10 µg/m3 increase in PM10, SO2, NO2, and CO, PEF decreased by 3.80 mL (95% CI: −6.51, −1.08), 16.73 mL (95% CI: −27.83, −5.63), 17 mL (95% CI: −26.44, −7.55), and 0.39 mL (95% CI: −0.72, −0.05), respectively. Furthermore, all five lung function indices were significantly decreased in children when exposed to SO2 and NO2 (P<0.05).
Multi-pollutant model
Table 4 shows the results of the multi-pollutant models. According to the principle of statistically significance in the single-pollutant model, the optimal effect day of lung function indices FVC, FEV1, PEF, FEF75, and FEF25 was determined to be lag3.
Table 4
| Pollutant model | FVC (mL) | FEV1 (mL) | PEF (mL) | FEF75 (mL) | FEF25 (mL) |
|---|---|---|---|---|---|
| Dual-pollutant model | |||||
| NO2 | −3.32 (−6.21, −0.44)* | −4.94 (−7.59, −2.28)*** | −17.00 (−26.44, −7.55)*** | −4.18 (−8.22, −0.14)* | −14.75 (−23.84, −5.65)** |
| +PM2.5 | −3.95 (−7.99, 0.10)* | −5.55 (−9.27, −1.82)** | −20.85 (−34.06, −7.64)** | −6.27 (−11.91, −0.63)* | −18.27 (−30.99, −5.55)** |
| +SO2 | −1.38 (−5.41, 2.64) | −3.78 (−7.51, −0.06)* | −13.45 (−26.72, −0.18)* | −2.59 (−8.26, 3.09) | −11.25 (−24.03, 1.52) |
| +O3 | −4.48 (−7.73, −1.23)** | −5.21 (−8.24, −2.18)*** | −18.35 (−29.08, −7.61)** | −1.89 (−6.39, 2.61) | −16.20 (−26.54, −5.85)** |
| Multi-pollutant model | |||||
| NO2 + PM2.5 | −3.95 (−7.99, 0.10)* | −5.55 (−9.27, −1.82)** | −20.85 (−34.06, −7.64)** | −6.27 (−11.91, −0.63)* | −18.27 (−30.99, −5.55)** |
| +SO2 | −1.76 (−6.98, 3.46) | −4.30 (−9.13, 0.53) | −17.37 (−34.54, −0.21)* | −4.77 (−12.10, 2.55) | −14.79 (−31.32, 1.74) |
| +O3 | −5.23 (−9.59, −0.87)* | −5.88 (−9.94, −1.82)** | −22.38 (−36.74, −8.03)** | −3.85 (−9.86, 2.17) | −19.91 (−33.75, −6.07)** |
Data are presented as β (95% CI). *, significant correlation at the level of α=0.05; **, significant correlation at the level of α=0.01; ***, significant correlation at the level of α=0.001. These estimates are from dual and multi-pollutant regression models, with adjustments for age, sex, height, weight, average temperature and relative humidity. CI, confidence interval; FEF25, forced expiratory flow at 25%; FEF75, forced expiratory flow at 75%; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; NO2, nitrogen dioxide; O3, ozone; PEF, peak expiratory flow; PM2.5, particulate matter with an aerodynamic diameter ≤2.5 μm; SO2, sulphur dioxide.
The dual-pollutant model showed a significant (P<0.05) decrease in FEV1 and PEF when NO2 was jointed with PM2.5, SO2 and O3. The multi-pollutant model showed a significant (P<0.05) decrease in PEF when particulate matter was combined with gaseous pollutants (Table 4).
After correction of the P value by the Bonferroni test (Table S3), both the two-pollutant model and the multi-pollutant model showed that the children’s lung function indices still showed significant decreases of varying magnitude (P<0.05) when irritant gases were jointed with particulate matter.
