
A new modified endoscopic evaluation system and its diagnostic accuracy of adenoid hypertrophy in children
Highlight box
Key findings
• A novel, modified evaluation system was introduced to investigate the correlation between adenoid hypertrophy and obstructive sleep apnea, including ear complications. Which enables a more accurate quantitative evaluation of adenoid hypertrophy during adenoid endoscopy, showing potential for improved diagnosis of progressive otitis media.
What is known and what is new?
• In recent years, nasopharyngeal endoscopy has been widely used in clinical practice. Currently, three methods are commonly used to assess the size of the adenoid: percentage of 4-grade system, Parikh’s grading system, and the airway/choana/eustachian tube (ACE) grading system.
• We introduced an improved anatomical adjacent 5-grade system (modified from Parikh’s grading system) that facilitates a finer categorization of extrusion between the adenoid and the pharyngeal orifice of the eustachian tube.
What is the implication, and what should change now?
• The anatomical adjacent of 5-grade system may be a promising tool for improving the detection of adenoid hypertrophy and monitoring the progression of otitis media. The 5-grade anatomical adjacency system should be widely applied in clinical examinations.
Introduction
Sleep-disordered breathing (SDB) can be divided into five categories: obstructive sleep apnea (OSA) and central sleep apnea, sleep-related hypopnea, sleep-related hypoxemia, sleep correlation isolated symptoms and normal variation (1). One of the most significant detrimental effects is OSA, characterized by nocturnal snoring accompanied by episodes of apnea and excessive daytime sleepiness. Due to airway collapse, recurrent hypoxemia, hypercapnia, and sleep structure disorders are commonly observed during the night. Adenoid hypertrophy is one of the main causes of airway obstruction in children and adolescents (2), which is primarily caused by recurrent infections or chronic inflammation, sometimes combined with tonsillar hypertrophy, occupying the narrow upper airway space, cause airway obstruction during sleep, leading to OSA. The reported prevalence rate of adenoid hypertrophy is up to 34% (3). Adenoidectomy has emerged as the most efficacious treatment modality for pediatric OSA associated with adenoid hypertrophy, underscoring the imperative need for accurate diagnosis in affected children (4).
In recent years, nasopharyngeal endoscopy has been widely used in clinical practice. Compared to imaging examinations, the flexible nasopharyngoscopy offers certain advantages, it has no radiation hazards and can detect whether there is any purulent secretion irritating the nasopharyngeal. Moreover, it is more conducive to observing the area near the pharyngeal orifice of the eustachian tube. Currently, the following three methods are commonly used to assess the size of the adenoid: percentage of 4-grade system (5), Parikh’s grading system (6), and the airway/choana/eustachian tube (ACE) grading system (7,8).
Previously, we introduced an improved anatomical adjacent 5-grade system (modified from Parikh’s grading system) that facilitates a finer categorization of extrusion between the adenoid and the pharyngeal orifice of the eustachian tube (8). However, the classification standard for adenoid hypertrophy is not unified (9) as there is no large sample prospective clinical study that has provided diagnostic performance data across the commonly used endoscopic adenoid classification systems. The objective of the present study was to investigate the association between adenoid hypertrophy and OSA and ear complication such as secretory otitis media (10) as standard protocols. Analysis of different endoscopic evaluation systems, including the percentage of 4-grade system, Parikh’s grading system, ACE grading system and our anatomical adjacent of 5-grade system (modified Parikh’s grading system), was executed to evaluate and compare the diagnostic efficacy for adenoid hypertrophy, surgical intervention, and prognostic accuracy for associated ear complications. We present this article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-189/rc).
Methods
Clinical data
The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. This study was examined and approved by the Ethics Committee of Shanghai Children’s Hospital (No. 2022R153-E01) and posted on the website of China Clinical Trial Center (https://www.chictr.org.cn) under the registration No. ChiCTR2300068424. Informed consent was obtained from all subjects and/or their legal guardians. This study was a prospective, single-center, observational study. All methods were carried out in accordance with relevant guidelines and regulations.
