
Global, regional, and national burden of neonatal infectious diseases from 1990 to 2021
Highlight box
Key findings
• The worldwide burden of neonatal infectious diseases has decreased over the past decades and is inversely related to socio-demographic index values.
What is known and what is new?
• Neonatal infectious diseases remain a critical public health challenge worldwide, contributing substantially to neonatal morbidity and mortality.
• The study provided a comprehensive analysis of the global, regional, and national burden of neonatal infectious diseases from 1990 to 2021.
What is the implication, and what should change now?
• Improving socio-economic levels and enhancing disease management are important in reducing the burden of neonatal infectious diseases.
Introduction
Neonatal infectious diseases, caused by bacterial, viral, or fungal pathogens, represent a major global health concern due to their significant morbidity and mortality rates among both term and preterm infants. Newborns are particularly vulnerable to infections due to their immature immune systems and underdeveloped barrier defenses. Pathogens can invade through multiple routes, including the skin, umbilical cord, conjunctiva, oropharynx, as well as gastrointestinal and respiratory tracts. Infants requiring prolonged hospitalization and advanced medical interventions, such as indwelling devices including intravenous lines, endotracheal tubes, urinary catheters, and shunts, are at an elevated risk of infection (1).
Severe systemic infections, classified as neonatal sepsis, can lead to life-threatening organ dysfunction and are the third leading cause of neonatal mortality, affecting 4 to 22 per 1,000 live births globally (2,3). Neonatal sepsis is categorized based on the timing of onset into early-onset sepsis (EOS) and late-onset sepsis (LOS). EOS typically manifests within the first 72 hours post-delivery, often resulting from vertical transmission from mother to infant, occurring either in utero or during delivery. In contrast, LOS arises from postnatal exposure to infectious agents within the community or hospital setting, typically emerging after 72 hours of life. Occasionally, pathogens acquired during delivery may only become symptomatic later (4,5).
Neonatal infectious diseases remain a critical public health challenge worldwide, contributing substantially to neonatal morbidity and mortality. Prior researches have indicated that the disease burden varies significantly across different regions. Low- and middle-income countries experience a disproportionately higher burden due to factors such as limited access to quality healthcare, inadequate sanitation, and higher rates of maternal infections (6,7). This study aims to elucidate the global, regional, and national trends in the incidence and disability-adjusted life years (DALYs) associated with neonatal infectious diseases from 1990 to 2021, stratifying these trends by sex, age, socio-demographic index (SDI), region, and country. We present this article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-57/rc).
Methods
Data source
The 2021 Global Burden of Disease (GBD) study, utilizing the latest epidemiological data and enhanced standardized methodologies, comprehensively assessed the health detriments associated with 369 diseases, injuries, and impairments, as well as 88 risk factors, encompassing 204 nations and territories (8). In this study, we extracted data on the incidence and DALYs for neonatal infectious disease from 1990 to 2021, categorized by country and region, using the Global Health Data Exchange Query Tool (http://ghdx.healthdata.org/gbd-results-tool). Regional and national stratification in this study was conducted based on the standard classification framework used by the GBD Study. Age-standardized rates (ASRs) were calculated based on the GBD global standard population to ensure comparability across regions and over time. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments.
Joinpoint regression analysis
The study employed the Joinpoint regression analysis model, a statistical methodology widely used in epidemiological research to assess temporal trends in disease. This model effectively identifies and quantitatively characterizes significant change points in temporal datasets related to neonatal infectious disease incidence and DALYs. The model facilitated the computation of the annual percentage change (APC) and average APC (AAPC), including their 95% confidence intervals (CIs). A log-linear model was specified, and the number of joinpoints was determined based on the Bayesian Information Criterion (BIC), allowing for a maximum of four joinpoints. Statistical significance of trend changes was tested using a Monte Carlo Permutation method, with a significance threshold set at P<0.05. The joinpoint model thus enabled identification of critical time points where significant shifts in disease trends occurred and provided a robust quantitative assessment of temporal patterns.
SDI
The SDI is a composite measure developed by researchers from the GBD study to assess the socio-economic development level of a country or region. It integrates three key indicators: lag-distributed income per capita, average years of schooling, and the fertility rate among females under age 25 years. Each component is rescaled using selected health indicators to a uniform scale ranging from 0 to 1. A higher SDI value indicates better socio-economic conditions and is generally associated with improved health outcomes. Based on SDI quintiles, countries are categorized into five levels of development: low, low-middle, middle, high-middle, and high SDI.
Statistics analysis
The main objective of this study was to estimate the global trends in neonatal infectious diseases incidence and DALYs. We stratified global trends by sex, age and reported regional and national trends. Rates in our projections were displayed/100,000 people.
The estimated APCs (EAPCs) were calculated to evaluate the annual average change in ASRs using a generalized linear regression model. This model characterizes the temporal dynamics of ASR by establishing a relationship between the natural logarithm (ln) of ASR and time through the equation: Y=αβX+ε. Here, Y represents ln (ASR), α is the intercept, X corresponds to the calendar year, ε denotes the error term, and β reflects a linear positive or negative trend in ASR. The EAPC and its 95% CI are computed using this formula: EAPC = 100 × [exp (β) − 1]. Trend significance is evaluated through 95% CIs, an upward trend is inferred when the lower CI boundary exceeded 0, while a downward trend is concluded if the upper CI boundary fell below 0. Trends are considered statistically non-significant when the 95% CI encompassed 0 (8).
