
Congenital patellar dislocation with genu valgum and Klinefelter syndrome: a case report
Highlight box
Key findings
• This case report details the successful surgical treatment of a 3-year-old child with a rare combination of bilateral congenital patellar dislocation (CPD), genu valgum, and Klinefelter syndrome, highlighting the importance of simultaneous surgical correction.
What is known and what is new?
• CPD with associated genu valgum is very rare in children. This case demonstrates the efficacy of simultaneous medial reefing, lateral release, and bilateral temporary tibial epiphysiodesis in addressing this complex presentation.
• Based on literature review and our clinical experience, we recommend early completion of diagnostic evaluations to confirm the underlying etiology, followed by surgical intervention at approximately 3 years of age, as children in this age group demonstrate improved tolerance to the procedure and favorable postoperative recovery outcomes.
What is the implication, and what should change now?
• For CPD, the lower extremity alignment should be carefully assessed, and associated knee deformities may be addressed successfully at the same procedure.
Introduction
Congenital patellar dislocation (CPD) is a severe and complex form of patellar dislocation, most commonly affecting children under 10 years old (1). It is frequently associated with conditions such as arthrogryposis, Larsen syndrome, dyschondrosteosis, and Rubinstein-Taybi syndrome (2). Early diagnosis is often challenging because the patella may be invisible on birth X-rays, and its underdeveloped state can make it difficult to assess, consequently, CPD is frequently overlooked (3). For CPD cases, depending on the clinical presentation, surgical options such as proximal or distal realignment may be performed individually or in combination to reduce or stabilize the patella. While genu valgum is a risk factor for patellar dislocation in general (4), for CPD combined with genu valgum, established surgical guidelines are lacking due to the rarity and complexity of the condition (5). There is no consensus on whether to perform simultaneous or staged surgery. If staged surgery is chosen, the optimal sequence—addressing genu valgum first or patellar dislocation first—remains controversial. We present this case in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2024-594/rc).
Case presentation
A 3-year-old boy presented with bilateral CPD, bilateral genu valgum and Klinefelter syndrome. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patient’s parent for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
The boy was initially diagnosed with “bilateral patellar dislocation” at age 1 at a local hospital and received no treatment. At age 2 (January 2021), he was re-evaluated at the same hospital, diagnosed with bilateral CPD and genu valgum, and was given brace treatment and observation. On July 11, 2021, he was presented to our institution. Clinical examination revealed a waddling gait and bilateral genu valgum (with knees touching, 9 cm ankle-to-ankle distance). Both patella demonstrated lateral dislocation with the left patella being reducible during knee extension, while the right patella remained persistently irreducible. No lower limb discrepancy was found. There was no joint tenderness and effusion bilaterally. Lower limb muscle tone, spinal curvature, peripheral circulation, and sensation were normal.
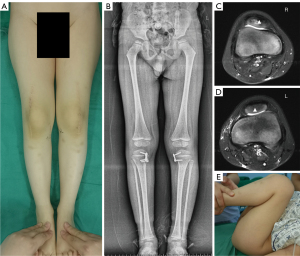
Preoperative X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) (see Figure 1) were performed to confirm bilateral CPD. A systematic evaluation excluded potential contributing pathological factors such as ligamentous laxity, musculoskeletal dysplasia, skeletal abnormalities, and neuromuscular disorders. Comprehensive radiographic analysis revealed: left mechanical tibiofemoral angle (MTFA) 173°, right MTFA 170°; left medial proximal tibial angle (MPTA) 93°, right MPTA 94°; left lateral distal femur angle (LDFA) 88°; right LDFA 89°; left tibial tubercle-trochlear groove distance (TT-TG) 2.54 cm, right TT-TG 2.26 cm; left joint line convergence angle (JLCA) 4°, right JLCA 7°. Increased MPTA and JLCA, with the MFTA change approximating the sum of the changes in MPTA and JLCA, indicated that genu valgum correction should target both the proximal tibia and the knee joint. Bilateral open reduction of the patellar dislocations and temporary proximal tibial epiphysiodesis using an eight-plate system were performed under general anesthesia.