A total of 184 children with varying degrees of sleep snoring and/or mouth breathing were recruited from the outpatient Department of Otorhinolaryngology Head and Neck Surgery, Shanghai Children’s Hospital from January 2023 to December 2023. All children underwent flexible electronic nasopharyngoscopy within 24 hours of enrollment. After surface anesthesia of the nasal cavity, the children were in supine position and accompanied by their parents. For children who cannot cooperate perfectly, parents and nurses assisted in immobilizing their shoulders and heads. The doctor stood at the head of the children to perform flexible electronic nasopharyngoscopy, and the examination processes were as gentle as possible. Adenoid grade under endoscopy was recorded by percentage of 4-grade system, Parikh’s grading system, ACE grading system and the modified Parikh’s grading system. Participants were followed up for 6 months in the outpatient department or until occurrence of the primary endpoint event. Adenoidectomy was indicated based on the Chinese guidelines for the diagnosis and treatment of OSA in children (2020), the diagnosis and treatment for secretory otitis media was indicated based on the Guidelines for the Diagnosis and Treatment of Secretory Otitis Media in Children (2021).
Inclusion and exclusion criteria
Inclusion criteria: (I) patients aged 0 to 14 years old; (II) the clinical symptoms suggest adenoid hypertrophy (including symptoms of OSA such as snoring, mouth breathing, apnea, and adenoid facies); (III) no contraindications for undergoing adenoidectomy or secretory otitis media surgery; (IV) no contraindications for undergoing flexible electronic nasopharyngoscopy examination.
Exclusion criteria: (I) patients aged over 15 years old; (II) Children who have undergone adenoidectomy surgery; (III) children who require direct surgical treatment and do not need follow-up; (IV) have contraindications for undergoing adenoidectomy or secretory otitis media surgery; (V) have contraindications for undergoing flexible electronic nasopharyngoscopy examination; (VI) combine severe systemic diseases; (VII) unable to obtain the informed consent.
Measurement methods
Percentage of 4-grade system (5)
Adenoid hypertrophy was classified into four grades according to the relationship between soft palate and adenoid: grade I: 0–25%, hyperplasia of lymphoid tissue in nasopharynx; grade II: 25–50%, half of the upper area blocked in nasopharynx; grade III: 50–75%, the upper area completely blocked in nasopharynx; grade IV: >75%, the adenoid almost complete blocked in nasopharynx. Among them, grade III and grade IV were considered clinically pathological obstructions. In this study, the grade of adenoid hypertrophy was independently evaluated by five pediatric otolaryngology head and neck surgeons and subsequently averaged.
Parikh’s grading system (6)
According to the anatomical relationship between adenoid and pharyngeal orifice of the eustachian tube, posterior edge of vomer bone and soft palate (during inspiration), a 4-grade system was used. Grade I was indicated by the absence of contact of the adenoid with any adjacent structures, grade II was indicated by contact with the pharyngeal orifice of the eustachian tube, grade III was indicated by contact with the pharyngeal orifice of the eustachian tube and vomer bone, and grade IV was indicated by contact with all of the adjacent structures. In this study, the grades were independently evaluated by five pediatric otolaryngology head and neck surgeons and subsequently averaged.
ACE grading system (7)
“A” was graded from 0 to 4 according to the percentage of adenoid obstructions in the posterior nostril. “C” was graded from 0 to 2 according to the relationship between the adenoid and vomer. “E” was graded from 0 to 1 according to the degree of congestion of the pharyngeal orifice of the eustachian tube. The maximum possible score is A4C2E1. In this study, the grades were independently evaluated by five pediatric otolaryngology head and neck surgeons and subsequently averaged.