All statistical analysis and graphical representations were conducted using R software (version 4.3.2) and the Joinpoint Regression Program (version 5.2.0).
Results
Global trends
Globally, the incidence cases of neonatal infectious diseases decreased from 4,654,910 [95% uncertainty interval (UI): 4,590,168 to 4,726,630] in 1990 to 3,634,421 (95% UI: 3,580,612 to 3,694,913) in 2021 and the rate decreased from 46,365.63 (95% UI: 45,720.76 to 47,080.01)/100,000 in 1990 to 37,294.43 (95% UI: 36,742.27 to 37,915.17)/100,000 in 2021, AAPC −0.71 (95% CI: −0.76 to −0.65). The DALYs cases decreased from 23,935,968 (95% UI: 21,127,958 to 26,691,398) in 1990 to 18,579,984 (95% UI: 15,702,408 to 21,843,560) in 2021 and the rate decreased from 238,416.27 (95% UI: 210,446.84 to 265,861.96)/100,000 in 1990 to 190,657.60 (95% UI: 161,129.49 to 224,146.63)/100,000 in 2021, AAPC −0.70 (95% CI: −0.83 to −0.57) (Table 1).
Table 1
| Global | 1990 | 2021 | AAPC (rate) | |||||
|---|---|---|---|---|---|---|---|---|
| Number of cases (95% UI) |
Rate per 100,000 people (95% UI) | Number of cases (95% UI) |
Rate per 100,000 people (95% UI) | Value (95% CI) | P | |||
| Incidence | 4,654,910 (4,590,168 to 4,726,630) |
46,365.63 (45,720.76 to 47,080.01) |
3,634,421 (3,580,612 to 3,694,913) |
37,294.43 (36,742.27 to 37,915.17) |
−0.71 (−0.76 to −0.65) |
<0.001 | ||
| DALYs | 23,935,968 (21,127,958 to 26,691,398) |
238,416.27 (210,446.84 to 265,861.96) |
18,579,984 (15,702,408 to 21,843,560) |
190,657.60 (161,129.49 to 224,146.63) |
−0.70 (−0.83 to −0.57) |
<0.001 | ||
P means P value for the significant test of AAPC. AAPC, average annual percentage change; CI, confidence interval; DALYs, disability-adjusted life years; UI, uncertainty interval.
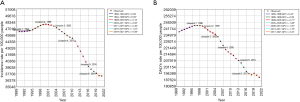
Joinpoint regression analysis of the incidence and DALYs rate of neonatal infectious diseases from 1990 to 2021 were shown in Figure 1. We found the incidence rate significantly increased from 1994–1999 (APC =0.59). Since 2003, the incidence rate significantly decreased (Figure 1A). For DALYs, the rate significantly increased from 1990–1996 (APC =0.44), and decreased from 1999–2017 (1999–2005 APC =−0.77, 2005–2008 APC =−1.98, 2008–2013 APC =−1.03, 2013–2017 APC =−1.76) (Figure 1B).
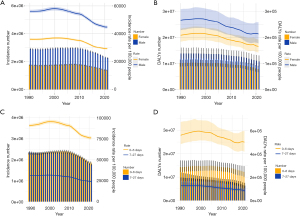
Sex and age groups
Figure 2 showed the trends in incidence and DALYs of neonatal infectious diseases by sex and age from 1990 to 2021. We found incidence and DALYs rate were decreasing overall. And there were gender and age differences, males and 0–6 days neonates had higher risk in neonatal infectious diseases.
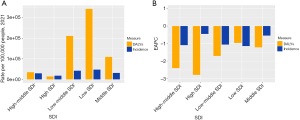
SDI region
In 2021, the highest cases and rates of incidence and DALYs in neonatal infectious diseases were shown in the low SDI regions (Table 2, Figure 3A). And from 1999 to 2019, all SDI regions showed a decreasing trend in both incidence and DALYs rates, the most rapid decreases of incidence rate were low SDI region (EAPC =−1.14), of DALYs rate were high SDI region (EAPC =−2.78) (Table 2, Figure 3B).
