Initial experience of a simplified modified Politano-Leadbetter technique for pneumovesicoscopic ureteral reimplantation in children
Highlight box
Key findings
• By standardizing essential procedural steps and optimizing the use of anatomical landmarks, this modified pneumovesicoscopic ureteral reimplantation using the Politano-Leadbetter (PVUR-PL) technique enhances the procedural applicability and simplifies surgical execution, particularly benefiting surgeons early in their learning curve.
What is known and what is new?
• The Politano-Leadbetter (PL) ureteral reimplantation technique preserves the natural direction of the ureter, preventing angulation and facilitating subsequent retrograde ureteroscopy for diagnostic and therapeutic purposes. However, the PVUR-PL is technically more demanding compared to the Cohen technique. With regard to the minimum age of the patients, minimal working space and difficulties in establishing the pneumovesicum and accurately locating the proximal retrovesical ureter were named as limiting factors.
• In this study, we introduce modifications to the PVUR-PL technique that simplify the operative procedure, improve the establishment of the pneumatic bladder trocar channel, and allow precise identification of the proximal retrovesical ureter. These improvements are especially beneficial in infants with limited bladder capacity and obese children with elevated body mass index, broadening the technique’s applicability, significantly reducing operative time, and minimizing tissue trauma.
What is the implication, and what should change now?
• This refinement improves accessibility to the PL approach without compromising surgical outcomes. These improvements may facilitate wider adoption of PVUR-PL among pediatric urologists. We appreciate the experts’ review and promotion.
Introduction
Primary vesicoureteral obstruction (UVJO) and vesicoureteral reflux (VUR) are common congenital anomalies of the upper urinary tract in children. The prevalence of VUR ranges from 0.4% to 1.8% (1), while UVJO occurs in approximately 0.36 per 1,000 to 1,500 live births (2-4). Surgical intervention, typically involving ureteral reimplantation, is commonly indicated for patients with UVJO or severe VUR. Although open ureteral reimplantation with a submucosal tunnel has traditionally been regarded as the gold standard, advancements in minimally invasive techniques have increasingly favored laparoscopic and endoscopic approaches (5-8).
The three primary techniques for ureterovesical reimplantation are the Lich-Gregoir, Cohen, and Politano-Leadbetter (PL) procedures. Transvesicoscopic cross-trigonal ureteral reimplantation (Cohen technique), first introduced by Yeung (5) in 2005, involves insufflation of the bladder with CO2. Numerous studies have demonstrated low complication rates and excellent success rates (90–98%) associated with this approach (9-11). However, a notable limitation is that the cross-trigonal submucosal tunnel alters the ureter’s natural course, potentially complicating future retrograde ureteral catheterization or ureteroscopy (12-14).
The Lich-Gregoir technique, an effective extravesical approach for ureteral reimplantation, preserves the natural ureteral alignment. However, its primary drawback is potential detrusor neurovascular injury, which increases the risk of postoperative urinary retention (15,16). This complication often necessitates prolonged catheterization and limits the applicability of this method in bilateral cases.
The PL ureteral reimplantation technique preserves the natural direction of the ureter, preventing angulation and facilitating subsequent retrograde ureteroscopy for diagnostic and therapeutic purposes. However, the PL method for pneumovesicoscopic ureteral reimplantation using the Politano-Leadbetter (PVUR-PL) technique is technically more demanding compared to the Cohen technique, primarily due to challenges in establishing the pneumatic bladder trocar channel and accurately locating the proximal retrovesical ureter through a newly created hiatus (17,18).
In this study, we introduce modifications to the PVUR-PL technique that simplify the operative procedure, improve the establishment of the pneumatic bladder trocar channel, and allow precise identification of the proximal retrovesical ureter. These improvements are especially beneficial in infants with limited bladder capacity and obese children with elevated body mass index (BMI), broadening the technique’s applicability, significantly reducing operative time, and minimizing tissue trauma. We present this article in accordance with the STROCSS reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-200/rc).