Anatomical adjacent of 5-grade system (modified Parikh’s grading system)
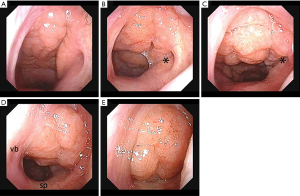
A modified Parikh’s grading system was evaluated, according to the anatomical relationship between the adenoid and the pharyngeal orifice of the eustachian tube, posterior edge of vomer bone and soft palate (during inspiration) (Figure 1). Grade I was indicated when the adenoid had no contact with any of the adjacent structures, grade II was indicated when the adenoid exhibited contact but did not extrude the pharyngeal orifice of the eustachian tube, grade III was indicated when the adenoid contacted and extruded the pharyngeal orifice of the eustachian tube, grade IV was indicated when the adenoid exhibited contact with the vomer bone or with the pharyngeal orifice of the eustachian tube and vomer bone, and grade V was indicated when the adenoid made contact with all adjacent structures. The grades were independently evaluated by five pediatric otolaryngology head and neck surgeons and subsequently averaged. There are differences between different grading systems (Figure 2).

Reference standard for adenoidectomy
The reference standard for adenoidectomy in this study was mainly determined by the Chinese guidelines for the diagnosis and treatment of OSA in children (2020) (5) and the American Academy of Pediatrics: Clinical practice guideline for the Diagnosis and Management of Childhood Obstructive (2012) (11). Adenoidectomy was considered in cases of pathological adenoid hypertrophy accompanied by a constellation of clinical symptoms indicative of hypoxia, such as sleep snoring, breathlessness, apnea, open mouth breathing, labile breathing, restless sleep, repeated awakenings, daytime sleepiness, attention deficit or hyperactivity, decreased academic performance, particularly when conservative pharmacological treatment had proven ineffective. According to the Percentage of 4-grade system, Parikh’s grading system (12), and the anatomical adjacent of 5-grade system, grades III and IV were considered clinically pathological obstruction. In the ACE grading system, the adenoid was considered clinically pathological when A=3 or 4.
Statistical analysis
SPSS 25.0 software was used for statistical analysis. The receiver operating characteristic (ROC) curves of all grading systems were analyzed, and the area under the curve (AUC) was calculated. MedCalc 19.0.4 was used to compare the AUC of the four grading systems by DeLong model, and the best cut-off value of the systems was determined by Youden index in ROC analysis. The sensitivity and specificity of the cutoff values of these four grading systems were calculated, and the negative predictive value, positive predictive value and accuracy were further calculated. McNemar test was used to compare the accuracy, sensitivity, specificity and other diagnostic efficacy of the four grading systems.
Results
Out of the total 184 cases, 19 were lost to follow-up, while the remaining 165 cases were successfully tracked to completion. Participant characteristics included 89 males, 76 females, the age ranged from 2 years and 2 months to 13 years, median age 6.30±2.68 years old, height 123±17 cm, weight 27.70±11.6 kg. Seventy-nine cases (47.88%) were in accordance with the surgical indications for adenoidectomy. Forty-six cases (27.88%) developed secretory otitis media or aggravated secretory otitis media during the follow-up period. Specific conditions of adenoidal hypertrophy assessed within different grading systems are shown in Table 1.
Table 1
| Grading systems | Levels | Number of cases | Adenoidectomy cases | Secretory otitis media cases |
|---|---|---|---|---|
| Percentage of 4-grade system | I | 7 | 1 | 1 |
| II | 15 | 1 | 4 | |
| III | 44 | 21 | 12 | |
| IV | 99 | 56 | 29 | |
| Parikh’s grading system | I | 1 | 0 | 0 |
| II | 11 | 4 | 4 | |
| III | 91 | 36 | 30 | |
| IV | 62 | 39 | 12 | |
| ACE grading system | A1C0E0 | 7 | 1 | 1 |
| A2C0E0 | 2 | 0 | 1 | |
| A2C1E0 | 4 | 0 | 2 | |
| A2C1E1 | 2 | 0 | 1 | |
| A2C2E0 | 4 | 1 | 0 | |
| A2C2E1 | 3 | 0 | 0 | |
| A3C2E0 | 4 | 2 | 2 | |
| A3C2E1 | 40 | 19 | 10 | |
| A4C2E1 | 99 | 56 | 29 | |
| Anatomical adjacent of 5-grade system | I | 1 | 0 | 0 |
| II | 7 | 2 | 2 | |
| III | 5 | 0 | 0 | |
| IV | 79 | 26 | 17 | |
| V | 73 | 51 | 27 |
ACE, airway/choana/eustachian tube.