Gender analysis
The results showed (Table 5) that pollutants had inconsistent effects on lung function in boys and girls, with boys showing a significant decrease in the lung function index FVC compared to girls (P<0.05). For every 10 µg/m3 increase in SO2 and NO2, the boys’ FVC decreased by 8.05 and 5.63 mL, respectively.
Table 5
| Pulmonary function | Air pollutants | Male | Female |
|---|---|---|---|
| FVC (mL) | PM2.5 | 1.15 (−1.04, 3.34) | 0.03 (−1.11, 1.17) |
| SO2 | 8.05 (1.33, 14.76)* | −0.51 (−4.50, 3.49) | |
| NO2 | 5.63 (0.18, 11.08)* | −0.65 (−4.09, 2.80) | |
| FEV1 (mL) | PM2.5 | 0.64 (−1.37, 2.64) | −0.21 (−1.40, 0.97) |
| SO2 | −0.06 (−6.51, 6.38) | −0.54 (−4.70, 3.61) | |
| NO2 | 1.87 (−3.26, 6.99) | −0.43 (−4.02, 3.15) | |
| PEF (mL) | PM2.5 | 4.40 (−2.77, 11.58) | −0.24 (−4.50, 4.02) |
| SO2 | −0.37 (−23.69, 22.94) | −3.43 (−18.31, 11.45) | |
| NO2 | 14.84 (−3.33, 33.01) | 3.93 (−8.90, 16.75) | |
| FEF75 (mL) | PM2.5 | −1.47 (−4.26, 1.31) | −0.13 (−1.98, 1.72) |
| SO2 | −7.76 (−16.49, 0.97) | 1.91 (−4.54, 8.36) | |
| NO2 | −6.08 (−13.07, 0.92) | 0.17 (−5.42, 5.75) | |
| FEF25 (mL) | PM2.5 | 4.53 (−2.38, 11.44) | 0.73 (−3.28, 4.75) |
| SO2 | −3.00 (−25.48, 19.47) | 0.94 (−13.13, 15.02) | |
| NO2 | 11.63 (−6.06, 29.32) | 6.05 (−5.98, 18.08) |
Data are presented as β (95% CI). *, significant correlation at the level of α=0.05. The multiple linear regression models were adjusted for age, weight, height, sex, relative humidity, and average temperature. CI, confidence interval; FEF25, forced expiratory flow at 25%; FEF75, forced expiratory flow at 75%; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; NO2, nitrogen dioxide; O3, ozone; PEF, peak expiratory flow; PM2.5, particulate matter with an aerodynamic diameter ≤2.5 μm; SO2, sulphur dioxide.
Discussion
This study explored the relationship between short-term exposure to air pollutants and children’s lung function by measuring lung function in healthy children. The results of the study showed that children’s lung function decreased after short-term exposure to pollutants. Further studies found that the effects were not limited to the moment of exposure, but that there was a significant lag effect and a cumulative lag effect. In particular, the pulmonary function index showed a significant decrease on the lag 3 d. In order to gain a more comprehensive understanding of the effects of different pollutants on children’s lung function, we used a multi-pollutant model for our analysis. The results showed a significant decrease in FEV1 and PEF when NO2 was combined with PM2.5, SO2 and O3. In addition, the study conducted a stratified analysis to explore changes in lung function in children of different genders in response to pollutant exposure. It was found that boys’ lung function was more sensitive to pollutant exposure.
Our results showed a statistically significant association between increasing pollutant concentrations and decreasing lung function indices in children, indicating that short-term exposure to air pollutants decreases lung function in healthy children. This finding is consistent with previous studies (25-27), all of which confirm the potential adverse effects of air pollutants on lung function in children. More importantly, we also observed a lagged and cumulative lagged effect of pollutants on lung function, a result supported by previous studies (7,14,28), confirming the persistence of the health risks posed by pollutants on children’s lung function.