Table 2
| SDI | Number of cases, 1990 (95% UI) |
Rate per 100,000 people, 1990 (95% UI) |
Number of cases, 2021 (95% UI) |
Rate per 100,000 people, 2021 (95% UI) |
EAPC (rate) (95% CI) |
|---|---|---|---|---|---|
| Incidence | |||||
| High-middle SDI | 553,032 (534,727 to 571,790) |
39,920.96 (38,599.64 to 41,275.07) |
257,849 (249,223 to 266,811) |
28,920.43 (27,952.85 to 29,925.59) |
−1.09 (−1.27 to −0.91) |
| High SDI | 199,427 (195,358 to 203,932) |
20,978.72 (20,550.70 to 21,452.55) |
138,128 (135,727 to 140,605) |
17,621.97 (17,315.65 to 17,937.98) |
−0.45 (−0.50 to −0.39) |
| Low-middle SDI | 1,692,476 (1,644,580 to 1,740,894) |
58,459.90 (56,805.51 to 60,132.33) |
1,227,321 (1,195,320 to 1,259,764) |
41,836.53 (40,745.69 to 42,942.44) |
−1.05 (−1.17 to −0.93) |
| Low SDI | 1,113,909 (1,080,890 to 1,147,580) |
67,431.59 (65,432.74 to 69,469.93) |
1,279,828 (1,247,062 to 1,315,300) |
47,243.06 (46,033.56 to 48,552.49) |
−1.14 (−1.33 to −0.96) |
| Middle SDI | 1,092,275 (1,067,835 to 1,118,439) |
34,691.27 (33,915.05 to 35,522.26) |
728,492 (710,473 to 746,158) |
30,111.95 (29,367.12 to 30,842.15) |
−0.55 (−0.72 to −0.37) |
| DALYs | |||||
| High-middle SDI | 906,284 (803,382 to 1,015,756) |
65,420.71 (57,992.65 to 73,322.98) |
305,777 (259,749 to 356,377) |
34,296.03 (29,133.47 to 39,971.30) |
−2.40 (−2.58 to −2.23) |
| High SDI | 292,886 (262,944 to 328,238) |
30,810.05 (27,660.36 to 34,528.90) |
110,038 (97,094 to 121,938) |
14,038.30 (12,386.93 to 15,556.50) |
−2.78 (−3.00 to −2.56) |
| Low-middle SDI | 10,091,044 (8,712,251 to 11,601,244) |
348,555.33 (300,930.35 to 400,719.23) |
6,184,297 (5,014,056 to 7,618,968) |
210,808.30 (170,917.50 to 259,712.90) |
−1.70 (−1.76 to −1.63) |
| Low SDI | 7,971,027 (6,957,414 to 9,110,055) |
482,534.03 (421,173.97 to 551,486.22) |
9,311,147 (7,530,435 to 11,478,119) |
343,708.08 (277,975.55 to 423,698.82) |
−0.96 (−1.01 to −0.91) |
| Middle SDI | 4,659,163 (4,018,096 to 5,430,913) |
147,977.63 (127,616.99 to 172,488.86) |
2,655,229 (2,191,720 to 3,231,881) |
109,752.87 (90,593.93 to 133,588.60) |
−1.21 (−1.42 to −0.99) |
CI, confidence interval; DALYs, disability-adjusted life years; EAPC, estimated annual percentage change; SDI, socio-demographic index; UI, uncertainty interval.
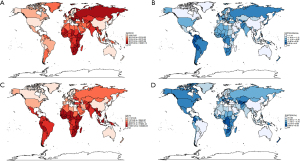
Regional trends
Across the regional level, we found in 2021, Southern Sub-Saharan Africa had the highest incidence rate (90,810.01/100,000), Western Sub-Saharan Africa had the highest DALYs rate (440,999.84/100,000) (Table 3, Figure 4A). In most regions, the incidence and DALYs rates of neonatal infectious diseases were decreasing, except Andean Latin America, Caribbean, Central Asia and Southern Sub-Saharan Africa. The most rapid decreases of incidence rate were High-income Asia Pacific (EAPC =−1.51), and of DALYs rate were Central Europe (EAPC =−5.82) (Table 3, Figure 4B).
Table 3
| Region | Number of cases, 1990 (95% UI) |
Rate per 100,000 people, 1990 (95% UI) | Number of cases, 2021 (95% UI) |
Rate per 100,000 people, 2021 (95% UI) | EAPC (rate) (95% CI) |
|---|---|---|---|---|---|
| Incidence | |||||
| Andean Latin America | 13,549 (12,609 to 14,494) |
15,336.78 (14,272.81 to 16,407.00) |
15,967 (14,988 to 16,956) |
16,998.34 (15,956.50 to 18,051.37) |
1.09 (0.83 to 1.35) |
| Australasia | 5,610 (5,027 to 6,260) |
23,247.01 (20,830.62 to 25,940.41) |
4,145 (3,737 to 4,630) |
15,219.43 (13,719.67 to 16,999.55) |
−1.32 (−1.45 to −1.20) |
| Caribbean | 15,437 (14,709 to 16,209) |
22,752.90 (21,680.67 to 23,891.39) |
13,872 (13,095 to 14,703) |
23,106.05 (21,811.82 to 24,490.90) |
0.39 (−0.18 to 0.59) |