Surgical indications for adenoidectomy and secretory otitis media were considered by reference standards as previously described. The severity of adenoid hypertrophy in 165 children was scored by the percentage of 4-grade system, Parikh’s grading system, ACE grading system and modified Parikh’s grading system. The ROC curves were analyzed, and the AUC was calculated.
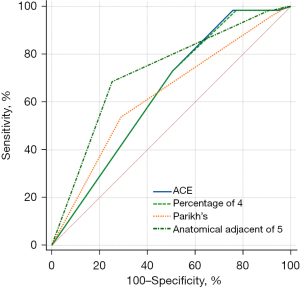
With surgical indications determined by reference standards, ACE grading system displayed the highest sensitivity, while the anatomical adjacent of 5-grade system (modified Parikh’s grading system) demonstrated the highest specificity, accuracy and AUC. The diagnostic efficiency of the anatomical adjacent of 5-grade system in determining whether OSA in children required surgical intervention was significantly different from the percentage of 4-grade system and Parikh’s grading system (P<0.05) (Tables 2,3, Figure 3).
Table 2
| Measurement methods | Sensitivity, % | Specificity, % | Accuracy, % | AUC (95% CI) |
|---|---|---|---|---|
| Percentage of 4-grade system | 73.134 | 49.367 | 60.274 | 0.638 (0.555–0.716) |
| Parikh’s grading system | 53.731 | 70.886 | 63.014 | 0.628 (0.544–0.706) |
| ACE grading system | 98.507 | 24.051 | 58.219 | 0.640 (0.556–0.717) |
| Anatomical adjacent of 5-grade system | 68.657 | 74.684 | 71.918 | 0.725 (0.645–0.796) |
ACE, airway/choana/eustachian tube; AUC, area under the curve; CI, confidence interval.
Table 3
| Measurement methods | Parikh’s grading system | ACE grading system | Anatomical adjacent of 5-grade system |
|---|---|---|---|
| Percentage of 4-grade system | P=0.83 | P=0.36 | P=0.048 |
| Parikh’s grading system | NA | P=0.80 | P=0.004 |
| ACE grading system | – | NA | P=0.053 |
ACE, airway/choana/eustachian tube; NA, not applicable; ROC, receiver operating characteristic.
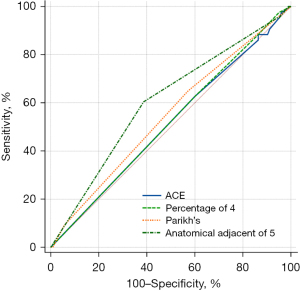
With secretory otitis media as the reference standard, all endoscopic grading systems exhibited generally similar AUC. After introducing the anatomical adjacent of 5-grade system for evaluation, the sensitivity, specificity, accuracy and AUC were all increased, but there was no significant difference between Parikh’s grading system (P=0.49) (Tables 4,5, Figure 4).
Table 4
| Measurement methods | Sensitivity, % | Specificity, % | Accuracy, % | AUC (95% CI) |
|---|---|---|---|---|
| Percentage of 4-grade system | 62.791 | 39.806 | 46.575 | 0.516 (0.432–0.600) |
| Parikh’s grading system | 34.884 | 57.282 | 50.685 | 0.546 (0.462–0.629) |
| ACE grading system | 62.791 | 39.806 | 46.575 | 0.511 (0.427–0.594) |
| Anatomical adjacent of 5-grade system | 60.465 | 61.165 | 60.959 | 0.605 (0.521–0.685) |
ACE, airway/choana/eustachian tube; AUC, area under the curve; CI, confidence interval.