Methods
Patients and study design
The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. This study was approved by the Ethics Committee of Tianjin Children’s Hospital (approval No. 2022-LXKY-010), and informed consent from the participants’ legal guardian/next of kin was not required in accordance with the national legislation and the institutional requirements. We retrospectively reviewed medical records of patients who underwent PVUR-PL from November 2021 to May 2024. Surgical indications included persistent UVJO, severe primary VUR [high-grade VUR or recurrent febrile urinary tract infections (UTIs)], and other vesicoureteral junction malformations requiring intervention. All procedures were conducted by the same surgeon. Initially, PVUR-PL was conducted using the method described by Baek et al. (17). Beginning in November 2022, we introduced modifications to the traditional technique based on cumulative surgical experience and local anatomical considerations. Accordingly, patients were divided into two groups: a traditional group (using Baek’s original technique) and a modified group (employing our refined methods).
Clinical data including age, gender, bladder capacity, BMI, disease type, operative time, postoperative hematuria, postoperative febrile UTIs, pain scores, and treatment outcomes were collected and analyzed. Operative time was defined from cystoscopy initiation to completion of trocar port closure. Pain scores were assessed using the Face, Legs, Activity, Cry, Consolability (FLACC) scale for patients under 6 years of age and the visual analog scale (VAS) for those aged 6 years and above. Bladder capacity was calculated using Koff’s formula: (age in years + 2) × 30 mL (19). Patients with megaureter requiring ureteral tailoring and those with follow-up periods shorter than 6 months were excluded. Postoperative ultrasound examinations were performed at 3, 6, and 12 months, and voiding cystourethrography (VCUG) was conducted approximately 6 months postoperatively to confirm resolution or absence of VUR when indicated.
Surgical procedures
- Patient positioning: the patient was placed in the lithotomy position.
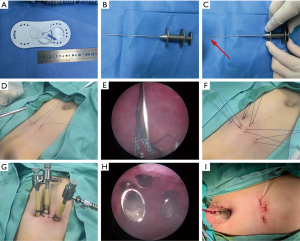
- Pneumovesicum establishment: the surgical establishment of bladder-abdominal wall adhesion and trocar fixation is illustrated in Figure 1. After filling the bladder with saline or CO2, an artificial adhesion between the bladder and abdominal wall was created using a long curved needle under cystoscopic guidance (Figure 1A,1D,1F). In cases with thicker abdominal walls, a hooked hernia needle facilitated this procedure (Figure 1B,1C,1E). Subsequently, a 5 mm trocar was introduced into the bladder cavity under cystoscopic visualization (Figure 1H) and fixed to prevent displacement. Two additional 5 mm trocars were similarly inserted into each side of the bladder and secured (Figure 1G).
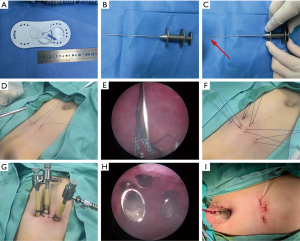 Figure 1 Surgical establishment of bladder-abdominal wall adhesion and trocar fixation. (A) A 1/2 arc, 40 mm round needle, for establishing the artificial “bladder abdominal wall adhesion area”. (B) A hooked hernia needle, for establishing the artificial “bladder abdominal wall adhesion area”. (C) The arrow shows the open tip of the crochet. (D) The abdominal wall and bladder were sutured with a needle. (E) The abdominal wall and bladder were sutured with a hooked hernia needle. (F) Appearance of sutures for fixing trocars, and two sutures for each puncture site. (G) Appearance of the trocars. (H) The depth of the bladder trocar. (I) Appearance of abdominal incision.
Figure 1 Surgical establishment of bladder-abdominal wall adhesion and trocar fixation. (A) A 1/2 arc, 40 mm round needle, for establishing the artificial “bladder abdominal wall adhesion area”. (B) A hooked hernia needle, for establishing the artificial “bladder abdominal wall adhesion area”. (C) The arrow shows the open tip of the crochet. (D) The abdominal wall and bladder were sutured with a needle. (E) The abdominal wall and bladder were sutured with a hooked hernia needle. (F) Appearance of sutures for fixing trocars, and two sutures for each puncture site. (G) Appearance of the trocars. (H) The depth of the bladder trocar. (I) Appearance of abdominal incision. - Ureteral mobilization: the key steps of the modified PVUR-PL technique are illustrated in Figure 2. A 5-0 Vicryl traction suture was placed just distal to the ureteral orifice (Figure 2A) to facilitate gentle ureteral mobilization, performed transvesicoscopically with a hook electrode. In male patients, care was taken to avoid vas deferens injury.
