
A retrospective cohort study comparing the therapeutic efficacy of three surgical interventions for pediatric flexible flatfoot
Highlight box
Key findings
• Subtalar extra-articular screw arthroereisis (SESA), HyProCure implantation at tarsal sinus, and calcaneo-cuboid-cuneiform (Triple C) osteotomy have all achieved satisfactory radiographic and clinical outcomes in the treatment of symptomatic flexible flatfoot.
What is known, and what is new?
• Existing studies have reported the efficacy of individual surgical techniques (subtalar arthroereisis and Triple C osteotomy) for pediatric flexible flatfoot but lack direct comparative analyses of clinical and radiological outcomes among these methods.
• This study provides the first direct comparison of three surgical interventions in a Chinese cohort, demonstrating that Triple C osteotomy achieves faster deformity correction, while minimally invasive arthroereisis techniques (SESA and HyProCure) reduce operative time and blood loss, with comparable long-term outcomes among all approaches.
What is the implication, and what should change now?
• All three surgical approaches are viable options for treating symptomatic flexible flatfoot in children. However, surgeons need to weigh the advantages and disadvantages of each method. For instance, if the primary goal is to shorten the operative time and reduce blood loss, SESA or HyProCure implantation can be considered. If a more rapid correction of the flatfoot deformity is desired, Triple C osteotomy may be a better choice.
Introduction
Flatfoot is a common condition seen in infants and children, which typically resolves on its own with the development of the medial arch (1,2). In its normal loaded mode, the first and fifth metatarsal bones, as well as the lateral edge of the foot come into contact with the ground. However, when flatfoot occurs, it causes a valgus or displacement of the calcaneus resulting in loss of support at the talus. This leads to a flattening of the arch and an inward leaning during normal loading mode which makes it more likely for heavier weight to be placed on that area when walking. A small number of children with flexible flatfeet may experience persistent pain, limited mobility when walking, and other symptoms which may require surgical treatment if conservative treatments prove unsuccessful (1,3).
Due to the lack of a strict clinical or imaging standard definition, the true incidence rate of flatfoot is still inaccurate (4). The pathogenesis of flexible flatfoot in children remains controversial. While it is generally accepted that muscle imbalance and ligament relaxation are involved, some scholars believe that coordination and normal function of ankle muscles are necessary to maintain the arch of the foot, and that feeble ankle muscles could be an important cause for flexible flatfeet (5). However, electromyogram studies have found that neither the internal nor the external muscles can support or maintain a normal vertical arch of the foot in standing posture (6). This has led some scholars to suggest that it is instead structural bones and ligaments which determine foot longitudinal arch height under static load, while muscles are essential for function and balance but not structural integrity (7,8).
For symptomatic pediatric flexible flatfeet, orthosis, fusion, or osteotomy can be considered for treatment (4). Subtalar arthroereisis is a relatively minimally invasive operation that is used to correct flexible flatfeet and can be divided into tarsal sinus metal implant, tarsal sinus absorbable implant, or subtalar calcaneus stop screw according to the different implants (9,10). Chambers (11) first described subtalar arthroereisis in 1946 as the implantation of a wedge-shaped bone block to impact the posterior edge of the calcaneus and limit forward displacement of the talus on the calcaneus. Rathjen and Mubarak then reported in 1998 on successful results from their use of calcaneo-cuboid-cuneiform (Triple C) osteotomies, which include medial sliding osteotomy of calcaneus, cuboid osteotomy and lengthening, and medial cuneiform closed osteotomies (12). While arthroereisis may lead to degenerative disease and deformity of adjacent articulations which could affect surgical outcomes, Triple C osteotomy can restore anatomical position of the foot without fusion (12). These three treatment methods have a broad overlap in their indications for use in pediatric flexible flatfoot, and clinicians and patients often face the challenge of choosing among them. Presently, most studies on the treatment of pediatric flexible flatfoot focus on the efficacy of a single surgical technique, lacking direct comparisons between different surgical methods. Such comparative studies not only provide more comprehensive evidence-based medical data to guide clinicians in formulating personalized treatment plans based on the specific conditions of their patients but also assess the long-term impact of each method on patients’ health and quality of life. Therefore, this study aims to systematically compare the clinical and radiological outcomes of these three surgical techniques, providing a scientific basis for clinical practice and highlighting significant clinical implications. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-23-610/rc).