Compared with previous studies, we were more comprehensive in the selection of study indicators. While previous studies focused on the core indices of FVC, FEV1, and PEF, our study included important indices such as FEF25 and FEF75 in addition to FVC, FEV1, and PEF. For example, a study of 315 schoolchildren aged 9 to 16 years in Bangladesh revealed that PEF and FEV1 showed a decrease of −4.19% and −2.05%, respectively, for every 20 µg/m3 increase in PM2.5 concentration (29). Another panel study of 86 children in China similarly showed that for every 10 µg/m3 increase in the 1-day moving average concentration of PM2.5, the values of FVC, FEV1, and PEF decreased by 23.22 mL, 18.93 mL, and 29.38 mL/s, respectively (30). In addition, a Japanese study also found a significant −3.67 L/min decrease in PEF for every 13.6 ppb increase in O3 exposure over the interquartile range (31). The comparison of these findings further highlights the comprehensiveness of our study in terms of indicator selection. And in clinical practice (32,33), FVC is often used to assess the function of the large airway, FEV1 is used to reflect the obstruction of large and small airways, and PEF is used to reveal airway obstruction and respiratory muscle strength. FEF25 and FEF75 are often regarded as proxies for peripheral small airway function. In this study, we found that all lung function indices of children decreased as the concentration of air pollutants increased; thus, it is evident that exposure to air pollutants not only affects children’s large airway function, but also has a significant negative effect on their small airway function. This finding further emphasizes the importance of good air quality in maintaining respiratory health.
The association between exposure to pollutants and decreased lung function observed in this study may be due to multiple mechanisms. It has been suggested that oxidative stress and inflammatory responses are the core mechanisms by which air pollutants adversely affect human health (34,35). Specifically, PM2.5, due to its extremely small particle size, easily penetrates the alveoli and activates an inflammatory response (36), and even low levels of PM2.5 may trigger airway inflammation (15), which can ultimately lead to a decreases in lung function. On the other hand, SO2 exposure should not be ignored. Studies have shown that SO2 can increase the expression levels of certain genes involved in inflammatory pathways, which in turn triggers oxidative damage in the lungs (37). In addition, air pollutants such as NO2 have been shown to induce the production of reactive oxygen species (ROS), which further contributes to tissue inflammation and cell death, resulting in potential damage to lung function (38).
It is worth mentioning that the present study also revealed the existence of a lagged effect of O3 on lung function, in particular the persistent correlation with FEF75. The low water solubility of O3, a pollutant with significant acute health effects, makes it more likely to be retained in the small airways (39); this is in line with our study, where O3 was associated with a decrease in FEF75, which represents the function of small air-ways. However, the effects of O3 on children’s pulmonary function are not significant compared to other pollutants, which might be related to the lower temperature in winter, at which the concentration of O3 is usually lower. An analysis of air pollution control measures and their co-benefits in Jinan showed a significant increasing trend in ozone concentrations in the city since 2013 (40), which further highlights the importance of continuous monitoring and assessment of the public health impacts of air pollution. This reminds us of the need to comprehensively consider the characteristics of different pollutants and their health impacts when formulating air quality improvement measures.
In our multi-pollutant model, the correlation coefficients between NO2 and PM10 and between NO2 and CO are very high, suggesting the problem of multicollinearity. Therefore, we included only PM2.5, SO2 and O3 in our multi-pollutant model. The modeling results showed that NO2 was associated with a decrease in lung function indices (P<0.05), especially PEF, which is consistent with the results of a national cohort study (41). These results strongly suggest that traffic-related air pollution, represented by NO2, has a significant impact on children’s respiratory health.
The specific mechanisms by which sex differences play a role in the response to air pollutants are currently unknown. Although existing studies have given increasing attention to this issue, the conclusions are not consistent. Notably, our study reveals that boys’ lung function is more sensitive to air pollutants compared to girls’, which is consistent with previous studies (42,43). However, there are also studies with opposite findings (9,44,45). These differences may stem from differences in methodology, measurement techniques, and age distribution of subjects across studies, while the types of air pollutants studied may also have an impact on the results. Therefore, to fully understand the role of gender in the response to air pollutants, future research needs to integrate these factors and use more standardized research methods.