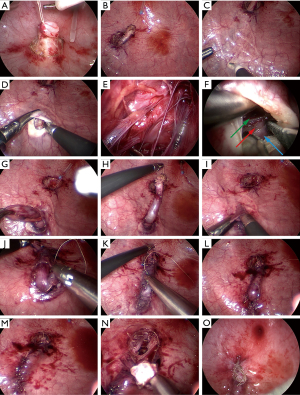
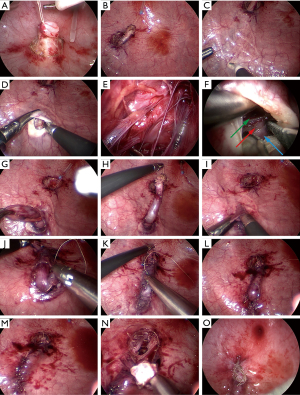 Figure 2 Key steps of modified PVUR-PL technique. (A) The distal ureter is mobilized by a hook electrode. (B) The distal end of the ureter is sutured to the tube for pulling to show the course of the ureter. (C) Neo-hiatus selection in a straight line superior to the original orifice. (D) Upon complete opening of the detrusor layer, light yellow adipose tissue and thin, white, loose reticular fascial tissue—representing the retrovesical extraperitoneal tissue—can be observed. (E) If the detrusor space is inadvertently entered, crisscrossing blood vessels, nerves, and muscle fibers may be visualized. (F) The posterior bladder tissue was dissociated slightly distal to the neo-hiatus to prevent rupture into the peritoneal cavity, expose the vas deferens, the green arrow shows the vas deferens, the red arrow shows the ureter, and the blue arrow shows the peritoneal reflextion. (G) The ureter is dragged into the bladder at the neo-hiatus. (H) Make sure that the length of the ureter is relaxed enough. (I) Submucosal tunnels were made. (J) Fix the ureteral at the new hiatus with the surrounding bladder detrusor on one side. (K) Fix the ureteral at the new hiatus with the surrounding bladder detrusor on the other side, ensuring they were not aligned in the same horizontal plane to avoid lateral traction of the ureter. (L) The detrusor was closed at the neo-hiatus. (M) The mucosa was closed at the neo-hiatus. (N) The detrusor was closed at the original hiatus. (O) The ureteral orifice was formed. PVUR-PL, pneumovesicoscopic ureteral reimplantation using the Politano-Leadbetter.
Figure 2 Key steps of modified PVUR-PL technique. (A) The distal ureter is mobilized by a hook electrode. (B) The distal end of the ureter is sutured to the tube for pulling to show the course of the ureter. (C) Neo-hiatus selection in a straight line superior to the original orifice. (D) Upon complete opening of the detrusor layer, light yellow adipose tissue and thin, white, loose reticular fascial tissue—representing the retrovesical extraperitoneal tissue—can be observed. (E) If the detrusor space is inadvertently entered, crisscrossing blood vessels, nerves, and muscle fibers may be visualized. (F) The posterior bladder tissue was dissociated slightly distal to the neo-hiatus to prevent rupture into the peritoneal cavity, expose the vas deferens, the green arrow shows the vas deferens, the red arrow shows the ureter, and the blue arrow shows the peritoneal reflextion. (G) The ureter is dragged into the bladder at the neo-hiatus. (H) Make sure that the length of the ureter is relaxed enough. (I) Submucosal tunnels were made. (J) Fix the ureteral at the new hiatus with the surrounding bladder detrusor on one side. (K) Fix the ureteral at the new hiatus with the surrounding bladder detrusor on the other side, ensuring they were not aligned in the same horizontal plane to avoid lateral traction of the ureter. (L) The detrusor was closed at the neo-hiatus. (M) The mucosa was closed at the neo-hiatus. (N) The detrusor was closed at the original hiatus. (O) The ureteral orifice was formed. PVUR-PL, pneumovesicoscopic ureteral reimplantation using the Politano-Leadbetter. - Relocation of the ureter proximally behind the bladder: a new proximal ureteral hiatus was created at a distance approximately five times the ureteral caliber (1:5 ratio) proximal to the original ureteral orifice. A silicone tube was inserted into the bladder through the urethra and attached to the distal ureter (Figure 2B). External manipulation of the silicone tube enabled visualization of the ureter’s path behind the bladder (Figure 2C), and use anatomical landmarks, such as characteristic retrovesical extraperitoneal tissues (Figure 2D) and vas deferens (Figure 2F), could aid identification and proximal relocation of the ureter through the new hiatus (Figure 2G,2H).