Methods
This study is a retrospective cohort study aimed at evaluating the clinical and radiographic outcomes of three different surgical methods (subtalar extra-articular screw arthroereisis (SESA), HyProCure implantation at the tarsal sinus, and Triple C osteotomy) for the treatment of pediatric flexible flatfoot. The study protocol was approved by the ethics committee of Hunan Children’s Hospital (No. KYSQ2021⁃029). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from the patients’ legal guardians. Based on preliminary studies and a literature review, we estimated the efficacy rate of each surgical method to be approximately 70%. To detect a 20% difference at a significance level of 0.05, a minimum of 10 patients per group was required. Considering potential dropout rates, we ultimately included 31 patients (13 boys and 18 girls) with a total of 49 affected feet. The study period was from June 2013 to August 2019, during which the aforementioned 31 patients were enrolled. The mean age of the patients was 10.7 years (range, 6–15 years). All included patients were clinically and radiographically diagnosed with flexible flatfoot.
Clinical assessment included assessment and recording of symptoms, deformity, pain, and difficulty in weight-bearing; while radiological assessment was based on formation of the arch and heel position during weight-bearing. Inclusion criteria: (I) clinically confirmed children aged 6–18 years with flexible flatfeet; and (II) those who experienced stubborn pain, limited walking, or other symptoms that did not improve after 6 months of conservative treatment such as arch support shoes or physical therapy. Exclusion criteria: (I) rigid flatfoot patients; (II) other foot diseases such as neurological disorders or tarsal syndesmosis; and (III) patients who lost follow-up. Data collection covered the results of clinical and radiographic assessments. Clinical variables included the patients’ age, sex, and American Orthopedic Foot and Ankle Society (AOFAS) scores. Radiographic parameters encompassed the anteroposterior (AP) talo-first metatarsal angle, lateral talo-first metatarsal angle, and AP talocalcaneal angle under weight-bearing conditions, etc. All surgeries were performed by the same surgical team to ensure consistency and comparability of the procedures. Postoperative follow-up was conducted every 3–6 months and included clinical evaluations and radiographic examinations. The primary follow-up outcomes were the AOFAS scores and changes in radiographic parameters, aimed at comprehensively assessing surgical outcomes.
Clinical data collection
The collected patient data included age at the time of surgery, operative time, intraoperative blood loss, completion time of correction, as well as preoperative and follow-up imaging data. The AOFAS was used to evaluate ankle function postoperatively.
Radiological parameters
All cases underwent weight-bearing AP and lateral X-rays of the foot at the time of preoperative and postoperative, hardware removal, and final follow-up, with measurements taken for the AP talo-first metatarsal angle, lateral talo-first metatarsal angle, AP talocalcaneal angle, talo-navicular coverage angle, calcaneal pitch angle, and lateral talocalcaneal angle. Three pediatric orthopedic surgeons independently performed the measurements to ensure the reliability of the results.
Operation
All patients were placed in a supine position and a pneumatic tourniquet was applied to the mid-thigh. The surgical field skin was disinfected with 0.5% complexed iodine and sterile towel sheets were laid.
SESA: slightly rotate the affected limb inward, keeping the subtalar articulation in an internally rotated position. Make a transverse incision about 2 cm long on the surface of the tarsal sinus. Passively separate the fat tissue at the tarsal sinus and use the technique to adduct forefoot and midfoot, turning calcaneus inward, while observing inner and outer ankles from sole of foot. Under C-arm fluoroscopy, insert K-wire into calcaneus from outside to inside, at outer upper edge of calcaneus in front of lateral process of talus; pay attention to maintaining direction that is relatively perpendicular to subtalar articulation. After confirming satisfactory position of K-wire in calcaneus via C-arm fluoroscopy, slowly place hollow cancellous bone screws with appropriate length and diameter into calcaneus. Perform C-arm fluoroscopy again to confirm correct placement of screw in calcaneus.
HyProCure implantation of tarsal sinus: perform a transverse incision of approximately 2 cm in length on the dorsolateral side of the tarsal sinus, and clear away any soft tissue within the tarsal canal. Utilize a K-wire as a guide needle for inserting the tarsal canal, then screw on the appropriate HyProCure device adapter (GraMedica, Macomb, MI, USA) along this guide needle. Under C-arm fluoroscopy, remove this adapter and push the HyProCure device into the tarsal sinus. Re-confirm its position under C-arm fluoroscopy once more.