Despite the insights of this study, there are some limitations. First, because air pollutant data are derived from existing and fixed monitoring stations, their measurements may deviate from the actual exposure of individuals, and this indirect assessment of exposure may lead to misclassification. Second, the study failed to adequately consider and adjust for some important confounding factors, such as home environment, parental smoking habits, and socioeconomic status, which may have an impact on children’s lung function, and therefore future studies could incorporate home environment questionnaires to collect data on household pollutants (e.g., indoor smoking, cooking practices, heating equipment, etc.) to more comprehensively assess the actual exposure of children’s levels. Third, since the pulmonary function tests in this study were performed specifically in December of each year, this temporal limitation makes the significance and generalizability of the findings somewhat limited. However, even with these limitations, the present study revealed a strong association between short-term exposure to different air pollutants and acute impairment of lung function in children and pointed out the lagged and cumulative lagged effects of air pollutants.
Conclusions
Overall, the present study reveals a significant negative association between some atmospheric pollutants and lung function in healthy children, especially those closely related to transportation, such as NO2 and SO2. Therefore, to effectively safeguard the respiratory health of children and adolescents, we need to adopt a series of targeted public health measures.
Acknowledgments
The authors are grateful to the Center for Disease Control and Prevention of Licheng District for sharing the information needed for this study.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-24-438/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-24-438/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-24-438/prf
Funding: This study was funded by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-24-438/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shandong Second Medical University (No. 2021SDL188) and informed consent was taken from all the participants’ guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yang L, Li C, Tang X. The Impact of PM on the Host Defense of Respiratory System. Front Cell Dev Biol 2020;8:91. [Crossref] [PubMed]
- Wu IP, Liao SL, Lai SH, et al. The respiratory impacts of air pollution in children: Global and domestic (Taiwan) situation. Biomed J 2022;45:88-94. [Crossref] [PubMed]
- Tsui HC, Chen CH, Wu YH, et al. Lifetime exposure to particulate air pollutants is negatively associated with lung function in non-asthmatic children. Environ Pollut 2018;236:953-61. [Crossref] [PubMed]
- Mahapatra B, Walia M, Avis WR, et al. Effect of exposure to PM(10) on child health: evidence based on a large-scale survey from 184 cities in India. BMJ Glob Health 2020;5:e002597. [Crossref] [PubMed]
- Gaffin JM, Hauptman M, Petty CR, et al. Nitrogen dioxide exposure in school classrooms of inner-city children with asthma. J Allergy Clin Immunol 2018;141:2249-2255.e2. [Crossref] [PubMed]
- Zhou X, Guo M, Li Z, et al. Associations between air pollutant and pneumonia and asthma requiring hospitalization among children aged under 5 years in Ningbo, 2015-2017. Front Public Health 2022;10:1017105. [Crossref] [PubMed]
- Zhang J, Wang Y, Feng L, et al. Effects of air pollution and green spaces on impaired lung function in children: a case-control study. Environ Sci Pollut Res Int 2022;29:11907-19. [Crossref] [PubMed]
- Brumberg HL, Karr CJ. COUNCIL ON ENVIRONMENTAL HEALTH. Ambient Air Pollution: Health Hazards to Children. Pediatrics 2021;147:e2021051484. [Crossref] [PubMed]
- Teng J, Li J, Yang T, et al. Long-term exposure to air pollution and lung function among children in China: Association and effect modification. Front Public Health 2022;10:988242. [Crossref] [PubMed]
- United Nations Children’s Fund. Childhood Air Pollution Exposure Key Messages. New York, NY: United Nations Children’s Fund; 2022.
