Role of a registered dietitian in pediatric type 1 and type 2 diabetes
Introduction
Diabetes mellitus is a disease in which blood glucose levels are above normal range. In order to help prevent acute and chronic complications that can accompany uncontrolled diabetes, close follow up from a diabetes care team is necessary. The medical team often may need to address outside or social factors influencing the individual’s ability to successfully manage this complex, chronic disease (1). A multidisciplinary team comprised of various health professionals specializing in diabetes care is essential to provide support for patients and families. Specifically, registered dietitians (RD) are a critical part of the multidisciplinary team and provide diabetes-focused nutrition education and counseling.
There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune condition where the body does not make the hormone insulin. Subcutaneous insulin is the only treatment to manage blood glucose. This condition typically presents in children and young adults. In pediatrics, more than 18,000 youth were diagnosed each year in 2008 and 2009 with type 1 diabetes (1). In type 2 diabetes, the body is unable to use insulin well or is unable to produce enough insulin to overcome insulin resistance. While type 2 diabetes is the most common type of diabetes in adults, prevalence in pediatrics is increasing rapidly. In pediatrics, more than 5,000 youth are diagnosed with type 2 diabetes each year (2). The TODAY study showed obesity is a key factor in the development of type 2 diabetes in youth. Obesity seen in children and adolescents is also linked to increased rates of diabetes as this population ages into adulthood (3). Other strong risk factors for developing type 2 diabetes include family history of diabetes, minority ethnic groups, female gender and conditions associated with insulin resistance, such as acanthosis nigricans (1). Adolescents with type 2 diabetes in the U.S. often come from families with greater socioeconomic disparity (3). Due to the increasing incidence of type 2 diabetes in the pediatric population, the American Diabetes Association (ADA) recommends screening high-risk, asymptomatic children starting at 10 years of age or onset of puberty (4).
Food and nutrition play an important role in management of blood sugars for people with diabetes. Carbohydrates, a macronutrient found in many foods, including grains, vegetables, fruits, dairy and sweets, are a primary component of rapid blood sugar rises during the day (5). Carbohydrates break down into glucose when digested, which is then absorbed through the small intestine to the bloodstream. When the body does not make enough (or any) insulin, glucose stays in the bloodstream and cannot reach the cells, resulting in elevated blood sugars. For optimal management of type 1 or type 2 diabetes, patients may be required to dose insulin based on pre-prandial blood glucose and carbohydrate content of their meals (5). This regimen is known as carbohydrate counting and allows flexibility in meal pattern and portion sizes.
Pediatric diabetes patients require very specialized care due to a need for frequent changes in insulin doses during periods of growth and development and gradual transition to independent diabetes care during adolescence (6). Goals for optimal diabetes management are individualized for patients and family. Diabetes self-management education (DSME) and support (DSMS), medical nutrition therapy (MNT), and psychosocial support are essential beginning at diagnosis and as the child ages.
When a patient is diagnosed with diabetes, there can be many challenges that affect clinical outcomes for optimal diabetes management. For pediatric patients, diabetes affects the entire family as children need constant support and supervision in all aspects of care. Children will require caregivers at home, school and events to ensure they are safe with diabetes care. Many times, medical teams are relying on these caregivers to prepare healthy meals, provide a structured meal pattern and encourage children to participate in physical activities. These caregivers are the role models for creating healthy lifelong habits and adjusting to life with diabetes (5).
DSME is critical to prevent serious short and long term health consequences that may result from both type 1 and type 2 diabetes if poorly controlled. In the short term or acute stage, hyperglycemia can cause symptoms of polydipsia, polyuria, polyphagia, fatigue, blurred vision, numbness or tingling in the feet or hands, as well as unintentional weight loss. This weight loss results from the inability to use glucose for energy, leading to the breakdown of fat as a secondary source of fuel. When fats are metabolized they form ketones, which cause the blood to become acidic as they accumulate. If untreated, this may result in diabetic ketoacidosis, which can be life-threatening (7). Long-term complications of hyperglycemia include a higher risk of stroke, heart disease, kidney disease, retinopathy, dental disease, nerve damage and foot problems. In contrast, acute hypoglycemic symptoms can vary person to person, but the affected individual may feel shaky, hungry, sweaty, confused or disoriented, fatigued, weak, or irritable. If untreated, severe hypoglycemia may result in seizures, convulsions or unconsciousness (8). Having a good understanding of diabetes management, including how to correctly calculate insulin doses for meals and snacks, may reduce occurrences of hyper- and hypoglycemia.