3C osteotomy: an oblique incision is made along the lower edge of the peroneus longus and peroneus brevis tendons from the posterior upper edge of the calcaneal tubercle. After dividing the skin, the sural nerve and peroneal tendon are pulled to the dorsum of the foot to expose the lateral surface of the calcaneus. A fluoroscopic examination is then conducted in order to mark an osteotomy line that runs parallel to the posterior calcaneal articulation surface along its outer upper edge and lower back. An electric saw is utilized to perform a triple C osteotomy, which involves preserving the integrity of the medial periosteum while moving the distal end of the saw medially and plantarly to correct any calcaneus valgus present. K-wire or steel plate fixation is then used to secure both ends of the osteotomy. The foot is extended dorsally to ensure stable compression at the osteotomy site before a straight incision is made on the medial side of the medial cuneiform bone. This incision exposes the bone for a closing wedge osteotomy on the metatarsal side of the middle third of the cuneiform bone, which helps to rebuild the arching of the forefoot flexion/pronation. To expose the cuboid bone, the distal part of the calcaneal incision is extended while the fibular tendon is pulled plantarly. This allows for an osteotomy to be performed on the middle cuboid bone, with the insertion cuneiform bone block fixed using K-wire, screw, or steel plate afterwards.
For those with Achilles tendon contracture, an Achilles tendon lengthening operation should be performed before hemostasis, wound washing and suturing with absorbable thread are completed.
Postoperative treatment
The patient was re-examined at the outpatient department 2- and 6-week post-surgery, during which they were not permitted to bear any weight. All patients are followed up in the outpatient clinic every 6 months postoperatively, and weight-bearing AP and lateral X-rays of both feet are taken. As per the follow-up imaging data of the children, the SESA group and HyProCure group should remove their internal fixation devices once the flatfoot deformity has been corrected. For those in the Triple C osteotomy group, they can take out their internal fixation devices after fusion at the osteotomy site has been observed during follow-up. Post removal of these devices, patients should continue walking with arch support ankle-foot orthosis or braces for 4 to 6 weeks before transitioning to sports shoes.
Statistical analysis
All data are expressed as mean ± standard deviation and were analyzed using SPSS version 21.0. When the data followed a normal distribution and had homogeneous variances, paired t-tests or one-way analysis of variance were used for statistical analysis. If the data did not follow a normal distribution or had heterogeneous variances, the Mann-Whitney U test or Wilcoxon signed-rank test was employed. The level of statistical significance was set at a two-tailed P<0.05.
Results
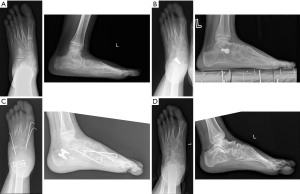
According to the above inclusion criteria, 31 patients were recruited for this study. SESA was adopted in 10 feet (SESA group), HyProCure implantation in 21 feet (HyProCure group), and Triple C osteotomy in 18 feet (Triple C osteotomy group). The operative time in the SESA and HyProCure groups (31.3±6.3 and 29.2±11.6 min, respectively) was significantly lower than that in the Triple C osteotomy group (93.1±15.8 min, P<0.05). Similarly, the intraoperative bleeding in the SESA and HyProCure groups (13.7±4.8 and 14.2±5.6 mL, respectively) was also significantly lower than that observed in the Triple C osteotomy group (41.9±19.9 mL, P<0.05). Compared to the SESA group and HyProCure, the triple C group achieves a shorter correction time for flatfoot (P<0.05) (Table 1). Postoperative follow-up was conducted for at least 32 months, with an average of 41 months. With satisfactory clinical outcomes being observed in all three groups: AOFAS score increased significantly from preoperative values of 44.5±6 to 85.5±8.6 for SESA group, 45.8±5.5 to 84.6±6.6 for HyProCure group, and 42.9±6.7 to 82.9±6.3 for Triple C osteotomy group (Table 2, Figure 1).