Table 5
| Measurement methods | Parikh’s grading system | ACE grading system | Anatomical adjacent of 5-grade system |
|---|---|---|---|
| Percentage of 4-grade system | P=0.69 | P=0.12 | P=0.09 |
| Parikh’s grading system | NA | P=0.64 | P=0.49 |
| ACE grading system | – | NA | P=0.07 |
ACE, airway/choana/eustachian tube; NA, not applicable; ROC, receiver operating characteristic.
Discussion
Children between the ages of 2 and 6 years exhibit robust adenoid development, which can easily lead to eustachian tube and nasopharyngeal cavity blockage due to limited nasal space. Consequently, a range of local symptoms such as nasal obstruction and secretory otitis media may arise. The indication for adenoidectomy is considered when the adenoid exhibits pathological hypertrophy accompanied by prominent clinical symptoms such as hypoxia (13). The selection of surgical indications should be based on the severity of adenoid hypertrophy prior to surgery. Therefore, a precise preoperative examination is imperative for accurate evaluation of adenoid condition.
At present, the most commonly used imaging methods in clinical practice are lateral X-ray and CT examination of the nasopharynx. Nasopharyngeal lateral slice density resolution is low and susceptible to image overlap, making it difficult to distinguish the border of adenoid, the anatomical marks of the sphenooccipital junction, and the soft and hard palate junction (14). Nasopharyngeal CT scan and lateral X-ray also present risks of radiation exposure. Compared to imaging examinations, nasopharyngeal endoscopy offers several advantages. It allows for dynamic observation of adenoid size from multiple angles and enables the detection of repeated stimulation of the nasopharynx by mucopurulent discharge. For children with recurrent secretory otitis media, this examination is particularly useful in assessing whether there is extrusion of the adenoids on the round occipital part of the eustachian tube, and determining its degree of extrusion. Although nasopharyngoscopy is an invasive examination, the use of small diameter soft scope in the hands of a skilled operator, generally does not cause damage to the children and eliminates the hazards of radiation exposure.
Study has shown that (15) in comparison with imaging examinations, nasopharyngeal endoscopy remains the golden standard for evaluating adenoid hypertrophy in children. During routine inspections, it is recommended to utilize nasopharyngeal endoscopy for accurate diagnosis of the extent of hypertrophy and subsequent appropriate treatment. The method used in the Chinese guidelines for the diagnosis and treatment of OSA in children (2020) (5) is the percentage of 4-grade system, which is mainly graded by the volume of adenoids relative to the nasopharyngeal cavity. Despite being simple, rapid, intuitive, and easy to comprehend, the grading system falls short in accurately capturing the compression and obstruction of adjacent tissues that result from adenoid hypertrophy. The available clinical evidence suggests that a mere assessment of adenoid volume may not adequately reflect the true severity of the disease or provide sufficient guidance for intervention measures (16). In clinical practice, we have observed that some children classified as having III or IV grade adenoid hypertrophy according to the percentage of 4-grade system do not exhibit clinical manifestations severe enough to necessitate adenoidectomy. Therefore, there is a need to update the endoscopic adenoid evaluation system to align with the demands of practical clinical work and to offer a more comprehensive assessment of adenoid hypertrophy-related conditions.
Parikh et al. (6) also proposed a 4-grade classification system based on the anatomical relationship between adenoids and the pharyngeal orifice of the eustachian tube, vomer bone and soft palate (during inspiration). Varghese et al. (7) proposed the ACE grading system based on Parikh’s grading system, though accounting for congestion of the pharyngeal orifice of the eustachian tube. In recent years, Parikh’s grading system has been widely used in North America, Europe and some Latin American countries (17-20). However, there remains a lack of large sample clinical data to support the efficacy of the associated grading systems in predicting the prognosis and intervention of OSA in children. In previous clinical works, clinical experience suggests that Parikh’s grading system may not accurately delineate the extent of extrusion between the adenoids and the pharyngeal orifice of the Eustachian tube. When adenoids exert pressure on the pharyngeal orifice of the eustachian tube, it may be more likely to result in secretory otitis media and subsequent hearing impairment. Therefore, elucidating the correlation between the adenoids and the pharyngeal orifice of the Eustachian tube is of paramount importance.