| Central Asia | 72,708 (69,329 to 76,212) |
48,977.83 (46,701.67 to 51,337.74) |
59,219 (56,163 to 62,326) |
38,184.75 (36,213.89 to 40,188.09) |
−0.92 (−1.10 to −0.74) |
| Central Europe | 95,731 (91,681 to 100,005) |
73,395.51 (70,290.45 to 76,671.94) |
44,652 (42,855 to 46,526) |
56,002.41 (53,748.50 to 58,352.66) |
−0.98 (−1.08 to −0.88) |
| Central Latin America | 99,831 (97,039 to 102,655) |
26,487.61 (25,746.74 to 27,236.65) |
59,518 (57,830 to 61,101) |
20,093.69 (19,523.91 to 20,627.91) |
−0.71 (−0.88 to −0.55) |
| Central Sub-Saharan Africa | 99,593 (92,078 to 108,384) |
51,805.60 (47,896.46 to 56,378.41) |
138,496 (127,724 to 150,731) |
41,237.41 (38,029.94 to 44,880.39) |
−0.59 (−0.89 to −0.29) |
| East Asia | 289,898 (280,845 to 300,189) |
16,029.16 (15,528.57 to 16,598.17) |
93,419 (91,460 to 95,664) |
10,664.54 (10,440.93 to 10,920.84) |
−1.44 (−1.58 to −1.31) |
| Eastern Europe | 171,277 (157,595 to 184,437) |
75,444.68 (69,417.93 to 81,241.43) |
80,892 (74,549 to 88,164) |
59,167.37 (54,528.49 to 64,486.82) |
−0.88 (−0.99 to −0.76) |
| Eastern Sub-Saharan Africa | 558,647 (533,045 to 582,979) |
83,359.72 (79,539.45 to 86,990.51) |
569,142 (546,396 to 592,268) |
55,249.53 (53,041.43 to 57,494.45) |
−1.43 (−1.58 to −1.27) |
| High-income Asia Pacific | 22,428 (20,826 to 24,246) |
14,924.40 (13,857.89 to 16,133.62) |
8,354 (7,969 to 8,798) |
9,222.06 (8,797.14 to 9,712.36) |
−1.51 (−1.62 to −1.40) |
| High-income North America | 44,720 (43,334 to 46,218) |
12,876.93 (12,477.83 to 13,308.33) |
29,567 (28,677 to 30,415) |
9,581.20 (9,292.77 to 9,856.04) |
−0.95 (−0.97 to −0.93) |
| North Africa and Middle East | 385,911 (371,854 to 400,323) |
46,889.01 (45,181.09 to 48,640.02) |
277,362 (267,716 to 287,536) |
30,682.51 (29,615.44 to 31,807.92) |
−1.31 (−1.51 to −1.10) |
| Oceania | 6,321 (5,826 to 6,907) |
37,300.13 (34,377.34 to 40,756.00) |
9,987 (9,108 to 10,873) |
30,921.76 (28,198.56 to 33,663.38) |
−0.56 (−0.76 to −0.36) |
| South Asia | 1,605,088 (1,555,336 to 1,650,657) |
62,614.52 (60,673.71 to 64,392.18) |
1,065,325 (1,033,451 to 1,102,156) |
44,789.20 (43,449.12 to 46,337.66) |
−1.04 (−1.11 to −0.97) |
| Southeast Asia | 434,099 (411,243 to 459,296) |
46,671.43 (44,214.10 to 49,380.54) |
288,009 (271,249 to 304,950) |
33,834.73 (31,865.88 to 35,824.90) |
−1.09 (−1.18 to −0.99) |
| Southern Latin America | 23,452 (21,291 to 25,798) |
29,336.77 (26,633.78 to 32,272.03) |
13,834 (12,649 to 15,093) |
23,490.18 (21,478.57 to 25,628.01) |
−0.53 (−0.64 to −0.42) |
| Southern Sub-Saharan Africa | 128,654 (119,219 to 139,469) |
105,580.35 (97,837.89 to 114,455.39) |
111,647 (103,453 to 120,328) |
90,810.01 (84,145.17 to 97,871.51) |
−0.43 (−0.55 to −0.32) |
| Tropical Latin America | 73,411 (71,284 to 75,655) |
28,967.55 (28,128.43 to 29,853.11) |
56,366 (54,700 to 57,963) |
21,562.46 (20,925.07 to 22,173.38) |
−0.59 (−0.78 to −0.40) |
| Western Europe | 97,550 (94,546 to 100,556) |
27,711.38 (26,857.82 to 28,565.13) |
79,642 (77,704 to 81,730) |
25,504.13 (24,883.53 to 26,172.77) |
−0.12 (−0.18 to −0.05) |
| Western Sub-Saharan Africa | 410,994 (389,025 to 434,032) |
61,607.08 (58,313.95 to 65,060.37) |
615,007 (584,257 to 647,049) |
46,116.62 (43,810.83 to 48,519.31) |
−0.91 (−1.16 to −0.65) |
| DALYs | |||||
| Andean Latin America | 317,580 (246,790 to 394,495) |
359,490.61 (279,358.18 to 446,555.03) |
154,976 (114,044 to 205,858) |
164,986.18 (121,410.41 to 219,155.11) |
−1.83 (−2.04 to −1.61) |
| Australasia | 4,806 (4,388 to 5,265) |
19,917.61 (18,185.04 to 21,819.05) |
2,394 (1,987 to 2,852) |
8,788.99 (7,293.23 to 10,470.36) |
−2.44 (−3.16 to −1.70) |
| Caribbean | 182,879 (139,133 to 233,654) |