Table 1
| Parameter | SESA group (n=10) | HyProCure group (n=21) | Triple C group (n=18) | P1 | P2 | P3 |
|---|---|---|---|---|---|---|
| Age at surgery (years) | 10.6±1.6 | 10±1.6 | 11.7±3.6 | 0.49 | 0.25 | 0.53 |
| Operative time (min) | 31.3±6.3 | 29.2±11.6 | 93.1±15.8 | <0.01 | <0.01 | 0.66 |
| Intraoperative bleeding (mL) | 13.7±4.8 | 14.2±5.6 | 41.9±19.9 | <0.01 | <0.01 | 0.89 |
| Time of orthopedic (months) | 43.5±9.9 | 39.7±13.5 | 13.2±7 | <0.01 | <0.01 | 0.56 |
Data are presented as mean ± standard deviation. P1: SESA group vs. Triple C group; P2: HyProCure group vs. Triple C group; P3: SESA group vs. HyProCure group. HyProCure group: HyProCure implantation at tarsal sinus. SESA, subtalar extra-articular screw arthroereisis; Triple C, calcaneo-cuboid-cuneiform.
Table 2
| Point of time | AOFAS scale | P1 | P2 | P3 | ||
|---|---|---|---|---|---|---|
| SESA | HyProCure | Triple C | ||||
| Preoperative | 44.5±6 | 45.8±5.5 | 42.9±6.7 | 0.692 | 0.294 | 0.687 |
| Last follow-up | 85.5±8.6 | 84.6±6.6 | 82.9±6.3 | 0.556 | 0.572 | 0.826 |
| P4 | <0.01 | <0.01 | <0.01 | |||
Data are presented as mean ± standard deviation. P1: SESA group vs. Triple C group; P2: HyProCure group vs. Triple C group; P3: SESA group vs. HyProCure group; P4: preoperative vs. last follow-up. HyProCure group: HyProCure implantation at tarsal sinus. AOFAS, American Orthopedic Foot and Ankle Society; SESA, subtalar extra-articular screw arthroereisis; Triple C, calcaneo-cuboid-cuneiform.

Regarding radiologic results, the last follow-up of the three groups concerning AP talo-first metatarsal angle, lateral talo-first metatarsal angle, AP talocalcaneal angle, talo-navicular coverage angle, and calcaneal pitch angle showed a marked improvement when compared to preoperative conditions (Table 3). Moreover, the measurement of the lateral talocalcaneal angle revealed no considerable differences between the three groups at the final follow-up prior to surgery. Clinical and imaging outcomes were also found to be similar across all three groups. No significant differences were found among the three groups regarding preoperative radiological parameters except talonavicular coverage and lateral talo-first metatarsal angle in the HyProCure and Triple C groups (Table 4). One special case involved a child who underwent implantation at tarsal sinus using the HyProCure method but whose deformity had not been corrected satisfactorily 34 months later; this was followed by a successful recovery of longitudinal arch on left foot after performing a subsequent Triple C osteotomy procedure accompanied by disappearance of walking pains symptoms (Figure 2).
Table 3
| Radiologic parameter | Preoperative | Postoperative | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SESA | HyProCure | Triple C | P1 | P2 | P3 | SESA | HyProCure | Triple C | P1 | P2 | P3 | ||
| AP talo-first MTT angle | 19.6±7.6 | 19.2±6.1 | 21.9±6.7 | 0.496 | 0.238 | 0.885 | 10.4±3.6 | 11.6±5.9 | 11.2±5.9 | 0.776 | 0.843 | 0.642 | |
| AP talocalcaneal angle | 29.4±8.5 | 31.5±5.4 | 31.2±8.8 | 0.662 | 0.914 | 0.453 | 23.5±6 | 23.8±4.6 | 26.1±7.3 | 0.435 | 0.276 | 0.885 | |
| Talonavicular coverage | 22±4.7 | 20.2±5 | 24.7±6.6 | 0.352 | 0.032* | 0.42 | 10.2±4.1 | 11.3±3.9 | 12.7±5.7 | 0.307 | 0.392 | 0.519 | |
| L talo-first MTT angle | 19.6±7.3 | 18±5.6 | 21.3±5.9 | 0.59 | 0.117 | 0.548 | 5.3±3.7 | 5.7±2.6 | 8.7±4.3 | 0.094 | 0.017* | 0.749 | |
| Calcaneal pitch | 11.4±1.8 | 9.9±3 | 11.5±4.6 | 0.929 | 0.25 | 0.269 | 19.7±4.7 | 21.1±5.2 | 23.4±5.4 | 0.152 | 0.221 | 0.562 | |
| L talocalcaneal angle | 38.8±8.4 | 39.3±6.4 | 42.6±4.5 | 0.203 | 0.116 | 0.87 | 36.8±6.2 | 38.4±3.4 | 40.6±3.9 | 0.114 | 0.099 | 0.402 | |
Data are presented as mean ± standard deviation. *, P<0.05. P1: SESA group vs. Triple C group; P2: HyProCure group vs. Triple C group; P3: SESA group vs. HyProCure group. HyProCure group: HyProCure implantation at tarsal sinus. AP, anteroposterior; L, lateral; MTT, metatarsal; SESA, subtalar extra-articular screw arthroereisis; Triple C, calcaneo-cuboid-cuneiform.