Nutrition-related comorbidities associated with hyperglycemia and obesity include dyslipidemia, hypertension, and nephropathy. The American Diabetes Association (ADA) Standards of Diabetes Care specifically addresses each of these related to the pediatric population (6). In children with type 2 diabetes, these comorbidities may already be present at diagnosis and should therefore be monitored at the time diabetes diagnosis is confirmed. At the beginning of the TODAY study, 10% of adolescents with type 2 diabetes already had high triglycerides, 80% had low HDL levels, and 13% had elevated microalbuminuria (9). While not related to glycemic control, monitoring for non-alcoholic hepatic steatosis is also crucial in obese youth with type 1 or type 2 diabetes. In type 2 diabetes in particular, fatty liver disease appears to progress more rapidly (3).
The American Heart Association (AHA) categorizes children with type 1 diabetes at higher risk for cardiovascular disease. Guidelines suggest screening fasting lipids in children 10 years and older as soon as glucose control is achieved after initial diagnosis. If levels are at goal (LDL-cholesterol <100 mg/dL), subsequent screening every three to five years is appropriate. However, if abnormal, lipids should be monitored annually. There is evidence that atherosclerosis may begin in childhood; therefore, interventions for dyslipidemia should be implemented as soon as abnormalities are detected. Treatment for elevated lipids would include MNT for the AHA Step 2 diet, which aims to decrease intake of saturated fats and cholesterol. If lipids remain high despite dietary intervention, a statin would be recommended as pharmacologic treatment (6).
Blood pressure should be monitored at each routine clinic visit. If confirmed high on three separate days, dietary modification of sodium intake, increased physical activity and weight management, if applicable, would be first line therapy for hypertension. If blood pressure remains above target 3–6 months after initiating lifestyle modifications, pharmacological treatment with either an ACE inhibitor or angiotensin receptor blocker is indicated (6). In general, hypertension is more common in children with type 2 versus type 1 diabetes, likely due in part to its positive correlation with high body mass index (BMI) (2).
For children with type 1 diabetes, annual screening for nephropathy should begin five years after initial diabetes diagnosis. For children with type 2 diabetes, nephropathy screening should be done at diagnosis and annually thereafter. If urine albumin-to-creatinine ratio is elevated and confirmed with two to three urine samples, treatment would include an ACE inhibitor (3). Microalbuminuria also has higher prevalence in youth with type 2 diabetes and incidence increases significantly with poor diabetes control (2). If kidney damage does occur, a modified-protein diet may be indicated to help prevent further damage (10).
Diabetes-related complications should be taken seriously from the onset of diagnosis. The Canadian First Nations youth with type 2 diabetes showed renal and neurological complications began to manifest within 5 years of diabetes diagnosis and major complications, such as amputation, began 10 years after diagnosis (3). As children with type 2 diabetes are being diagnosed at younger ages, it is imperative for nutrition professionals to help these families understand the role good glycemic control and weight management play in helping to avoid negative health outcomes.
An RD is a food and nutrition expert who has met academic and professional requirements to practice, including completion of a bachelor’s degree program approved by the Academy of Nutrition and Dietetics’ Accreditation Council for Education in Nutrition and Dietetics (ACEND), 1,200 hours of supervised practice and a national examination by the Commission on Dietetic Registration. RDs must complete continuing education requirements to maintain registration and licensure throughout their careers (11). MNT is a process used by dietitians to deliver individualized nutrition recommendations and help patients achieve specific treatment goals (12). The dietitian uses MNT, Motivational Interviewing and realistic goal setting to help patients realize how dietary and lifestyle choices impact overall health. A nutrition assessment includes evaluation of nutrition-related history, biochemical data, anthropometric measurements, nutrition-focused physical findings and client history. Then, a nutrition diagnosis identifies and defines any nutrition-related issues and helps drive nutrition intervention. Finally, it is important to monitor and evaluate the patient’s progress and whether the nutrition interventions are contributing to the desired outcome. Goals and interventions are routinely evaluated and revised based on patient’s progress (13).
RDs play a role in diabetes care by routinely assessing nutritional status, quality of diet and supporting weight management (10). An RD with experience in diabetes management is most qualified to provide carbohydrate counting education. Dietitians can provide counseling to patients and families on how dietary and lifestyle choices impact blood sugar control and other nutrition-related comorbidities. Diabetes education and nutrition counseling from an RD is an essential component of the multidisciplinary approach. A literature review was completed to determine the role of the RD in achieving improved clinical parameters to prevent, delay and manage diabetes complications.