- Submucosal tunnel formation: dissection commenced between the mucosal and detrusor layers at the new hiatus, creating a sufficiently wide tunnel for the ureter. Mucosa and muscle layers were clamped together when necessary to avoid mucosal tearing (Figure 2I).
- Ureteral orifice fixation: the ureter was repositioned through the submucosal tunnel to its original orifice without twisting, and fixed to the detrusor muscle with sutures. Two additional sutures secured the detrusor muscle around the ureter at the new hiatus, positioned at different horizontal planes to prevent lateral traction (Figure 2J,2K).
- Closure of the proximal defect: the proximal detrusor defect was carefully sutured to ensure closure, minimizing the risk of bladder diverticulum formation (Figure 2L,2M).
- Original hiatus closure and ureteral orifice reconstruction: the original hiatus was sutured, and the ureteral orifice was reconstructed appropriately (Figure 2N,2O).
- The ureteral stent was left indwelling, and the skin incision was closed (Figure 1I).
Statistical analysis
Categorical variables were analyzed using Fisher’s exact test and were presented as frequencies with percentages [n (%)], while continuous variables were compared with Student’s t-test and expressed as mean ± standard deviation (SD). All statistical analyses were performed using IBM SPSS software (version 25.0), with statistical significance defined as P<0.05.
Results
A total of 25 patients underwent PVUR-PL, with no loss to follow-up (Table 1) (20). Ten patients received traditional PVUR-PL, and 15 underwent modified PVUR-PL utilizing our technique. In the traditional group, 6 cases had VUR (3 unilateral, 3 bilateral) and 4 had UVJO (2 unilateral, 2 bilateral), including one case with ipsilateral duplex kidney and ureteral cyst. The modified group comprised 5 VUR cases (3 unilateral, 2 bilateral) and 10 UVJO cases (9 unilateral, 1 bilateral), including one with ipsilateral bladder diverticulum. The youngest patient in the traditional group was 11 months old [bladder capacity: 90 mL; maximum BMI: 21.4 kg/m2 (normal range)]. With the modified technique, PVUR-PL was performed in infants as young as 8 months [bladder capacity: 75 mL; maximum BMI: 26.9 kg/m2 (overweight)].
Table 1
| Characteristics | Traditional group (n=10) | Modified group (n=15) | P value |
|---|---|---|---|
| Age (years) | 6.89±4.29 | 5.69±3.85 | 0.47 |
| Gender | 0.43 | ||
| Male | 4 | 9 | |
| Female | 6 | 6 | |
| Bladder capacity (mL) | 249.5±140.56 | 195.33±110.30 | 0.29 |
| Minimum bladder capacity (mL) | 90 | 75 | |
| BMI (kg/m2) | 16.06±2.98 | 17.69±3.15 | 0.21 |
| Maximum BMI (kg/m2) | 21.4 | 26.9 | |
| Side | – | ||
| Right | 1 | 5 | |
| Left | 4 | 7 | |
| Bilateral | 5 | 3 | |
| Total number of ureters | 15 | 18 | – |
| VUR (cases) | 6 | 5 | – |
| Right | 1 | 2 | |
| Left | 2 | 1 | |
| Bilateral | 3 | 2 | |
| Total | 9 | 7 | |
| VUR grade | – | ||
| III | 3 | 2 | |
| IV | 4 | 4 | |
| V | 2 | 1 | |
| UVJO (cases) | 4 | 10 | – |
| Right | 0 | 3 | |
| Left | 2 | 6 | |
| Bilateral | 2 | 1 | |
| Total | 6 | 11 |
Data are presented as mean ± SD or n. VUR grades according to the International Reflux Study Committee (20). BMI, body mass index; SD, standard deviation; UVJO, ureterovesical junction obstruction; VUR, vesicoureteral reflux.