Table 4
| Radiologic parameter | SESA group | HyProCure group | Triple C group | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | P | Pre-op | Post-op | P | Pre-op | Post-op | P | |||
| AP talo-first MTT angle | 19.6±7.6 | 10.4±3.6 | 0.017 | 19.2±6.1 | 11.6±5.9 | <0.001 | 21.9±6.7 | 11.2±5.9 | <0.001 | ||
| AP talocalcaneal angle | 29.4±8.5 | 23.5±6 | 0.015 | 31.5±5.4 | 23.8±4.6 | <0.001 | 31.2±8.8 | 26.1±7.3 | 0.002 | ||
| Talonavicular coverage | 22±4.7 | 10.2±4.1 | <0.001 | 20.2±5 | 11.3±3.9 | <0.001 | 24.7±6.6 | 12.7±5.7 | <0.001 | ||
| L talo-first MTT angle | 19.6±7.3 | 5.3±3.7 | <0.001 | 18±5.6 | 5.7±2.6 | <0.001 | 21.3±5.9 | 8.7±4.3 | <0.001 | ||
| Calcaneal pitch | 11.4±1.8 | 19.7±4.7 | 0.002 | 9.9±3 | 21.1±5.2 | <0.001 | 11.5±4.6 | 23.4±5.4 | <0.001 | ||
| L talocalcaneal angle | 38.8±8.4 | 36.8±6.2 | 0.248 | 39.3±6.4 | 38.4±3.4 | 0.495 | 42.6±4.5 | 40.6±3.9 | 0.083 | ||
Data are presented as mean ± standard deviation. HyProCure group: HyProCure implantation at tarsal sinus. AP, anteroposterior; L, lateral; MTT, metatarsal; pre-op, preoperative; post-op, postoperative; SESA, subtalar extra-articular screw arthroereisis; Triple C, calcaneo-cuboid-cuneiform.
Tarsal sinus pain was reported by 10% of patients treated with SESA and 14% of those treated with HyProCure implants; no patient required removal of internal fixation due to obvious pain while 10% experienced fibular muscle contracture after SESA surgery; 16.7% reported wound pain after Triple C osteotomy treatment without any serious complications such as internal fixation loosening or nonunion occurring during follow-up period across all three study groups. There were no cases of recurrence in any of the three patient groups during the follow-up period.
Discussion
This study assessed the clinical effects and radiological outcomes of children with symptomatic, flexible flatfeet treated with arthroereisis and Triple C osteotomy. Subtalar arthroereisis was mainly utilized, with the HyProCure device of subtalar articulation made from titanium alloy inserted into the tarsal sinus, its head located behind the talus to limit internal rotation. Twenty-one feet were treated in this manner, with an average correction time of 39.7 months and satisfactory results achieved. HyProCure device implanted at tarsal sinus is becoming increasingly popular due to its simple operation and definite efficacy; however, there is still a lack of follow-up studies on its long-term efficacy (13-15). Smith and Millar (16) [1983] reported that blocking screws could be inserted into the calcaneus via the tarsal sinus for calcaneal arrest in order to preserve foot function and limit excessive forward movement of the talus. In our SESA group, screws were inserted into the calcaneus along the tarsal sinus to effectively support the talus, avoiding contact between it and bottom of tarsal sinus while reducing talar adduction deformity. Ten feet were treated in this manner over an average correction time of 43.5 months achieving satisfactory postoperative results; it is a simple operation that is cost-effective as well as being able to be used alone or as an auxiliary treatment for parascaphoid syndrome or tarsal syndesmosis (17,18).
Some scholars have reported that Triple C osteotomy can achieve satisfactory results in the treatment of flexible flatfeet and the restoration of foot anatomy (19,20). Kim et al. (21) found that Triple C osteotomy was more effective than calcaneus lengthening in correcting severe flatfoot deformity in children. We treated 18 children with flexible flatfeet through Triple C osteotomy and achieved satisfactory results, basically consistent with the outcomes reported by Agashe et al. and Kim et al. (19,20).