Materials and methods
A literature review was conducted using MeSH terms: Diabetes Mellitus, Type 1; Diabetes Mellitus, Type 2; Nutritionists; Diet Therapy; Pediatrics and Endocrinology. A total of 21 sources were reviewed, including randomized, controlled trials as well as clinical guidelines and review articles published within the last 22 years. These references were analyzed by all team members. The primary objective was to determine the value of the dietitian, as part of the multidisciplinary team, in improving diabetes control and reducing the risk of diabetes-related complications in the pediatric population.
Results
Thorough review of related articles shows RD involvement reduces long-term complications of diabetes and positively impacts weight status. The decline in beta-cell function and onset of diabetes-related complications is accelerated in adolescents with type 2 diabetes compared to adults (2,3,9). MNT can be used to help prevent these processes, thus emphasizing the importance of nutrition-related diabetes education. Behavior modification programs that include a nutrition component have improved BMI, total cholesterol and insulin resistance in children who did not have diabetes (3). The diabetes prevention program (DPP) showed that type 2 diabetes can be delayed or prevented in adults with implementation of lifestyle modification groups led by RD coaches. These RDs used counseling and problem solving with participants to promote behavior change. This intensive lifestyle intervention produced a 58% reduction in development of type 2 diabetes versus placebo, which was above and beyond the results seen in the study group taking oral medication alone (14).
Studies have demonstrated that providing MNT to diabetes patients improves glycemic outcomes and significantly decreases hemoglobin A1c (HbA1c) (10,15), which was then able to be maintained over the course of a year (10). A significant improvement was seen in HbA1c after 12 weeks with a nutrition counseling program (12), while another study also showed improved insulin sensitivity in adults with type 2 diabetes. These findings suggest that positive lifestyle changes result from continuous education provided by an RD, possibly related to recommendations such as higher consumption of fiber-rich foods and daily physical activity (16).
For patients with type 1 diabetes, calculating mealtime insulin dose to match planned carbohydrate intake at meals leads to improved glycemic control and quality of life (10). These results can likely be replicated for patients with type 2 diabetes who also calculate mealtime insulin based on carbohydrate intake. This education is often provided by an RD specializing in diabetes. Any level of diabetes education provided by the RD resulted in improved glycemic control compared with a group that had no RD intervention (17).
Improving glycemic control leads to other health benefits, such as an improvement in lipid levels (18). Studies have demonstrated an additional correlation between dietary counseling and improvement in lipid panel, particularly in lowering triglycerides and LDL-cholesterol and increasing HDL-cholesterol (12,15,19). There is conclusive evidence that high fiber diets have been shown to lower cholesterol compared to low fiber diets (10). Dietary counseling to increase fiber intake helped improve lipid levels to goals set by the ADA for children with type 1 diabetes (19). In addition, counseling by an RD achieved greater reductions in LDL-cholesterol than did that given by other health professionals, including medical doctors (20). Nutrition counseling for cardiovascular disease may have the most impact on lipid panel in the first three to six months, although on-going support from an RD may provide additional accountability to help patients maintain lifestyle changes and long-term improvement in cholesterol levels (10).
The irony of weight management in type 2 diabetes is that improved glycemic control achieved through compliance with insulin regimen can result in weight gain. In a review of randomized controlled trials evaluating lifestyle interventions for overweight patients with type 2 diabetes, a loss of at least five percent total body weight produced beneficial effects on lipids, HbA1c and blood pressure. Studies involving RD-led nutrition counseling helped maintain this weight loss at 12 months (15). Additionally, a 12-week nutrition counseling program demonstrated improvements in body weight, BMI and waist circumference (12). Adults with type 2 diabetes who had RD-led case management intervention lost more weight, had greater reduction in waist circumference, took fewer prescription medications and reported improved quality of life compared to non-RD case managers (21). Having patients meet with a dietitian has also been shown to provide benefits in glycemic control and weight loss above DSME alone, although not statistically significant (10,15).
The type of nutrition education program may also play a role in the success of MNT. Managing type 2 diabetes with structured group education produced better results than the traditional one-to-one approach. Utilizing RDs as the facilitators of these groups may offer a cost-effective approach to providing this type of care (16). Moreover, beneficial effects of dietary changes and improved diabetes control may be even greater with an activity component included (21). In addition to benefits seen in glycemic control, lipid levels and weight management resulting from MNT, RD involvement also decreases hospital admissions and health care costs (10,15).