As depicted in Figure 2, when graded by percentage of 4-grade system, d and e were Grade IV (>75%) but were classified as A4C2E1 (A: 76% to 100%, C: >50% block, E: abutting ET) by the ACE grading system. Although it can be observed that there was a variation in the size of adenoids between d and e; when graded by Parikh’s grading system, b and c were Grade II (adenoid contact with the pharyngeal orifice of the eustachian tube) but the adenoid in c exerted pressure on the pharyngeal orifice of the eustachian tube. We believed that a reasonable grading system should reflect the compression and obstruction of adjacent anatomic structures around the adenoids, including the pharyngeal orifice of the eustachian tube. Combining the advantages of Parikh’s grading system and ACE grading system, we modified Parikh’s grading system and introduced the 5-degree grading method.
A total of 184 subjects were prospectively enrolled in this study, and 165 subjects completed follow up. The surgical indications for adenoidectomy and secretory otitis media were used as the reference standards. The severity of adenoid hypertrophy under endoscopy was scored by percentage of 4-grade system, Parikh’s grading system, ACE grading system and a modified Parikh’s grading system. To ensure inter-rater reliability, the grades were independently evaluated by five pediatric otolaryngology head and neck surgeons and subsequently averaged. The sensitivity, specificity, accuracy and area under the ROC curve were compared between each grading method.
Among the currently used endoscopic grading systems for adenoid hypertrophy for evaluation of children with OSA, the ACE grading system exhibited the highest sensitivity and AUC, while Parikh’s grading system exhibited the highest specificity and accuracy. Parikh’s grading system and the ACE grading system performed better than the percentage of 4-grade system to some extent, though without statistical difference. After introducing the modified Parikh’s grading system for evaluation, sensitivity was improved while the specificity, accuracy and AUC were the highest. The diagnostic efficiency of the modified Parikh’s grading system in determining whether OSA in children requires surgical intervention was superior than either the Percentage of 4-grade system and Parikh’s grading system (P<0.05). Although there was no statistical difference (P=0.053), the diagnostic efficiency of the modified Parikh’s grading system for OSA demonstrated certain improvements compared with the ACE grading system (the AUC was higher).
In this group of data, when judging the occurrence and progression of secretory otitis media in children with the currently used adenoid endoscopic grading systems, the AUC of Parikh’s grading system was slightly higher than percentage of 4-grade system and ACE grading system. However, they were generally similar. After introducing the modified Parikh’s grading system for evaluation, the sensitivity, specificity, accuracy and AUC were all increased, but there was no significant difference between Parikh’s grading system (P=0.49). Although there was no statistical difference, the diagnostic efficiency of the modified Parikh’s grading system for secretory otitis media in children demonstrated certain improvements compared with the percentage of 4-grade system and the ACE grading system (P is close to 0.05).
One of the limitations of the present study is that data were taken from a single center. In the future, uniform and rigorous criteria should be used to conduct large sample, multi-center studies to verify the diagnostic efficacy of the anatomical adjacent of 5-grade system.
Conclusions
The anatomical adjacent of 5-grade system (modified Parikh’s grading system) evaluated the severity of adenoid hypertrophy more accurately via endoscopic analysis. Due to the relationship between the adenoids and the eustachian tube (the development and progression of otitis media), the anatomical adjacent of 5-grade system may be a promising tool for improving the detection of adenoid hypertrophy and monitoring the progression of otitis media.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-189/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-189/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-189/prf
Funding: This study was partially supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-189/coif). All authors report that this study was partially supported by the National Natural Science Foundation of China (No. 82171121). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. This study was examined and approved by the Ethics Committee of Shanghai Children’s Hospital (No. 2022R153-E01) and posted on the website of China Clinical Trial Center (https://www.chictr.org.cn) under the registration No. ChiCTR2300068424. Informed consent was obtained from all subjects and/or their legal guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sateia MJ. International classification of sleep disorders-third edition: highlights and modifications. Chest 2014;146:1387-94.