For unilateral procedures, mean operative time was significantly shorter in the modified group (157.73±15.33 vs. 188.90±26.55 min; P=0.01). Bilateral procedures also showed reduced operative time (230.00±27.07 vs. 280.25±16.46 min; P=0.02) (Table 2) (21).
Table 2
| Traditional group (n=10) | Modified group (n=15) | P value | |
|---|---|---|---|
| Operation time (min) | |||
| For unilateral cases | 188.90±26.55 | 157.73±15.33 | 0.01 |
| For bilateral cases | 280.25±16.46 | 230.00±27.07 | 0.02 |
| Postoperative pain score | 4.20±1.23 | 2.93±1.03 | 0.01 |
| Postoperative hematuria (days) | 5.15±1.29 | 2.97±0.74 | <0.001 |
| Postoperative febrile UTI | 0 | 0 | – |
| Peritoneum perforated | 3 | 0 | 0.052 |
Data are presented as mean ± SD or n. Postoperative pain score, assessed using FLACC and VAS methods (ESPA Pain Guidelines 2022) (21). ESPA, European Society for Paediatric Anaesthesiology; FLACC, Face, Legs, Activity, Cry, Consolability; SD, standard deviation; UTI, urinary tract infection; VAS, visual analogue scale.
No severe complications occurred. Peritoneal perforation during retrovesical ureter identification via the proximal new hiatus occurred in 3 traditional group cases but none in the modified group. Postoperative pain scores (2.93±1.03 vs. 4.20±1.23; P=0.01) and hematuria duration (2.97±0.74 vs. 5.15±1.29 days; P<0.001) were significantly lower in the modified group (Table 2).
No cases of febrile UTI were reported during the follow-up period in either group. Ultrasound examinations performed at 3, 6, and 12 months postoperatively revealed marked improvements in ureteral diameter and hydronephrosis. Cystourethrography (VCUG) was performed approximately 6 months postoperatively to assess for the presence of VUR when indicated. VCUG was performed in 5 of 15 patients in the modified group and 3 of 10 patients in the traditional group, with no evidence of VUR observed in any case.
Discussion
The three primary ureterovesical reimplantation techniques are the Lich-Gregoir, Cohen, and PL procedures. Since its introduction in 2005, PVUR has gained popularity as a minimally invasive surgical approach (9,10,13,17).
The PL technique addresses key limitations associated with the Cohen and Lich-Gregoir methods. The submucosal tunnel created by the PL approach maintains the natural ureteral alignment, facilitating future retrograde ureteroscopy or catheterization. However, the PL technique is more technically demanding compared to the Cohen and Lich-Gregoir techniques. The learning curve is steep and challenging initially, but once mastered, the procedure can be performed with relative ease. The first report on PVUR-PL was published by Soh et al. in 2015 (13), and subsequent studies have demonstrated consistently favorable outcomes. In 2019, Tae et al. confirmed the long-term safety and effectiveness of PVUR-PL, with results comparable to traditional open surgery (22). The same year, Baek et al. introduced a modified PVUR-PL technique for identifying the retrovesical ureter by pulling the distal ureter through a new hiatus without detrusor incision and suture (17). In 2022, Zhao et al. described a novel approach involving a metal probe inserted through the urethra to elevate the ureter and bladder wall, facilitating the creation of the new hiatus and ureter identification (12).