Each side was operated on sequentially. The right-side procedure (described as an example) began with application of a tourniquet. A 15-cm anterior midline incision was made, extending approximately 5 cm superior to the patella and down to the tibial tubercle. The quadriceps muscle, patellar tendon, and patella were exposed in layers. Lateral patellar displacement was noted, with significant tension on the lateral retinaculum and iliotibial band (see Figure 2). The medial and lateral retinaculum were partially released along the patellar margins, and the medial and lateral quadriceps tendons were partially tenotomized, preserving a 1-cm central strip. The lateral retinacular release extended to the patellar tendon insertion. A Z-lengthening plasty (approximately 1 cm) was performed on the iliotibial band to release the lateral knee joint. The patella was reduced, and the medial retinaculum was re-attached to the patella and quadriceps using an overlapping suture technique; the lateral repair involved only partial synovial closure. Passive range of motion testing confirmed satisfactory patellar stability. Fluoroscopic guidance was used to locate the medial proximal tibial epiphyseal plate; a 2-cm longitudinal incision exposed the bone, allowing insertion of a guide pin and subsequent eight-plate fixation with two screws. Intraoperative blood loss was approximately 20 mL. Bilateral long leg casts were applied for immobilization.

The child was discharged 3 days postoperatively and maintained cast immobilization for 6 weeks, with non-weight bearing for the first 3 weeks, followed by assisted ambulation with support for the remaining 3 weeks. A formal rehabilitation plan was not implemented for such a young child; instead, parents were instructed to initiate pain-free active range-of-motion and quadriceps strengthening exercises 2 weeks after cast removal. At the ten-month postoperative follow-up on May 9, 2022, the cosmetic appearance of the knee was satisfactory (see Figure 3A); the full-length lower extremity radiographic examination (see Figure 3B) revealed well-aligned patella and satisfactory lower extremity alignment; bilateral knee MRI (see Figure 3C,3D) showed TT-TG distances of approximately 1.1 cm on the left and 1.2 cm on the right, patellar tilt angles of approximately 8° (left) and 11° (right), and stable patellar fixation; the knee flexion was unlimited (see Figure 3E); and the eight plates were removed at this time. The child continues regular follow-up visits, demonstrating normal gait, well-aligned lower extremities, and stable patellar fixation.
Discussion
CPD associated with genu valgum is uncommon, especially in cases with Klinefelter syndrome, lacking standardized surgical protocols and correction sequences. While there’s no consensus on the optimal timing of surgery for uncomplicated CPD, the literature showed the lowest treatment age was around 1.5 to 3 years, which might improve outcomes and reduce recurrence rates (1,6).
For the case, patellar dislocation and genu valgum may exert reciprocal influences. Following patellar dislocation, tension on the lateral retinaculum and iliotibial band can contribute to and exacerbate genu valgum. Conversely, genu valgum alters joint mechanics, worsening patellar instability. In a staged surgical approach, addressing patellar dislocation first risks instability due to persistent genu valgum, while prioritizing genu valgum correction with temporary epiphyseal arrest (requiring over a year for alignment correction) delays functional recovery, prolongs treatment, and may increase the difficulty of subsequent patellar reduction. Therefore, simultaneous correction was chosen.
Patellar dislocation often involves multiple anatomical abnormalities, including femoral trochlear dysplasia, lateralized tibial tuberosities, and lower limb malalignment. Preoperative imaging (X-rays for bone structure, CT for three-dimensional alignment, and MRI for soft tissue assessment) is crucial for comprehensive anatomical evaluation and personalized surgical planning. Surgical options for isolated CPD range from lateral releases and patellar tendon procedures (Insall proximal realignment, Roux-Goldthwait hemi-transfer, stepwise quadriceps lengthening) to patellar stabilization techniques, often used in combination. For recurrent and habitual dislocation cases, medial patellofemoral ligament (MPFL) reconstruction is more prevalent. In pediatric patients with skeletal immaturity—marked by young age, small patellar dimensions, and active growth plates—MPFL procedures carry inherent risks of physeal injury. Moreover, the reconstructed ligament may become anatomically incompatible as the knee joint matures due to ongoing skeletal growth.