Discussion
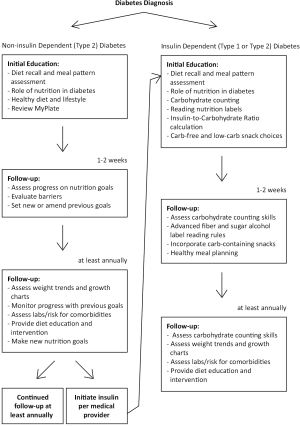
Based on best patient practices outlined in recent research, RDs in the section of endocrinology at a large, free-standing pediatric facility aim to be an integrative part of a multidisciplinary team. The dietitian meets routinely with patients throughout the course of their diabetes treatment, including initial education and a series of follow up visits (see Figure 1). The nutrition concepts discussed at diagnosis are dependent upon whether insulin initiation is indicated. However, the majority of patients seen at our institution require insulin therapy. Topics discussed by the RD include carbohydrate counting, dosing insulin at meals, appropriate meal pattern and general healthy eating tips. At initial education, a diet recall helps identify areas of opportunity for nutrition intervention. The RD assesses overall diet quality and monitors if patients are skipping meals, drinking sugar-sweetened beverages and consuming age-appropriate portions. These sugary beverages, such as sports drinks, regular soda, sweet tea or fruit punch, are the only items discouraged by the RD. Children who have diabetes are otherwise encouraged to consume healthy, well-balanced diets just like their peers. During carbohydrate counting education, food models are used as a visual representation and help to reinforce importance of measuring portions. Caregivers and the patient, if developmentally appropriate, are asked to participate in hands-on teaching to practice counting carbohydrates in sample meals, reading nutrition labels and calculating meal time insulin doses based on an insulin-to-carbohydrate ratio (ICR). Families are given handouts with both words and pictures to accommodate different learning styles. A Calorie King® book is provided to each patient at diagnosis to use as a tool to help count carbohydrates in fresh fruits and vegetables, which will not have food labels. This is also a beneficial reference to use when dining out. Recommendations are given for other apps and websites that may be helpful for carbohydrate counting. Initially, patients are encouraged to choose low-carbohydrate snacks or “free foods” that would not require insulin during the initial adjustment phase. An extensive list of low-carbohydrate snack choices is provided to help alleviate stress. However, RDs do recommend low-fat “free foods” to prevent excess weight gain. For example, deli turkey would be a more preferable choice than bologna.
An RD and a diabetes nurse educator meet with the patient again within the next 1 to 2 weeks to assess how the family is adjusting and understanding their new routine for diabetes care. At this visit, the dietitian reviews more complex management concepts including healthy meal planning, appropriate snacking and advanced food label reading in regards to fiber and sugar alcohols based on ADA guidelines. If the family has adjusted well to insulin dosing and glucose levels are more stable, the RD will instruct them on how to dose insulin for carbohydrate-containing snacks. Healthy, satiating snacks that include fiber and protein are encouraged. However, patients may prefer to continue with low-carb snack options to limit the number of injections required per day. The RD will then plan to meet with patients and their families annually, at minimum, in outpatient clinic in accordance with ADA recommendations.
At routine outpatient clinic visits with an RD, MNT is individualized based on patient and family concerns or needs. The dietitian gathers and interprets data in regards to intake patterns and the correlation to blood sugar trends. Visits begin by collecting a diet recall, including portion sizes consumed and carbohydrate content of some of these items. This detailed information helps the RD to identify deficits in carb counting skills, understand a patient’s daily meal and activity schedule and gain insight into cultural or food preferences. Follow-up questions, such as if insulin is given for all carbohydrate-containing meals and snacks and whether this is done before or after eating, may provide insight into the patient’s understanding of diabetes management and help identify concerns for the diabetes team to address. Secondary to assessment of diabetes control and carbohydrate counting knowledge, the RD assesses growth charts and weight trends, as well as overall quality of dietary intake. The dietitian helps identify if poor weight gain is correlated to suboptimal glucose control or inadequate caloric intake. Diabetes-specific nutrition instruction may include topics such as acceptable carbohydrate sources for treating versus preventing hypoglycemia. The RD will provide a variety of handouts and visual education tools as needed.