Our postoperative results suggest that all three surgical methods can achieve satisfactory outcomes in the treatment of flexible flatfoot. Imaging measurement indexes, including AP talo-first metatarsal angle and lateral talo-first metatarsal angle, as well as AOFAS scores showed no significant differences between the three methods. In terms of operative time and intraoperative bleeding, HyProCure group and SESA group were significantly better than Triple C osteotomy group; however, the latter required less time to correct flatfeet compared to the other two groups. In terms of complications, all three groups presented symptoms of localized wound or sinus tarsi pain. The SESA group, HyProCure group, and Triple C group had incidence rates of 10%, 14.3%, and 16.7%, respectively, with no significant differences observed between the groups. All patients experiencing localized pain were successfully treated with conservative measures such as pain medication and physical therapy to address this complication. In the SESA group, due to the obstruction caused by the implanted screws, patients often adopt a passive position of pronation for pain relief, leading to complications such as peroneal muscle contracture (22,23). We identified one case of peroneal muscle contracture in the SESA group during follow-up, and the symptoms disappeared after physical therapy and the use of a plantar orthosis.
The SESA and the implantation of HyProCure devices at the tarsal sinus are relatively simple and straightforward procedures with a low learning curve, which facilitates their promotion and application. Fibular muscle contracture appears to be a specific complication of SESA, which may be related to patients’ stimulation of pain and tarsal sinus mechanoreceptors (24). Implantation of the tarsal sinus device can lead to complications such as tarsal sinus pain or joint effusion. de Bot et al. (25) reported that 26% of patients required a second revision surgery due to an incorrect selection of the size of the tarsal sinus implant. Triple C osteotomy has the advantage that it does not interfere with the articular surface, but is more traumatic and requires higher experience and knowledge in anatomy from the operator. We can observe that implantation of subtalar extra-articular screws or HyProCure devices is slow and follows regular follow-up visits. When orthopedic effects are unsatisfactory or other complications occur, these implants can be removed, providing some degree of reversibility; they can also be treated using osteotomy again.
Despite some limitations, such as a relatively small sample size and short follow-up period, our study is one of the first to report on Triple C osteotomy for the Chinese population. To gain a more comprehensive understanding of its efficacy, we recommend conducting long-term follow-up studies to assess whether there are any recurrences of malformations or symptoms, as well as initiating active prospective research.
Conclusions
The three types of operations can achieve satisfactory results in the treatment of flexible flatfoot without serious complications. From our experience, we tend to use more “minimally invasive” surgical methods such as implanting subtalar extra-articular screws or HyProCure devices for symptomatic flexible flatfoot. Although these two methods require a longer orthopedic period, the curative effect is definite. Additionally, the symptoms may reduce over time during the correction process, thus avoiding the need for extensive orthopedic surgery. However, it is important to note that subtalar extra-articular screws or HyProCure devices must be followed up on and monitored closely for any potential complications such as articulation degeneration.
Acknowledgments
We are grateful to all the patients who accepted to participate in this study.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-23-610/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-610/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-23-610/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-23-610/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the ethics committee of Hunan Children’s Hospital (No. KYSQ2021⁃029). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Informed consent was obtained from the patients’ legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Molina-García C, Banwell G, Álvarez-Salvago F, et al. Efficacy of Functional Re-Education as a Treatment for Infantile Flexible Flatfoot: Systematic Review. Children (Basel) 2024;12:8. [Crossref] [PubMed]
- Kim HY, Shin HS, Ko JH, et al. Gait Analysis of Symptomatic Flatfoot in Children: An Observational Study. Clin Orthop Surg 2017;9:363-73. [Crossref] [PubMed]
- Yontar NS, Ogut T, Guven MF, et al. Surgical treatment results for flexible flatfoot in adolescents. Acta Orthop Traumatol Turc 2016;50:655-9. [Crossref] [PubMed]
- Xu L, Gu H, Zhang Y, et al. Risk Factors of Flatfoot in Children: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health 2022;19:8247. [Crossref] [PubMed]
- Tahmasbi A, Shadmehr A, Attarbashi Moghadam B, et al. Does Kinesio taping of tibialis posterior or peroneus longus have an immediate effect on improving foot posture, dynamic balance, and biomechanical variables in young women with flexible flatfoot? Foot (Edinb) 2023;56:102032. [Crossref] [PubMed]
- Koyama K, Yamauchi J. Increased toe flexor strength does not relate to altered postural sway during static upright standing after 12 weeks of multicomponent exercise training. Eur J Sport Sci 2023;23:520-9.