We identified two major challenges in PVUR-PL: establishing the pneumatic bladder trocar channel and locating the retrovesical ureter through the newly created hiatus, particularly in infants with small bladder capacity and obese children with a high BMI. Establishing an effective trocar channel is crucial for successful PVUR-PL but remains inadequately described in existing literature. Based on our experience, we highlight several key considerations:
Patient age and bladder capacity: previous studies recommend pneumovesicoscopic approaches primarily for children over 2 years of age or with bladder capacities exceeding 100–150 mL (22,23). In our traditional group, the youngest patient was 11 months old with approximately 90 mL bladder capacity. With our modified technique, we successfully performed PVUR-PL in three infants aged 8 months, each with a bladder capacity of approximately 75 mL. We conclude that experienced urologists can safely perform PVUR-PL with bladder capacities of 70–80 mL; however, surgeons in the early learning curve should avoid selecting infants with limited bladder capacity as initial cases.
Gas versus saline bladder insufflation: traditionally, the bladder is initially filled with saline under cystoscopic guidance, followed by trocar placement, aspiration of saline, and subsequent CO2 insufflation. In our experience, patients older than 1 year or those with bladder capacities exceeding 100 mL can safely undergo direct CO2 insufflation via cystoscopy, thus eliminating water-gas exchange and shortening operative time. Furthermore, CO2 poses minimal risks in the event of peritoneal perforation. However, for infants younger than 1 year or those with bladder capacities below 100 mL, saline filling is recommended to ensure adequate bladder distension for trocar placement. This approach is particularly crucial for female infants due to their shorter urethra and higher risk of gas leakage, potentially limiting effective bladder expansion.
Tool selection for bladder-abdominal wall adhesion: in younger or normal-weight children, an adhesion area between the bladder and abdominal wall can be established under cystoscopic visualization using a long curved needle, with two fixation sutures placed at each puncture site for stability. In overweight children, percutaneous needle penetration can be challenging; thus, a hooked hernia needle inserted through a small skin incision is preferred to minimize trauma and effectively secure the bladder to the abdominal wall.
Trocar positioning and depth: the bladder in infants and younger children is positioned relatively higher, extending towards the umbilical region and closely covered by peritoneum. Thus, trocar entry points should be placed approximately 2–3 cm below the bladder dome to minimize peritoneal injury. Additionally, trocars should not be inserted excessively deep into the bladder, as excessive trocar length can compromise visualization and reduce operative space, complicating the surgical procedure, especially in patients with smaller bladder capacities.
The following section details the modified PVUR-PL procedure. Although previous studies by Baek et al. (17) and Zhao et al. (12), simplified the PVUR-PL approach, identifying the retrovesical ureter through the newly created hiatus remains technically challenging, especially for novice surgeons. This difficulty stems from limited anatomical understanding of this region and its proximity to structures such as the vas deferens. We outline our modified techniques below, based on initial clinical experience, aimed at facilitating retrovesical ureter identification:
Silicone tube-assisted ureteral localization: following ureteral mobilization, a silicone tube is introduced into the bladder via the urethra and attached to the distal ureter with sutures. Baek et al. introduced a modified PVUR-PL technique for identifying the retrovesical ureter by pulling the distal ureter through a new hiatus without detrusor incision and suture (17), which reduced postoperative edema and inflammation of the detrusor. Our early surgical practice also adopted this approach, but we found that direct traction of the ureter would occupy one operative instrument, which was unfavorable for surgical exposure. Zhao et al. described a novel approach involving a metal probe inserted through the urethra to elevate the ureter and bladder wall, facilitating the creation of the new hiatus and ureter identification (12). However, we found that the efficacy was minimal in children with longer urethras, particularly in male children. In our group, a silicone tube was inserted into the bladder through the urethra and attached to the distal ureter, and repeated external traction and release of the silicone tube clearly reveal the ureteral path, simplifying ureter identification behind the bladder through the newly created hiatus.