General nutrition education may include discussion of age-appropriate diet and tips for handling selective eating habits. The United States Department of Agriculture MyPlate is a visual resource commonly used to educate families on ideal portion sizes and nutrient-dense choices from each food group. This tool is widely used for weight management and guidance for healthy eating, but it is often necessary to compromise on goals that are more realistic and individualized to the patient based on their family’s available resources. For example, if diet recall reveals minimal fruit and vegetable intake, but food budget is limited, the dietitian may suggest a goal of eating one serving of canned, fresh or frozen fruits and vegetables per day. A nutrition appointment for a patient with prediabetes or diabetes not requiring insulin therapy may have a much larger focus on weight management and lifestyle interventions to improve endogenous insulin sensitivity.
As previously mentioned, patients with diabetes often have a higher risk of nutrition-related comorbidities such as dyslipidemia, obesity, and hypertension. Thus, the role of the RD is also to regularly assess vitals such as blood pressure, weight, BMI and labs such as lipid levels and HbA1c. If irregularities in these parameters occur, the dietitian will provide focused MNT and counseling to help patients work towards a healthier lifestyle and improve nutrition-related measures. As progress is monitored and evaluated over time, the RD amends or gives additional strategies to help overcome barriers and advance a nutrition goal. Most often, providers will have families meet with an RD for nutrition counseling prior to starting medications to lower cholesterol or blood pressure. In this case, the dietitian would provide individualized instruction on ways to lower saturated fat, dietary cholesterol and sodium intake.
There are many challenges in nutrition and diabetes practice, such as the lack of evidence for an established diet or distribution of macronutrients effective in managing diabetes. There is also much conflicting evidence on effectiveness (in terms of improved HbA1c levels) of a low-glycemic index diet. Many families may be overtly aware or avoidant of carbohydrates after receiving initial education, resulting in restrictive behaviors. These may subsequently lead to an inability to maintain appropriate growth and development secondary to insufficient energy, vitamins, minerals and fiber (10). Other patients may consume excessive carbohydrates, increasing the likelihood of weight gain, insulin resistance and other weight-related comorbidities. Patients who eat frequently throughout the day or have multiple servings at meals may require education on why this meal pattern is not ideal for healthy eating or good blood sugar control. In particular, patients who start on insulin pump therapy may be more inclined to frequent snacking or grazing due to the ease of insulin delivery. If weight management is a concern and diet recall reveals excessive carbohydrate intake, the dietitian may provide a maximum goal for carbohydrate intake at meals as a way to provide portion control and limit overall caloric intake. If needed, the RD can provide closer follow-up for families and is available whenever additional nutrition-related questions or concerns arise.
The RD collaborates and works closely with all other members of the diabetes care team in a multidisciplinary clinic model. Throughout a year, patients and families will also meet with a pediatric endocrinologist, advanced practitioner, diabetes nurse educator, and social worker. Additional referrals are available as needed, such as psychology or nephrology. This collaborative and multidisciplinary approach makes the clinic visit more efficient, thorough, and individualized to the needs of the patient and family.
There were limitations identified in the literature review. For example, most studies were conducted with adult participants. Many of the nutrition counseling programs reviewed involved weekly to monthly contact with a dietitian, which may not be feasible in a routine clinic model. Conducting on-going group education may be limited by staffing and space accommodations. Also, few studies are available that specifically focus on the RD role in diabetes management in a pediatric population. However, research shows that diabetes complications occur more rapidly in this population (3). Therefore, the results of these studies should be applicable to all age groups and RD involvement may be even more critical for pediatric patients for this reason. Studies have shown that meeting with an RD, at any frequency, for routine diabetes care positively impacts patient outcomes compared with patients who had no RD intervention (17).
Given the important role of MNT in optimal diabetes care, a dietitian is a crucial member of the multidisciplinary team. Nutrition education on carbohydrate counting is standard practice for patients taking mealtime insulin and should be provided by a dietitian specializing in diabetes care. Dietitians can provide dietary education that is individualized to specific patient needs. Having an RD as part of the diabetes care team helps improve glycemic control, decreases risk of long-term complications and aids in weight management. In any diabetes care setting, dietitians are a valuable resource on the diabetes team and help provide comprehensive and ongoing disease management to patients and their families.
