
Delayed diagnosis of isolated congenital H-type tracheoesophageal fistula: a case report of surgical repair supported by TachoSil® as an adjunct in chronically inflamed tissues
Highlight box
Key findings
• Delayed diagnosis of isolated congenital H-type tracheoesophageal fistula (TEF) can lead to chronic inflammation, fibrosis, and increased surgical complexity.
• A fibrinogen-thrombin-coated hemostatic patch was successfully used to reinforce the suture lines in the repair of an H-type TEF, minimizing air leaks and postoperative complications.
• The patient recovered without early or late complications, demonstrating the feasibility of this surgical approach in challenging cases.
What is known and what is new?
• H-type TEF is a rare congenital anomaly that can be difficult to diagnose, especially when symptoms are subtle or attributed to other conditions such as recurrent respiratory infections or gastroesophageal reflux.
• This case highlights the challenges of diagnosing and surgically managing an H-type TEF in a patient with chronic inflammation. The use of a fibrin-based hemostatic patch to reinforce tissue repair is presented as a viable adjunct for improving postoperative outcomes.
What is the implication, and what should change now?
• Delayed diagnosis of H-type TEF can result in complex anatomical variations and chronic tissue inflammation, requiring meticulous surgical planning.
• Pediatricians and surgeons should maintain a high index of suspicion for TEF in children with recurrent respiratory infections. Additionally, the use of advanced surgical biomaterials should be considered to enhance suture durability and reduce postoperative complications in high-risk cases.
Introduction
H-type tracheoesophageal fistulas (TEFs) are a rare congenital anomaly characterized by an abnormal connection between the trachea and the esophagus (1). Due to its severe respiratory and gastrointestinal complications, this condition requires careful clinical management, mainly when associated with a delayed diagnosis (1).
According to Gross’s classification, H-type TEFs are considered part of the spectrum of esophageal atresia (EA) defects and represent 8% of cases (2). H-type TEFs are typically identified shortly after birth. However, in some cases, their presence may not be discovered until later in childhood, especially when presenting with subtle but recurrent respiratory symptoms (1).
We presented the case of a 14-year-old girl whose H-type TEF was only diagnosed after a prolonged history of recurrent respiratory tract infections. This highlighted the challenges of the diagnosis and the possible respiratory complications associated with a delayed definitive diagnosis. We also discussed the use of TachoSil® (Corza Medical, Linz, Austria), a hemostatic patch, as a potential surgical adjunct for managing the H-type TEF procedure, intending to improve outcomes and prevent postoperative complications, as shown in other cases in the available literature (2,3). We present this case in accordance with the CARE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-72/rc).
Case presentation
A 14-year-old girl was referred to our pediatric tertiary care center due to a long-standing history of recurrent upper respiratory tract infections that began in early childhood. Initially, she had been diagnosed with bronchiolitis and bronchospasm, which necessitated multiple hospital admissions and treatment with continuous positive airway pressure (CPAP). At the age of one, she was also diagnosed with gastroesophageal reflux disease (GERD) and was prescribed proton pump inhibitors (PPIs), though adherence to the medication was reportedly poor. Despite extensive evaluations, her condition remained undiagnosed, with recurring infections and inconclusive results from prior genetic and gastrointestinal assessments. Notably, no imaging studies had been conducted during the earlier diagnostic investigations.
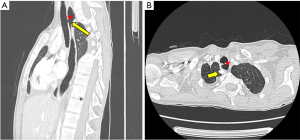
The girl was admitted to the pediatric intensive care unit (PICU) due to severe respiratory distress and acute respiratory failure. In the context of her prolonged history of recurrent respiratory tract infections, failure to thrive, and the lack of a definitive diagnosis despite multiple prior evaluations, the sudden worsening of her respiratory status raised clinical suspicion for a congenital structural anomaly. This prompted a contrast-enhanced chest computed tomography (CT) scan, which revealed the presence of H-type TEF. The anatomical evaluation showed that the fistula was located at the cervicothoracic junction, accompanied by complex structural abnormalities, including an aberrant right subclavian artery, a T4 hemivertebra contributing to scoliosis, partial schisis of the T6 vertebra, and a bronchial anomaly with lingular branches originating from the lower left bronchial division. These findings were further confirmed by preoperative imaging, providing essential guidance for surgical planning (Figure 1). These anomalies likely exacerbated her respiratory and gastrointestinal symptoms, contributing to the delayed diagnosis.