- Jung KH, Torrone D, Lovinsky-Desir S, et al. Short-term exposure to PM(2.5) and vanadium and changes in asthma gene DNA methylation and lung function decrements among urban children. Respir Res 2017;18:63. [Crossref] [PubMed]
- Khatri SB, Newman C, Hammel JP, et al. Associations of Air Pollution and Pediatric Asthma in Cleveland, Ohio. ScientificWorldJournal 2021;2021:8881390. [Crossref] [PubMed]
- Ji N, Baptista A, Yu CH, et al. Traffic-related air pollution, chronic stress, and changes in exhaled nitric oxide and lung function among a panel of children with asthma living in an underresourced community. Sci Total Environ 2024;912:168984. [Crossref] [PubMed]
- Zhou J, Lei R, Xu J, et al. The Effects of Short-Term PM2.5 Exposure on Pulmonary Function among Children with Asthma-A Panel Study in Shanghai, China. Int J Environ Res Public Health 2022;19:11385. [Crossref] [PubMed]
- Kim Y, Park EH, Ng CFS, et al. Respiratory function declines in children with asthma associated with chemical species of fine particulate matter (PM2.5) in Nagasaki, Japan. Environ Health 2021;20:110. [Crossref] [PubMed]
- Newcomb P, Hunt A, Rast P, et al. Acute effects of walking environment and GSTM1 variants in children with asthma. Biol Res Nurs 2012;14:55-64. [Crossref] [PubMed]
- Xu D, Chen Y, Wu L, et al. Acute effects of ambient PM(2.5) on lung function among schoolchildren. Sci Rep 2020;10:4061. [Crossref] [PubMed]
- Yu Z, Merid SK, Bellander T, et al. Associations of improved air quality with lung function growth from childhood to adulthood: the BAMSE study. Eur Respir J 2023;61:2201783. [Crossref] [PubMed]
- Tasmin S, Ng CFS, Stickley A, et al. Acute effects of ambient temperature on lung function of a panel of school children living in Dhaka, Bangladesh. Sci Total Environ 2022;838:156139. [Crossref] [PubMed]
- Garcia E, Rice MB, Gold DR. Air pollution and lung function in children. J Allergy Clin Immunol 2021;148:1-14. [Crossref] [PubMed]
- Watkins WJ, Course CW, Cousins M, et al. Impact of ambient air pollution on lung function in preterm-born school-aged children. Thorax 2024;79:553-63. [Crossref] [PubMed]
- Suhaimi NF, Jalaludin J, Mohd Juhari MA. The impact of traffic-related air pollution on lung function status and respiratory symptoms among children in Klang Valley, Malaysia. Int J Environ Health Res 2022;32:535-46. [Crossref] [PubMed]
- Hsu HL, Wilson A, Schwartz J, et al. Prenatal Ambient Air Pollutant Mixture Exposure and Early School-age Lung Function. Environ Epidemiol 2023;7:e249. [Crossref] [PubMed]
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005;26:319-38. [Crossref] [PubMed]
- Cao S, Li S, Duan X, et al. Environmental and Behavioral Factors in Association with Lung Function Impairment in Children Living in Wuhan, China. Int J Environ Res Public Health 2023;20:1134. [Crossref] [PubMed]
- Amazouz H, Bougas N, Thibaudon M, et al. Association between lung function of school age children and short-term exposure to air pollution and pollen: the PARIS cohort. Thorax 2021;76:887-94. [Crossref] [PubMed]
- Cibella F, Cuttitta G, Della Maggiore R, et al. Effect of indoor nitrogen dioxide on lung function in urban environment. Environ Res 2015;138:8-16. [Crossref] [PubMed]
- Huang ZH, Liu XY, Zhao T, et al. Short-term effects of air pollution on respiratory diseases among young children in Wuhan city, China. World J Pediatr 2022;18:333-42. [Crossref] [PubMed]