269,556.39 (205,075.53 to 344,395.75) |
183,228 (133,283 to 244,465) |
305,201.05 (222,007.63 to 407,201.54) |
0.48 (0.34 to 0.62) |
| Central Asia | 82,968 (67,643 to 108,681) |
55,889.03 (45,565.69 to 73,209.96) |
96,211 (80,754 to 115,926) |
62,037.21 (52,070.37 to 74,749.37) |
0.44 (0.12 to 0.76) |
| Central Europe | 44,053 (38,101 to 54,208) |
33,774.95 (29,211.70 to 41,560.61) |
5,938 (4,915 to 7,138) |
7,447.72 (6,164.46 to 8,952.67) |
−5.82 (−6.49 to −5.14) |
| Central Latin America | 665,154 (619,632 to 713,202) |
176,481.01 (164,402.92 to 189,229.15) |
431,575 (340,180 to 540,184) |
145,702.27 (114,846.75 to 182,369.28) |
−0.65 (−00.79 to −0.51) |
| Central Sub-Saharan Africa | 364,079 (250,601 to 512,296) |
189,384.28 (130,356.03 to 266,482.37) |
503,970 (298,362 to 810,498) |
150,058.20 (88,837.93 to 241,327.31) |
−0.27 (−0.54 to 0.01) |
| East Asia | 613,158 (478,230 to 764,798) |
33,902.96 (26,442.45 to 42,287.46) |
99,416 (73,536 to 124,586) |
11,349.22 (8,394.76 to 14,222.53) |
−3.57 (−3.78 to −3.36) |
| Eastern Europe | 129,686 (118,871 to 146,650) |
57,124.40 (52,360.50 to 64,596.83) |
68,588 (60,609 to 76,500) |
50,167.89 (44,331.53 to 55,955.55) |
−0.95 (−1.41 to −0.50) |
| Eastern Sub-Saharan Africa | 3,894,568 (3,356,492 to 4,534,183) |
581,136.53 (500,846.30 to 676,577.98) |
4,020,996 (3,112,800 to 5,102,904) |
390,338.58 (302,175.42 to 495,364.96) |
−1.10 (−1.19 to −1.02) |
| High-income Asia Pacific | 30,202 (25,076 to 36,650) |
20,096.99 (16,686.22 to 24,387.46) |
4,773 (3,986 to 5,687) |
5,268.84 (4,400.53 to 6,278.21) |
−4.27 (−4.44 to −4.10) |
| High-income North America | 78,123 (75,640 to 80,471) |
22,495.20 (21,780.02 to 23,171.21) |
55,482 (49,677 to 61,659) |
17,978.87 (16,097.91 to 19,980.84) |
−0.73 (−1.01 to 0.44) |
| North Africa and Middle East | 722,825 (588,677 to 866,533) |
87,824.74 (71,525.46 to 105,285.56) |
356,028 (272,325 to 454,389) |
39,384.69 (30,125.25 to 50,265.64) |
−2.80 (−2.93 to −2.67) |
| Oceania | 13,314 (8,446 to 19,756) |
78,562.88 (49,839.34 to 116,580.47) |
24,767 (14,487 to 39,276) |
76,681.66 (44,854.55 to 121,606.24) |
−0.12 (−0.36 to 0.12) |
| South Asia | 8,204,979 (7,056,318 to 9,728,176) |
320,076.46 (275,267.16 to 379,496.43) |
4,545,958 (3,651,721 to 5,535,297) |
191,124.59 (153,528.41 to 232,719.11) |
−1.80 (−1.88 to −1.73) |
| Southeast Asia | 3,060,985 (2,397,056 to 3,915,655) |
329,097.03 (257,715.72 to 420,985.52) |
1,549,110 (1,177,157 to 2,116,952) |
181,986.54 (138,290.26 to 248,695.59) |
−1.97 (−2.10 to −1.83) |
| Southern Latin America | 111,540 (98,748 to 123,550) |
139,529.08 (123,527.46 to 154,552.55) |
31,282 (24,180 to 39,703) |
53,116.57 (41,057.06 to 67,414.60) |
−3.39 (−3.65 to −3.13) |
| Southern Sub-Saharan Africa | 260,024 (203,888 to 316,933) |
213,389.47 (167,321.58 to 260,092.66) |
269,250 (214,217 to 332,464) |
218,999.83 (174,237.41 to 270,416.19) |
0.38 (0.21 to 0.55) |
| Tropical Latin America | 726,958 (643,887 to 818,222) |
286,853.89 (254,074.35 to 322,866.05) |
258,436 (203,109 to 324,927) |
98,863.43 (77,698.29 to 124,298.94) |
−3.23 (−3.71 to −2.75) |
| Western Europe | 74,573 (71,800 to 77,198) |
21,184.19 (20,396.33 to 21,929.89) |
36,471 (31,077 to 41,975) |
11,679.32 (9,951.84 to 13,441.77) |
−1.59 (−1.82 to −1.36) |
| Western Sub-Saharan Africa | 4,353,511 (3,569,148 to 5,109,639) |
652,581.77 (535,007.54 to 765,923.67) |
5,881,136 (4,827,864 to 7,014,513) |
440,999.84 (362,019.72 to 525,986.68) |
−1.17 (−1.23 to −1.11) |
CI, confidence interval; DALYs, disability-adjusted life years; EAPC, estimated annual percentage change; UI, uncertainty interval.