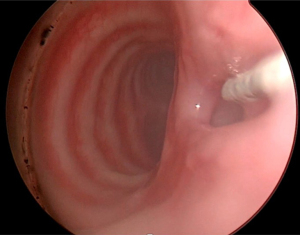
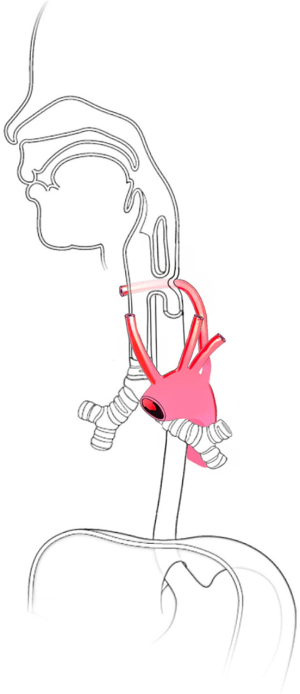
A surgical procedure was, therefore, planned to correct the congenital anomaly. The procedure began with preparatory laryngo-tracheo-bronchoscopy and esophagoscopy. Under tracheoscopy, the H-type TEF was identified and cannulated using a 4 Fr ureteral catheter (Figure 2). During esophagoscopy, the ureteral catheter passed through the mouth was carefully retracted to form a loop, enabling precise identification and management of the fistula during dissection. These steps allowed for accurate localization and manipulation of the TEF before proceeding with the primary surgical repair, which was performed through a cervical approach. The surgical correction of the TEF was performed via a right cervicotomy. After identifying the right jugular vein, the common carotid artery was isolated. Notably, the artery was displaced significantly to the right, crossing near the midline and positioned approximately 3 cm away from the vein. Severe scoliosis of the cervicothoracic spine further complicated the surgical field by distorting usual anatomical landmarks. Identifying the vagus nerve was also challenging due to an aberrant subclavian artery, which coursed posterior to the esophagus and caused significant displacement of the normal vascular anatomy in the neck (Figure 3). The dissection required sectioning of the medial head of the sternocleidomastoid muscle to identify the appropriate surgical plane and isolate the fistula. Dense scar tissue, likely due to recurrent inflammation, encased the trachea and esophagus, necessitating meticulous dissection. The presence of the catheter confirmed the successful isolation of the fistula, which was then completed with precise separation of the trachea and esophagus.
An esophagoscopy second-look examination verified the defect’s complete isolation. The tracheal and esophageal defects were sutured using absorbable sutures [i.e., polydioxanone suture (PDS)], and the tracheal suture was reinforced with a muscle layer. A hydropneumatic test confirmed the absence of leakage.
A critical step in ensuring surgical success was applying TachoSil®, a fibrinogen-thrombin-coated patch. This was layered three times over the suture lines to provide robust sealing and hemostasis, minimizing the risk of postoperative air leaks and bleeding (Figure 4). Given the extensive scarring and altered anatomy, this approach was essential. A lamellar drain was positioned near the anastomosis to monitor for complications, such as bleeding or leaks.
A prolonged inflammatory response initially complicated the patient’s postoperative course. However, respiratory and hemodynamic stability were achieved shortly after surgery. Follow-up imaging, including an upper gastrointestinal (GI) contrast study at 2 weeks, confirmed successful closure without leakage. The patient was discharged after 10 days and entered a multidisciplinary follow-up program involving pulmonology, gastroenterology, and pediatric surgery. The patient resumed normal physical activities and returned to school within 4 weeks. No respiratory support was required post-discharge, and pulmonary function improved steadily. At 6-month follow-up, she remained asymptomatic with no evidence of recurrence, stenosis, or dysphagia.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s), and with the Declaration of Helsinki and its subsequent amendments. According to Buzzi Children’s Hospital’s regulations (i.e., Department of Pediatric Surgery, Buzzi Children’s Hospital, 20154 Milan, Italy), the need for ethics approval for this non-interventional study’s retrospectively obtained and anonymized data was waived. The reservedness of the collected information was ensured according to Regulation (EU)/2016/679 GDPR, Legislative Decree n.101/18. Full informed consent was obtained from the study participant’s guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
H-type TEFs are typically congenital anomalies that arise from incomplete separation of the trachea and esophagus during embryonic development (1). As seen in our patient, this condition can lead to severe respiratory issues, aspiration, and repeated infections (4). The delayed diagnosis was partly due to the nonspecific symptoms, including recurrent respiratory infections and poor growth, which masked the underlying pathology (5). Few cases in the literature involve misdiagnosed H-type TEF (6), and identifying the congenital defect can be challenging (7). In addition, a delayed diagnosis increases the risk of chronic pulmonary complications and nutritional deficits. While recurrence is rare after complete resection, long-term follow-up is essential. Studies such as those by Zani et al. (5) report low recurrence but emphasize the need for structured surveillance to detect late sequelae (5-7).
This case highlights the diagnostic challenges and management complexities of H-type TEF in the context of congenital malformation syndrome. The patient’s presentation with recurrent respiratory infections and GERD masked the underlying pathology, resulting in years of symptomatic treatment without a definitive diagnosis. This delayed recognition is uncommon in isolated H-type TEF cases, mainly when symptoms are subtle or attributed to more common conditions such as asthma or reflux.