Anatomical considerations during detrusor dissection: Baek et al. (17) recommended careful, layer-by-layer opening of the detrusor to prevent peritoneal injury. Our clinical observations indicate that younger children’s detrusor muscles are typically thin and difficult to separate clearly. In older children, the detrusor is thicker and contains abundant intertwined blood vessels, increasing dissection difficulty and the risk of misidentifying tissue planes. Therefore, precise identification of the correct dissection plane between the detrusor muscle and ureteral adventitia is crucial. Upon complete detrusor opening, characteristic retrovesical extraperitoneal tissues—light-yellow adipose tissue and thin, white, loose reticular fascia—become apparent (Figure 2D). Dissection should then extend slightly distal to the new hiatus to prevent inadvertent peritoneal entry. Conversely, unintended detrusor penetration exposes characteristic crisscrossing blood vessels, nerves, and muscle fibers (Figure 2E).
Relationship with the vas deferens: during posterior bladder dissection, the vas deferens occasionally becomes visible. Typically, the ureter is located medial and inferior to the vas deferens (Figure 2F), which serves as a reliable anatomical landmark, aiding safe ureter identification without peritoneal cavity entry.
These modifications expanded the applicability of PVUR-PL, successfully including infants as young as 8 months old (bladder volume ~75 mL) and obese children (maximum BMI of 26.9 kg/m2). Procedures were conducted with relative efficiency within our own cohort and under our specific handling conditions, resulting in a notable decrease in operative times compared to our previous experiences, along with minimal intraoperative bleeding and reduced postoperative pain. Additionally, no cases of peritoneal perforation occurred with this modified technique, and long-term follow-up demonstrated favorable outcomes. We aim to first present the outcomes achieved through this straightforward and feasible modified surgical approach. Moreover, we are eager to share our experiences with others. To solidify and authenticate our research results, it is of utmost significance to enlarge the sample size, employ a prospective study design, maintain uniformity in follow-up practices, engage in multi-center endeavors, and carry out randomized controlled trials (RCTs) in subsequent studies.
Limitations
This study has several limitations. First, the small sample size restricts the generalizability of the findings, and the retrospective design may introduce bias. Second, variable parental compliance led to incomplete follow-up data; notably, some patients lacked postoperative VCUG imaging. We will prioritize obtaining complete VCUG data in future follow-up. Additionally, postoperative urodynamic evaluations were absent due to patient noncompliance, representing a significant gap. Future studies will aim to incorporate urodynamic assessments. Finally, the learning curve effect is a potential limitation, as all procedures were performed by the same surgical team whose evolving experience may have influenced outcomes.
Conclusions
In conclusion, our refined PVUR-PL technique, guided by precise anatomical insights and advanced operative methods, significantly reduces operative time and postoperative complications. This streamlined surgical procedure offers a standardized and easily implementable option for clinicians.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the STROCSS reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-200/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-200/dss
Peer Review File: Available at https://tp.amegroups.com/article/view/10.21037/tp-2025-200/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-2025-200/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. This study was reviewed and approved by the Medical Ethics Committee of Tianjin Children’s Hospital (approval No. 2022-LXKY-010). Written informed consent from the participants’ legal guardian/next of kin was not required in accordance with the national legislation and the institutional requirements.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tekgül S, Riedmiller H, Hoebeke P, et al. EAU guidelines on vesicoureteral reflux in children. Eur Urol 2012;62:534-42. [Crossref] [PubMed]