- Kuhle S, Hoffmann DU, Mitra S, et al. Anti-inflammatory medications for obstructive sleep apnoea in children. Cochrane Database Syst Rev 2020;1:CD007074.
- Pereira L, Monyror J, Almeida FT, et al. Prevalence of adenoid hypertrophy: A systematic review and meta-analysis. Sleep Med Rev 2018;38:101-112.
- Kang M, Mo F, Witmans M, et al. Trends in Diagnosing Obstructive Sleep Apnea in Pediatrics. Children (Basel) 2022;9:306.
- Working Group of Chinese Guideline for the Diagnosis and Treatment of Childhood OSA. Subspecialty Group of Respiratory Diseases, Society of Pediatrics, Chinese Medical Association; Society of Pediatric Surgery, Chinese Medical Association; Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery. Chinese guideline for the diagnosis and treatment of childhood obstructive sleep apnea (2020). Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2020;55:729-47.
- Parikh SR, Coronel M, Lee JJ, et al. Validation of a new grading system for endoscopic examination of adenoid hypertrophy. Otolaryngol Head Neck Surg 2006;135:684-7.
- Varghese AM, Naina P, Cheng AT, et al. ACE grading-A proposed endoscopic grading system for adenoids and its clinical correlation. Int J Pediatr Otorhinolaryngol 2016;83:155-9.
- Zhang MJ, Xu HM, Pu SL, et al. Evaluation and grading progression of adenoid hypertrophy in children. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2023;58:188-92.
- Patel A, Brook CD, Levi JR. Comparison of adenoid assessment by flexible endoscopy and mirror exam. Int J Pediatr Otorhinolaryngol 2020;134:110073.
- Editorial Board of Chinese Journal of Otorhinolaryngology Head and Neck Surgery. Guideline for the diagnosis and treatment of otitis media with effusion in children (2021). Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2021;56:556-67.
- Marcus CL, Brooks LJ, Draper KA, et al. Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012;130:e714-55.
- Franco RA Jr, Rosenfeld RM, Rao M. First place--resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surg 2000;123:9-16.
- Ke X, Zhang R, Chen G. On the Diagnosis and Treatment Strategies for Secretory Otitis Media in Children with Adenoid Hypertrophy. Chinese Journal of Otology 2019;17:77-81.
- Fujioka M, Young LW, Girdany BR. Radiographic evaluation of adenoidal size in children: adenoidal-nasopharyngeal ratio. AJR Am J Roentgenol 1979;133:401-4.
- Sarma N, Khaund G. A Comparative Study of Radiograph and Nasal Endoscopy in Diagnosis of Hypertrophied Adenoids. Indian J Otolaryngol Head Neck Surg 2019;71:1793-5.
- Cassano P, Gelardi M, Cassano M, et al. Adenoid tissue rhinopharyngeal obstruction grading based on fiberendoscopic findings: a novel approach to therapeutic management. Int J Pediatr Otorhinolaryngol 2003;67:1303-9.
- Ciprandi G, Ameli F, Asmanov A, et al. Risk factors for recurrent acute otitis media: a real-life clinical experience. J Biol Regul Homeost Agents 2021;35:33-8.
- Leal MC, Seabra Ramos D, Pinto Bezerra T, et al. The Prevalence of Adenoid Hypertrophy among Children with Zika Related Microcephaly. Viruses 2021;13:62.
- Ameli F, Brocchetti F, Mignosi S, et al. Recurrent respiratory infections in children: a study in clinical practice. Acta Biomed 2020;91:e2020179.
- Ciprandi G, Tosca MA, Gallo F, et al. Turbinate hypertrophy in children with allergic rhinitis: clinical relevance. Acta Biomed 2020;91:43-7.