National trends
Across the national level, we found in most countries, the incidence and DALYs rates of the neonatal infectious diseases were decreasing (Figure 5). Africa had higher disease burden with lower SDI values. The most rapid decreases of incidence rate were Slovakia (EAPC =−2.51) and Israel (EAPC =−2.01), both were high SDI countries. The most rapid decreases of DALYs rate were Poland (EAPC =−8.54) and Serbia (EAPC =−6.43), also both were high SDI countries (Figure 5).
Discussion
We used GBD database to analyze the worldwide distribution, regional variances, temporal trends, and socio-economic associations of neonatal infectious disease incidence and DALYs. Our study indicated that the trend in the burden of neonatal infectious diseases from 1990 to 2021 by incidence and DALYs is decreasing overall. Except Andean Latin America, Caribbean, Central Asia and Southern Sub-Saharan Africa, other regions defined by the GBD reported declines in incidence and DALY rates of neonatal infectious diseases. Among the 204 countries analysed, Slovakia showed the most decrease in incidence rate and Poland showed the most decrease in DALYs rate. In terms of SDI regions, both the highest cases and rates for neonatal infectious diseases were shown in the low SDI regions in 2021.
Severe systemic infections, classified as neonatal sepsis, is a life-threatening disease and associated with adverse neurodevelopmental outcome (9-11). A recent resolution by World Health Organization (WHO) listed sepsis as a key health-care priority for the coming decade and peak sepsis incidence occur in the extreme age groups, with newborn babies, young children, and elderly people at highest risk (12). Many previous studies have described the incidence of neonatal sepsis and the GBD. Studies have shown the incidence of neonatal sepsis was 1.8-fold higher in middle-income countries and 3.5-fold higher in low-income countries compared with high-income countries. And the incidence and mortality of EOS were higher than LOS (13). However, other neonatal infectious diseases such as enteric infections, upper respiratory infections, lower respiratory infections, and tetanus can also cause severe harm (14-17). Previous studies have shown that neonatal infectious diseases affect nearly 3.9 million neonates (18,19), but in our study we found in 2021, the number of incident cases of neonatal infectious diseases is 3,634,421, which is lower than previous studies, reflecting significant strides in neonatal health over recent decades. With advances in medical and socio-economic development, the burden of neonatal infectious diseases is decreasing.
From a global perspective, three-quarters of newborn deaths occur in the first week after birth, and the incidence of EOS were higher than LOS, therefore, conducting age-stratified research on incidence and DALYs associated with neonatal infectious diseases is significant importance. Our study indicated that 0–6 days have higher risk in neonatal infectious diseases, which aligns with the outcomes of previous studies.
There is also a gender difference, males have higher risk in neonatal infectious diseases. Previous multiple studies highlight a significant role of sex chromosome complement on overall immunity, many genes with immunomodulatory function are encoded on the X chromosome, lead males are generally more susceptible than females to infections (20,21). And this is consistent with our findings, male newborns have a higher burden of disease.
Additionally, significant variations were observed across different regions and countries. Previous studies have mentioned that in developing countries, the incidence of neonatal infectious diseases is higher, especially in Africa (22-25), and our study also confirm this. Through the analysis of SDI, regions and countries, we find the burden of neonatal infectious diseases is related to socio-economic development. With better socio-economic development have relatively lower disease burdens.
Neonatal infections have non-specific symptoms, thus diagnosing neonatal infectious disease can be challenging (26), repeated clinical assessments and laboratory investigations may help rule out infection and avoid unnecessary antibiotic treatment, but they are often unfeasible in low-income countries (24,27).
Health system coverage can affect neonatal health outcomes (28). Low- and middle-income countries are more likely to face challenges such as inadequate drinking water, poor sanitation, incorrect hygiene behaviours and weak healthcare infrastructure, and that remain critical determinants of the global disease burden, particularly among young children (29-33). Additionally, vaccine inequality exacerbates disparities in infectious disease outcomes, high-income countries secured vaccines faster, while low- and middle-income nations faced delays. Vaccination plays a critical role in preventing infectious diseases by stimulating the immune system to recognize and combat pathogens such as viruses and bacteria, is one of the most effective public health interventions.
Education and religion are related to disease prevention and treatment (34). In low- and middle-income countries, families and healthcare workers often lack the necessary knowledge and training to identify infections at an early stage, leading to delays in treatment (35,36). Certain religious practices may increase the risk of infectious diseases, for example, by rejecting vaccinations, refusing medical interventions, or promoting unhealthy dietary habits.
Antibiotic resistance has become a persistent global health threat (37). Low- and middle-income countries have misuse of antibiotics and population level resistance, that cause high resistance to antibiotics (38,39). Antibiotics resistance can lead to poor treatment of infectious diseases.