- Chang J, Zhang Q, Hou P, et al. Comparative Clinical Study Between Modified Ureteral Orthotopic Reimplantation and Cohen Method Under Pneumovesicum in Pediatric Patients With Hydroureteronephrosis. Front Pediatr 2020;8:62. [Crossref] [PubMed]
- Gimpel C, Masioniene L, Djakovic N, et al. Complications and long-term outcome of primary obstructive megaureter in childhood. Pediatr Nephrol 2010;25:1679-86. [Crossref] [PubMed]
- Ranawaka R, Hennayake S. Resolution of primary non-refluxing megaureter: an observational study. J Pediatr Surg 2013;48:380-3. [Crossref] [PubMed]
- Yeung CK, Sihoe JD, Borzi PA. Endoscopic cross-trigonal ureteral reimplantation under carbon dioxide bladder insufflation: a novel technique. J Endourol 2005;19:295-9. [Crossref] [PubMed]
- Canon SJ, Jayanthi VR, Patel AS. Vesicoscopic cross-trigonal ureteral reimplantation: a minimally invasive option for repair of vesicoureteral reflux. J Urol 2007;178:269-73; discussion 273. [Crossref] [PubMed]
- Soulier V, Scalabre AL, Lopez M, et al. Laparoscopic vesico-ureteral reimplantation with Lich-Gregoir approach in children: medium term results of 159 renal units in 117 children. World J Urol 2017;35:1791-8. [Crossref] [PubMed]
- Bustangi N, Kallas Chemaly A, Scalabre A, et al. Extravesical Ureteral Reimplantation Following Lich-Gregoir Technique for the Correction of Vesico-Ureteral Reflux Retrospective Comparative Study Open vs. Laparoscopy. Front Pediatr 2018;6:388. [Crossref] [PubMed]
- Valla JS, Steyaert H, Griffin SJ, et al. Transvesicoscopic Cohen ureteric reimplantation for vesicoureteral reflux in children: a single-centre 5-year experience. J Pediatr Urol 2009;5:466-71. [Crossref] [PubMed]
- Emir H, Mammadov E, Elicevik M, et al. Transvesicoscopic cross-trigonal ureteroneocystostomy in children: a single-center experience. J Pediatr Urol 2012;8:83-6. [Crossref] [PubMed]
- Tae BS, Choi H, Park JY, et al. Laparoscopic Approach for Intravesical Surgery Using Pneumovesicum in Urology: Literature Review. Int Neurourol J 2018;22:S10-22. [Crossref] [PubMed]
- Zhao X, Tian Q, Fang E, et al. Use of Urethral Sound to Facilitate Locating Retrovesical Ureter for Politano-Leadbetter Pneumovesicoscopic Ureteral Reimplantation. Front Pediatr 2022;10:834465. [Crossref] [PubMed]
- Soh S, Kobori Y, Shin T, et al. Transvesicoscopic ureteral reimplantation: Politano-Leadbetter versus Cohen technique. Int J Urol 2015;22:394-9. [Crossref] [PubMed]
- Hong CH, Kim JH, Jung HJ, et al. Single-surgeon experience with transvesicoscopic ureteral reimplantation in children with vesicoureteral reflux. Urology 2011;77:1465-9. [Crossref] [PubMed]
- David S, Kelly C, Poppas DP. Nerve sparing extravesical repair of bilateral vesicoureteral reflux: description of technique and evaluation of urinary retention. J Urol 2004;172:1617-20; discussion 1620. [Crossref] [PubMed]
- Leissner J, Allhoff EP, Wolff W, et al. The pelvic plexus and antireflux surgery: topographical findings and clinical consequences. J Urol 2001;165:1652-5.
- Baek M, Han DH. Transvesicoscopic Politano-Leadbetter ureteral reimplantation in children with vesicoureteral reflux: A novel surgical technique. Investig Clin Urol 2019;60:405-11. [Crossref] [PubMed]
- Kruppa C, Fitze G, Schuchardt K. Vesicoscopic Cross-Trigonal Ureteral Reimplantation for Vesicoureteral Reflux: Intermediate Results. Children (Basel) 2022;9:298. [Crossref] [PubMed]
- Koff SA. Estimating bladder capacity in children. Urology 1983;21:248. [Crossref] [PubMed]
- Medical versus surgical treatment of primary vesicoureteral reflux: report of the International Reflux Study Committee. Pediatrics 1981;67:392-400.
- ESPA Pain Task Force. Procedural and Postoperative Pain in Children: Clinical Practice Recommendations. Pediatr Anesth 2021;31:S9-24.
- Tae BS, Jeon BJ, Choi H, et al. Comparison of open and pneumovesical approaches for Politano-Leadbetter ureteric reimplantation: a single-center long-term follow-up study. J Pediatr Urol 2019;15:513.e1-7. [Crossref] [PubMed]
- Choi H, Park JY, Bae JH. Initial experiences of laparoscopic intravesical detrusorraphy using the Politano-Leadbetter technique. J Pediatr Urol 2016;12:110.e1-7. [Crossref] [PubMed]