- Tasmin S, Ng CFS, Stickley A, et al. Effects of Short-term Exposure to Ambient Particulate Matter on the Lung Function of School Children in Dhaka, Bangladesh. Epidemiology 2019;30:S15-23. [Crossref] [PubMed]
- Xu D, Zhang Y, Zhou L, et al. Acute effects of PM(2.5) on lung function parameters in schoolchildren in Nanjing, China: a panel study. Environ Sci Pollut Res Int 2018;25:14989-95. [Crossref] [PubMed]
- Kurai J, Noma H, Sano H, et al. Association of short-term ozone exposure with pulmonary function and respiratory symptoms in schoolchildren:A panel study in a western Japanese city. J Med Invest 2018;65:236-41. [Crossref] [PubMed]
- Ye T, Guo Y, Abramson MJ, et al. Greenspace and children's lung function in China: A cross-sectional study between 2013 and 2015. Sci Total Environ 2023;858:159952. [Crossref] [PubMed]
- Xiao Y, Gu X, Niu H, et al. Associations of residential greenness with lung function and chronic obstructive pulmonary disease in China. Environ Res 2022;209:112877. [Crossref] [PubMed]
- Dondi A, Carbone C, Manieri E, et al. Outdoor Air Pollution and Childhood Respiratory Disease: The Role of Oxidative Stress. Int J Mol Sci 2023;24:4345. [Crossref] [PubMed]
- Backes AT, Reinmuth-Selzle K, Leifke AL, et al. Oligomerization and Nitration of the Grass Pollen Allergen Phl p 5 by Ozone, Nitrogen Dioxide, and Peroxynitrite: Reaction Products, Kinetics, and Health Effects. Int J Mol Sci 2021;22:7616. [Crossref] [PubMed]
- Dauchet L, Hulo S, Cherot-Kornobis N, et al. Short-term exposure to air pollution: Associations with lung function and inflammatory markers in non-smoking, healthy adults. Environ Int 2018;121:610-9. [Crossref] [PubMed]
- Joelsson JP, Kricker JA, Arason AJ, et al. Azithromycin ameliorates sulfur dioxide-induced airway epithelial damage and inflammatory responses. Respir Res 2020;21:233. [Crossref] [PubMed]
- Rosário Filho NA, Urrutia-Pereira M, D'Amato G, et al. Air pollution and indoor settings. World Allergy Organ J 2021;14:100499. [Crossref] [PubMed]
- Li J, Song H, Luo T, et al. Exposure to O3 and NO2 on the interfacial chemistry of the pulmonary surfactant and the mechanism of lung oxidative damage. Chemosphere 2024;362:142669. [Crossref] [PubMed]
- Cui L, Zhou J, Peng X, et al. Analyses of air pollution control measures and co-benefits in the heavily air-polluted Jinan city of China, 2013-2017. Sci Rep 2020;10:5423. [Crossref] [PubMed]
- Zhang L, Guo C, Jia X, et al. Short-term effects of ambient air pollution on lung functions in school children: a panel study in Shanghai. Environ Health 2021;38:209-14.
- Gauderman WJ, Urman R, Avol E, et al. Association of improved air quality with lung development in children. N Engl J Med 2015;372:905-13. [Crossref] [PubMed]
- Mokoena KK, Ethan CJ, Yu Y, et al. Ambient air pollution and respiratory mortality in Xi'an, China: a time-series analysis. Respir Res 2019;20:139. [Crossref] [PubMed]
- Chen C, Li C, Li Y, et al. Short-term effects of ambient air pollution exposure on lung function: A longitudinal study among healthy primary school children in China. Sci Total Environ 2018;645:1014-20. [Crossref] [PubMed]
- Yang T, Chen R, Gu X, et al. Association of fine particulate matter air pollution and its constituents with lung function: The China Pulmonary Health study. Environ Int 2021;156:106707. [Crossref] [PubMed]