The data in the article are all sourced from the GBD database, this time-trends data can be used to monitor disease patterns and identify long-term trends by tracking the incidence and DALYs over time. In addition, can reveal disparities among different demographic groups and help forecast future disease burdens, guiding targeted interventions. This study provided a comprehensive analysis of the global, regional, and national burden of neonatal infectious diseases from 1990 to 2021 using the latest GBD 2021 data. The insights were valuable for policymakers and healthcare providers in developing more effective health policies, optimizing resource allocation, and implementing tailored healthcare interventions. This research made a contribution to global efforts aimed at reducing neonatal mortality and improving long-term child health outcomes, ultimately supporting the achievement of Sustainable Development Goal targets related to child survival and public health improvement.
There are several limitations to this study. Firstly, diagnosis of neonatal infections is challenging. Neonatal infections often manifest with a wide range of non-specific clinical signs, such as feeding intolerance, respiratory distress, episodes of apnea, bradycardia, increased oxygen requirement, lethargy, hypotension, temperature dysregulation, rash and prolonged inconsolable crying. These ambiguous presentations potentially resulting in both misdiagnosis and overdiagnosis, especially in Low- and middle-income countries (40). Secondly, the accuracy of burden estimation relies on the availability and quality of data from the GBD database, there may be a lack of access to the raw/original data for some countries, particularly in low- and middle-income countries. Thirdly, variations in the diagnosis and detection protocols across countries and over time may potentially impact the comparability of results.
Conclusions
Overall, the burden of neonatal infectious diseases has decreased worldwide. Males and 0–6 days neonates have higher risk. And the burden of neonatal infectious diseases is related to SDI values, high SDI countries have a relatively lower disease burden. Though the burden of disease is decreasing, regional and national differences are still significant, improving socio-economic levels and enhancing disease management are very important.
Acknowledgments
We highly appreciate the efforts of the GBD 2021 collaborators.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-57/rc
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-57/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-57/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Plano LR. The changing spectrum of neonatal infectious disease. J Perinatol 2010;30:S16-20. [Crossref] [PubMed]
- Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1459-544. [Crossref] [PubMed]
- Glaser MA, Hughes LM, Jnah A, et al. Neonatal Sepsis: A Review of Pathophysiology and Current Management Strategies. Adv Neonatal Care 2021;21:49-60. [Crossref] [PubMed]
- Bethou A, Bhat BV. Neonatal Sepsis-Newer Insights. Indian J Pediatr 2022;89:267-73. [Crossref] [PubMed]
- Shane AL, Sánchez PJ, Stoll BJ. Neonatal sepsis. Lancet 2017;390:1770-80. [Crossref] [PubMed]
- Masanja PP, Kibusi SM, Mkhoi ML. Predictors of Early Onset Neonatal Sepsis among Neonates in Dodoma, Tanzania: A Case Control Study. J Trop Pediatr 2020;66:257-66. [Crossref] [PubMed]
- Traoré FB, Sidibé CS, Diallo EHM, et al. Prevalence and factors associated with maternal and neonatal sepsis in sub-Saharan Africa: a systematic review and meta-analysis. Front Public Health 2024;12:1272193. [Crossref] [PubMed]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. [Crossref] [PubMed]
- De Rose DU, Ronchetti MP, Martini L, et al. Diagnosis and Management of Neonatal Bacterial Sepsis: Current Challenges and Future Perspectives. Trop Med Infect Dis 2024;9:199. [Crossref] [PubMed]
- Hayes R, Hartnett J, Semova G, et al. Neonatal sepsis definitions from randomised clinical trials. Pediatr Res 2023;93:1141-8. [Crossref] [PubMed]
- Ong WJ, Seng JJB, Yap B, et al. Impact of neonatal sepsis on neurocognitive outcomes: a systematic review and meta-analysis. BMC Pediatr 2024;24:505. [Crossref] [PubMed]
- Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, et al. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med 2018;6:223-30. [Crossref] [PubMed]
- Fleischmann C, Reichert F, Cassini A, et al. Global incidence and mortality of neonatal sepsis: a systematic review and meta-analysis. Arch Dis Child 2021;106:745-52. [Crossref] [PubMed]
- Thapar N, Sanderson IR. Diarrhoea in children: an interface between developing and developed countries. Lancet 2004;363:641-53. [Crossref] [PubMed]
- Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine 2021;37:100986. [Crossref] [PubMed]