Although the literature suggests that hemiepiphysiodesis should be used cautiously in children under 8 years old (7), as they may have the potential for spontaneous correction of deformities or physiological genu valgum. However, considering the clear pathological severity of this patient’s lower limb deformity and the significant malalignment, we cautiously opted for surgical intervention as part of the treatment plan to prevent recurrence. In addition, the TT-TG distance could decrease gradually as the tibial tuberosity could medialize during the MPTA became lower.
Thus, for this patient, the surgical strategy prioritized medial retinacular reefing and lateral release to stabilize the patella, supplemented by temporary hemiepiphysiodesis using an eight-plate system to address genu valgum. According to the preoperative measurements, the knee valgum came from proximal tibia and knee joint, which owing to the tight later retinaculum and iliotibial band. So the iliotibial band lengthening was performed at the same time.
Given the absence of established genu valgum correction angle guidelines in CPD, regular postoperative monitoring and timely adjustments are crucial (8). Lower extremity alignment restoration served as our primary correction endpoint.
The patient’s Klinefelter syndrome (48, XXYY karyotype confirmed by genetic testing) further complicated the case. While CPD is associated with mutations in genes such as LMX1B and TBX4 on autosomes (9), the underlying relationship between Klinefelter syndrome, CPD, and genu valgum remains unclear. Further research, including long-term cohort studies, functional genomics, and biomechanical modeling, is needed to elucidate potential shared etiological pathways. Continued monitoring of motor function, quality of life, and overall medical history, will guide future management.
Conclusions
This case report describes a child with bilateral CPD and genu valgum with the Klinefelter syndrome. Successful treatment was achieved using medial reefing, lateral release, and bilateral temporary tibial epiphysiodesis. Given the complexity and severity of this condition, early diagnosis and intervention are crucial to minimize long-term effects on growth, development, and motor function. Prolonged follow-up is recommended to monitor for recurrence and allow for treatment plan adjustments as needed.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2024-594/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-2024-594/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2024-594/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent was obtained from the patient’s parent for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Parikh SN, Lopreiato N, Veerkamp M. 4-in-1 Quadricepsplasty for Habitual and Fixed Lateral Patellar Dislocation in Children. J Pediatr Orthop 2023;43:237-45. [Crossref] [PubMed]
- Sever R, Fishkin M, Hemo Y, et al. Surgical Treatment of Congenital and Obligatory Dislocation of the Patella in Children. J Pediatr Orthop 2019;39:436-40. [Crossref] [PubMed]
- Yan Z, Yao Y, Yang Q, et al. Application of ultrasound in the early diagnosis of congenital patellar dislocation: a case description. Quant Imaging Med Surg 2023;13:7362-6. [Crossref] [PubMed]
- Berruto M, Ferrua P, Carimati G, et al. Patellofemoral instability: classification and imaging. Joints 2013;1:7-14. [PubMed]
- Pedrotti L, Bertani B, De Rosa F, et al. Congenital Dislocation of the Patella - Surgical Treatment Rationale and Literature Review. J Orthop Case Rep 2021;11:59-64. [Crossref] [PubMed]
- Mo Y, Jing Y, Wang D, et al. Modified Langenskiöld procedure for congenital patella dislocations in pediatric patients. BMC Musculoskelet Disord 2022;23:241. [Crossref] [PubMed]
- Redler LH, Wright ML. Surgical Management of Patellofemoral Instability in the Skeletally Immature Patient. J Am Acad Orthop Surg 2018;26:e405-15. [Crossref] [PubMed]
- Bachman DR, Phillips D, Veerkamp MW, et al. MPFL Reconstruction and Implant-Mediated Guided Growth in Skeletally Immature Patients With Patellar Instability and Genu Valgum. Am J Sports Med 2024;52:698-704. [Crossref] [PubMed]
- Bongers EM, van Kampen A, van Bokhoven H, et al. Human syndromes with congenital patellar anomalies and the underlying gene defects. Clin Genet 2005;68:302-19. [Crossref] [PubMed]