The malformation complex, including an aberrant right subclavian artery (arteria lusoria), skeletal anomalies, and bronchial variants, significantly complicated both diagnosis and surgical management. The aberrant right subclavian artery, with its retroesophageal course, increased esophageal compression and limited esophageal mobility, requiring meticulous dissection to avoid vascular injury. The presence of a T4 hemivertebra caused cervicothoracic scoliosis, which distorted the usual mediastinal and cervical anatomical landmarks. This abnormal curvature displaced critical vascular structures, including the common carotid artery and jugular vein, necessitating deviation from standard surgical planes and increasing the difficulty of safely isolating the fistula. In addition, a bronchial branching anomaly, where the lingular branches originated from the lower division of the left main bronchus, complicated endoscopic localization of the fistula during bronchoscopy. These anatomical variations collectively required a highly individualized surgical strategy, incorporating both open and endoscopic techniques to achieve accurate fistula identification and secure closure.
Surgical management of H-type TEF in the presence of chronic inflammation and fibrosis presents a unique challenge (7). Chronic inflammation from recurrent infections creates a hostile surgical environment, with fragile tissues that are prone to air leaks, bleeding, and other complications.
The successful outcome, in this case, was supported using TachoSil® as an adjunct to standard surgical techniques, including two-layer closure and muscle buttressing in the surgical management of H-type TEF. TachoSil® is a fibrinogen-thrombin-coated patch that is highly effective in achieving hemostasis and reinforcing surgical repairs. In this patient, TachoSil® was applied to the trachea and esophagus suture lines to ensure a secure seal of tissues seriously involved in chronic inflammation.
The pathology of H-type TEF often involves significant inflammation and fibrosis around the fistula, which can complicate surgical repair (8). The presence of scar tissue and adhesions makes the dissection challenging and increases the risk of intraoperative bleeding and the extension of the surgical resection (4). TachoSil® provided a valuable advantage by enhancing tissue adhesion and offering immediate hemostasis, allowing for a more secure and durable repair (9) and reducing the postoperative risk of air leaks, fistula recurrence, or hemorrhage (2,10). This application is critical in pediatric patients, where tissue fragility is a significant concern (3).
As demonstrated in various thoracic and abdominal surgeries (2), TachoSil® can reduce postoperative complications related to air leaks and hemorrhage (9). In pediatric patients with congenital malformations, like H-type TEF, ensuring secure sealing of sutures is essential due to the friable and inflamed nature of the tissues involved (3). Experiences reported in similar studies, such as those published by Filosso et al. (2), Marano & Di Martino (9), and Rickenbacher et al. (3), highlight TachoSil®’s effectiveness in reducing surgical morbidity by enhancing tissue adhesion and ensuring hemostasis (5,7).
In the study published by Filosso et al. (2) in 2013, TachoSil® was shown to significantly reduce the duration of air leaks and the length of hospital stay in 96 patients (60.4±10.3 years) undergoing redo surgery for lung malignancies. Similarly, Marano & Di Martino (9), in their 2016 study, demonstrated that TachoSil® effectively reduced the intensity and duration of postoperative air leaks in 13 patients undergoing lobectomy (62.5±13.6 years; range, 37–77 years). The use of TachoSil® in pediatric surgery has also been supported by Rickenbacher et al. (3) in 2009, who reported successful outcomes in controlling bleeding during complex surgeries. This underscores the importance of having a dependable hemostatic agent, particularly in pediatric patients where tissue fragility and inflammation pose additional challenges (10). These findings align with our experience using TachoSil® for H-type TEF repair. While TachoSil® is not superior to other adjuncts such as muscle flaps (11) or fibrin glue (12-14), its successful application in this case underscores its utility as a safe and effective reinforcement in complex, inflamed tissue environments.
Various surgical materials, including cyanoacrylate adhesives, collagen-based patches, and biologic meshes (12-15), are available to reinforce suture lines in high-risk repairs. However, these alternatives often lack the dual function of hemostasis and tissue sealing. In this context, TachoSil® was preferred for its ease of application, rapid activation upon contact with moist tissue, and proven efficacy in both thoracic and gastrointestinal procedures. Its application provided a secure reinforcement over inflamed and friable tissues, which was particularly valuable in this pediatric patient.