- GBD 2019 LRI Collaborators. Age-sex differences in the global burden of lower respiratory infections and risk factors, 1990-2019: results from the Global Burden of Disease Study 2019. Lancet Infect Dis 2022;22:1626-47. [Crossref] [PubMed]
- Li J, Liu Z, Yu C, et al. Global epidemiology and burden of tetanus from 1990 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. Int J Infect Dis 2023;132:118-26. [Crossref] [PubMed]
- Rosa-Mangeret F, Benski AC, Golaz A, et al. 2.5 Million Annual Deaths-Are Neonates in Low- and Middle-Income Countries Too Small to Be Seen? A Bottom-Up Overview on Neonatal Morbi-Mortality. Trop Med Infect Dis 2022;7:64. [Crossref] [PubMed]
- Lavoie PM, Popescu CR, Molyneux EM, et al. Rethinking management of neonates at risk of sepsis. Lancet 2019;394:279-81. [Crossref] [PubMed]
- Jacobsen H, Klein SL. Sex Differences in Immunity to Viral Infections. Front Immunol 2021;12:720952. [Crossref] [PubMed]
- Dias SP, Brouwer MC, van de Beek D. Sex and Gender Differences in Bacterial Infections. Infect Immun 2022;90:e0028322. [Crossref] [PubMed]
- Ganatra HA, Zaidi AK. Neonatal infections in the developing world. Semin Perinatol 2010;34:416-25. [Crossref] [PubMed]
- Ranjeva SL, Warf BC, Schiff SJ. Economic burden of neonatal sepsis in sub-Saharan Africa. BMJ Glob Health 2018;3:e000347. [Crossref] [PubMed]
- Rosa-Mangeret F, Dupuis M, Dewez JE, et al. Challenges and opportunities in neonatal sepsis management: insights from a survey among clinicians in 25 Sub-Saharan African countries. BMJ Paediatr Open 2024;8:e002398. [Crossref] [PubMed]
- Sturrock S, Sadoo S, Nanyunja C, et al. Improving the Treatment of Neonatal Sepsis in Resource-Limited Settings: Gaps and Recommendations. Res Rep Trop Med 2023;14:121-34. [Crossref] [PubMed]
- Cohen R, Romain O, Tauzin M, et al. Neonatal bacterial infections: Diagnosis, bacterial epidemiology and antibiotic treatment. Infect Dis Now 2023;53:104793. [Crossref] [PubMed]
- Stocker M, van Herk W, El Helou S, et al. C-Reactive Protein, Procalcitonin, and White Blood Count to Rule Out Neonatal Early-onset Sepsis Within 36 Hours: A Secondary Analysis of the Neonatal Procalcitonin Intervention Study. Clin Infect Dis 2021;73:e383-90. [Crossref] [PubMed]
- Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1250-84. [Crossref] [PubMed]
- Prüss-Ustün A, Wolf J, Bartram J, et al. Burden of disease from inadequate water, sanitation and hygiene for selected adverse health outcomes: An updated analysis with a focus on low- and middle-income countries. Int J Hyg Environ Health 2019;222:765-77. [Crossref] [PubMed]
- Mitra DK, Mullany LC, Harrison M, et al. Incidence and risk factors of neonatal infections in a rural Bangladeshi population: a community-based prospective study. J Health Popul Nutr 2018;37:6. [Crossref] [PubMed]
- Wolf J, Johnston RB, Ambelu A, et al. Burden of disease attributable to unsafe drinking water, sanitation, and hygiene in domestic settings: a global analysis for selected adverse health outcomes. Lancet 2023;401:2060-71. [Crossref] [PubMed]
- Mebrahtom S, Worku A, Gage DJ. The risk of water, sanitation and hygiene on diarrhea-related infant mortality in eastern Ethiopia: a population-based nested case-control. BMC Public Health 2022;22:343. [Crossref] [PubMed]
- Arowosegbe AO, Ojo DA, Shittu OB, et al. Water, sanitation, and hygiene (WASH) facilities and infection control/prevention practices in traditional birth homes in Southwest Nigeria. BMC Health Serv Res 2021;21:912. [Crossref] [PubMed]
- Aziz A, Saleem S, Nolen TL, et al. Why are the Pakistani maternal, fetal and newborn outcomes so poor compared to other low and middle-income countries? Reprod Health 2020;17:190. [Crossref] [PubMed]
- Huynh BT, Padget M, Garin B, et al. Bacterial neonatal sepsis and antibiotic resistance in low-income countries. Lancet 2016;387:533-4. [Crossref] [PubMed]
- Doherty T, Tran N, Sanders D, et al. Role of district health management teams in child health strategies. BMJ 2018;362:k2823. [Crossref] [PubMed]
- Frieri M, Kumar K, Boutin A. Antibiotic resistance. J Infect Public Health 2017;10:369-78. [Crossref] [PubMed]
- Mendelson M, Røttingen JA, Gopinathan U, et al. Maximising access to achieve appropriate human antimicrobial use in low-income and middle-income countries. Lancet 2016;387:188-98. [Crossref] [PubMed]
- Thomson KM, Dyer C, Liu F, et al. Effects of antibiotic resistance, drug target attainment, bacterial pathogenicity and virulence, and antibiotic access and affordability on outcomes in neonatal sepsis: an international microbiology and drug evaluation prospective substudy (BARNARDS). Lancet Infect Dis 2021;21:1677-88. [Crossref] [PubMed]
- Popescu CR, Cavanagh MMM, Tembo B, et al. Neonatal sepsis in low-income countries: epidemiology, diagnosis and prevention. Expert Rev Anti Infect Ther 2020;18:443-52. [Crossref] [PubMed]