Acknowledgements
We would like the thank Manmohan Kamboj, MD, Associate Professor and Interim Division Chief of the Section of Endocrinology at Nationwide Children’s Hospital in Columbus, Ohio for guidance in this review.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Diabetes Report Card 2014 [Internet]. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2015 [cited 2017 June 30]. Available online: https://www.cdc.gov/diabetes/pdfs/library/diabetesreportcard2014.pdf
- Folsom LJ, Hannon TS. Collaboration Is Key for Successful Treatment of Youth-Onset Type 2 Diabetes. J Adolesc Health 2017;60:360-2. [Crossref] [PubMed]
- Nadeau KJ, Anderson BJ, Berg EG, et al. Youth-Onset Type 2 Diabetes Consensus Report: Current Status, Challenges, and Priorities. Diabetes Care 2016;39:1635-42. [Crossref] [PubMed]
- Classification and Diagnosis of Diabetes. Diabetes Care 2017;40:S11-24. [Crossref] [PubMed]
- Silverstein J, Klingensmith G, Copeland K, et al. Care of Children and Adolescents With Type 1 Diabetes. A statement of the American Diabetes Association 2005;28:186-212.
- American Diabetes Association. 12. Children and Adolescents. Diabetes Care 2017;40:S105-13. [Crossref] [PubMed]
- American Diabetes Association. Hyperglycemia (High Blood Glucose) [Internet]. Arlington, VA: American Diabetes Association; 2014 [cited 2017 June 30]. Available online: http://www.diabetes.org/living-with-diabetes/treatment-and-care/blood-glucose-control/hyperglycemia.html
- American Diabetes Association. 6. Glycemic Targets. Diabetes Care 2017;40:S48-56. [Crossref] [PubMed]
- Narasimhan S, Weinstock RS. Youth-onset type 2 diabetes mellitus: lessons learned from the TODAY study. Mayo Clin Proc 2014;89:806-16. [Crossref] [PubMed]
- Franz MJ, Powers MA, Leontos C, et al. The evidence for medical nutrition therapy for type 1 and type 2 diabetes in adults. J Am Diet Assoc 2010;110:1852-89. [Crossref] [PubMed]
- Academy of Nutrition and Dietetics (US). Qualifications of a Registered Dietitian Nutritionist [Internet]. Chicago, IL: Academy of Nutrition and Dietetics; 2014 [cited 2017 June 30]. Available online: http://www.eatright.org/resource/food/resources/learn-more-about-rdns/qualifications-of-a-registered-dietitian-nutritionist
- Barakatun Nisak MY, Ruzita AT, Norimah AK, et al. Medical nutrition therapy administered by a dietitian yields favourable diabetes outcomes in individual with type 2 diabetes mellitus. Med J Malaysia 2013;68:18-23. [PubMed]
- Academy of Nutrition and Dietetics (US). Nutrition Care Process [Internet]. Chicago, IL: Academy of Nutrition and Dietetics; [cited 2017 June 30]. Available online: http://www.eatrightpro.org/resources/practice/practice-resources/nutrition-care-process
- Wylie-Rosett J, Delahanty L. An integral role of the dietitian: implications of the Diabetes Prevention Program. J Am Diet Assoc 2002;102:1065-8. [Crossref] [PubMed]
- Marincic PZ, Hardin A, Salazar MV, et al. Diabetes Self-Management Education and Medical Nutrition Therapy Improve Patient Outcomes: A Pilot Study Documenting the Efficacy of Registered Dietitian Nutritionist Interventions through Retrospective Chart Review. J Acad Nutr Diet 2017;117:1254-64. [Crossref] [PubMed]
- Trento M, Basile M, Borgo E, et al. A randomised controlled clinical trial of nurse-, dietitian- and pedagogist-led Group Care for the management of Type 2 diabetes. J Endocrinol Invest 2008;31:1038-42. [Crossref] [PubMed]
- Franz MJ, Monk A, Barry B, et al. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J Am Diet Assoc 1995;95:1009-17. [Crossref] [PubMed]
- Petitti DB, Imperatore G, Palla SL, et al. Serum lipids and glucose control: The search for diabetes in youth study. Arch Pediatr Adolesc Med 2007;161:159-65. [Crossref] [PubMed]
- Cadario F, Prodam F, Pasqualicchio S, et al. Lipid profile and nutritional intake in children and adolescents with Type 1 diabetes improve after a structured dietician training to a Mediterranean-style diet. J Endocrinol Invest 2012;35:160-8. [PubMed]
- Nutrition Subcommittee of the Diabetes Care Advisory Committee of Diabetes UK. The implementation of nutritional advice for people with diabetes. Diabetic Medicine 2003;20:786-807. [Crossref] [PubMed]
- Wolf AM, Conaway MR, Crowther JQ, et al. Translating lifestyle intervention to practice in obese patients with type 2 diabetes: Improving Control with Activity and Nutrition (ICAN) study. Diabetes Care 2004;27:1570-6. [Crossref] [PubMed]