Conclusions
This case highlights the importance of recognizing tissue damage caused by chronic inflammation in cases of delayed diagnosis of isolated congenital H-type TEF. Pediatric surgeons can significantly improve patient outcomes with fragile tissues by utilizing advanced techniques. The recurrence of H-type TEF is rare when the fistula is completely excised and securely repaired; long-term follow-up remains essential. Our patient showed no recurrence at the 6-month follow-up, consistent with literature indicating low recurrence rates after primary closure. While not central to the repair, the use of TachoSil® complemented standard techniques by helping reinforce the suture lines and may have contributed to reduced postoperative complications in this complex inflammatory setting.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-72/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-72/prf
Funding: This study was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-72/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s), and with the Declaration of Helsinki and its subsequent amendments. According to Buzzi Children’s Hospital’s regulations (i.e., Department of Pediatric Surgery, Buzzi Children’s Hospital, 20154 Milan, Italy), the need for ethics approval for this non-interventional study’s retrospectively obtained and anonymized data was waived. The reservedness of the collected information was ensured according to Regulation (EU)/2016/679 GDPR, Legislative Decree n.101/18. Full informed consent was obtained from the study participant’s guardians for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fallon SC, Langer JC, St Peter SD, et al. Congenital H-type tracheoesophageal fistula: A multicenter review of outcomes in a rare disease. J Pediatr Surg 2017;52:1711-4. [Crossref] [PubMed]
- Filosso PL, Ruffini E, Sandri A, et al. Efficacy and safety of human fibrinogen-thrombin patch (TachoSil®) in the treatment of postoperative air leakage in patients submitted to redo surgery for lung malignancies: a randomized trial. Interact Cardiovasc Thorac Surg 2013;16:661-6. [Crossref] [PubMed]
- Rickenbacher A, Breitenstein S, Lesurtel M, et al. Efficacy of TachoSil a fibrin-based haemostat in different fields of surgery--a systematic review. Expert Opin Biol Ther 2009;9:897-907. [Crossref] [PubMed]
- Taghavi K, Tan Tanny SP, Hawley A, et al. H-type congenital tracheoesophageal fistula: Insights from 70 years of The Royal Children's Hospital experience. J Pediatr Surg 2021;56:686-91. [Crossref] [PubMed]
- Zani A, Jamal L, Cobellis G, et al. Long-term outcomes following H-type tracheoesophageal fistula repair in infants. Pediatr Surg Int 2017;33:187-90. [Crossref] [PubMed]
- Więckowski PR, Łysak JM, Maciejewski IZ, et al. A Cautionary Tale: Undetected H-type Tracheoesophageal Fistula in an Adolescent Male. Cureus 2024;16:e57647. [Crossref] [PubMed]
- Morchio C, Ganarin A, Conforti A, et al. Diagnosis and Management of Congenital H-Type Tracheoesophageal Fistula: Results of a National Survey. Children (Basel) 2024;11:423. [Crossref] [PubMed]
- Bibas BJ, Cardoso PFG, Minamoto H, et al. Surgery for intrathoracic tracheoesophageal and bronchoesophageal fistula. Ann Transl Med 2018;6:210. [Crossref] [PubMed]
- Marano L, Di Martino N. Efficacy of Human Fibrinogen-Thrombin Patch (TachoSil) Clinical Application in Upper Gastrointestinal Cancer Surgery. J Invest Surg 2016;29:352-8. [Crossref] [PubMed]
- Pelizzo G, Arbustini E, Pasqua N, et al. Thoracoscopic Treatment of Pneumothorax in Marfan Syndrome: Hemostatic Patch to Support Lung Resection Recovery. Case Rep Surg 2018;2018:7597215. [Crossref] [PubMed]
- Suzuki T, Narisawa T, Tanaka H, et al. Closure of a cervical H-type tracheoesophageal fistula. Thorac Cardiovasc Surg 2004;52:57-9. [Crossref] [PubMed]
- Upadhyaya VD, Gopal SC, Gangopadhyaya AN, et al. Role of fibrin glue as a sealant to esophageal anastomosis in cases of congenital esophageal atresia with tracheoesophageal fistula. World J Surg 2007;31:2412-5. [Crossref] [PubMed]
- Lao VV, Lustig D, Boseley M, et al. Pediatric ingested foreign body, acquired tracheoesophageal fistula – Endoscopic repair with cautery & fibrin glue (Tisseel): Case report and literature review. Journal of Pediatric Surgery Case Reports 2015;3:426-31.
- Tzifa KT, Maxwell EL, Chait P, et al. Endoscopic treatment of congenital H-Type and recurrent tracheoesophageal fistula with electrocautery and histoacryl glue. Int J Pediatr Otorhinolaryngol 2006;70:925-30. [Crossref] [PubMed]
- Tomasicchio G, Martines G, Tartaglia N, et al. Suture reinforcement using a modified cyanoacrylate glue to prevent anastomotic leak in colorectal surgery: a prospective multicentre randomized trial : The Rectal Anastomotic seaL (ReAL) trial. Tech Coloproctol 2024;28:95. [Crossref] [PubMed]