- Mann R, Inman VT. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am 1964;46:469-81.
- Huang CK, Kitaoka HB, An KN, et al. Biomechanical evaluation of longitudinal arch stability. Foot Ankle 1993;14:353-7. [Crossref] [PubMed]
- Vescio A, Testa G, Amico M, et al. Arthroereisis in juvenile flexible flatfoot: Which device should we implant? A systematic review of literature published in the last 5 years. World J Orthop 2021;12:433-44. [Crossref] [PubMed]
- Vogt B, Toporowski G, Gosheger G, et al. Subtalar Arthroereisis for Flexible Flatfoot in Children-Clinical, Radiographic and Pedobarographic Outcome Comparing Three Different Methods. Children (Basel) 2021;8:359. [Crossref] [PubMed]
- Chambers EF. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol 1946;54:77-86.
- Rathjen KE, Mubarak SJ. Calcaneal-cuboid-cuneiform osteotomy for the correction of valgus foot deformities in children. J Pediatr Orthop 1998;18:775-82.
- Pavone V, Testa G, Vescio A, et al. Diagnosis and treatment of flexible flatfoot: results of 2019 flexible flatfoot survey from the European Paediatric Orthopedic Society. J Pediatr Orthop B 2021;30:450-7. [Crossref] [PubMed]
- Pavone V, Vescio A, Andreacchio A, et al. Results of the Italian Pediatric Orthopedics Society juvenile flexible flatfoot survey: diagnosis and treatment options. J Pediatr Orthop B 2022;31:e17-23. [Crossref] [PubMed]
- Longo UG, Papalia R, De Salvatore S, et al. Trends in hospitalisation of Subtalar Joint Arthroereisis in Italy from 2009 to 2016. Foot Ankle Surg 2022;28:258-62. [Crossref] [PubMed]
- Smith SD, Millar EA. Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res 1983;15-23.
- Elmarghany M, Abd El-Ghaffar TM, Elgeushy A, et al. Is subtalar extra articular screw arthroereisis (SESA) reducing pain and restoring medial longitudinal arch in children with flexible flat foot? J Orthop 2020;20:147-53. [Crossref] [PubMed]
- Shah NS, Needleman RL, Bokhari O, et al. 2013 Subtalar Arthroereisis Survey: The Current Practice Patterns of Members of the AOFAS. Foot Ankle Spec 2015;8:180-5. [Crossref] [PubMed]
- Kim JR, Park CI, Moon YJ, et al. Concomitant calcaneo-cuboid-cuneiform osteotomies and the modified Kidner procedure for severe flatfoot associated with symptomatic accessory navicular in children and adolescents. J Orthop Surg Res 2014;9:131. [Crossref] [PubMed]
- Agashe MV, Sagade BS, Bansal AV. Functional and Radiological Outcomes Following Calcaneo-Cuboid-Cuneiform Osteotomy for the Treatment of Planovalgus Feet: A Short-Term Analysis. Indian J Orthop 2021;55:119-27. [Crossref] [PubMed]
- Kim JR, Shin SJ, Wang SI, et al. Comparison of lateral opening wedge calcaneal osteotomy and medial calcaneal sliding-opening wedge cuboid-closing wedge cuneiform osteotomy for correction of planovalgus foot deformity in children. J Foot Ankle Surg 2013;52:162-6. [Crossref] [PubMed]
- De Pellegrin M, Moharamzadeh D, Strobl WM, et al. Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children. J Child Orthop 2014;8:479-87. [Crossref] [PubMed]
- Bobiński A, Tomczyk Ł, Pelc M, et al. Arthroereisis with a Talar Screw in Symptomatic Flexible Flatfoot in Children. J Clin Med 2023;12:7475. [Crossref] [PubMed]
- Rein S, Hagert E, Hanisch U, et al. Immunohistochemical analysis of sensory nerve endings in ankle ligaments: a cadaver study. Cells Tissues Organs 2013;197:64-76. [Crossref] [PubMed]
- de Bot RTAL, Stevens J, Hermus JPS, et al. Clinical and Radiological Outcomes of Subtalar Kalix II Arthroereisis for a Symptomatic Pediatric Flexible Flatfoot. Foot Ankle Spec 2021;14:9-18. [Crossref] [PubMed]


