Going back to the ward—transitioning care back to the ward team
Introduction
Transition of care, defined as admission to, transfer between, or discharge from a healthcare facility or hospital ward, places the patient at risk for experiencing medical error and increases feelings of uncertainty, stress and anxiety in patients and families (1-3). One particularly challenging transition of care is the transfer from the intensive care unit (ICU) to the ward. This transition typically occurs when patients are clinically recovering from a critical illness, yet require ongoing acute inpatient care. While the patient usually remains in the same healthcare facility, there is often a change in the care team. The ward physicians, nurses, pharmacists, social workers (SWs), and care managers may be less familiar with the details of the patient’s initial presentation and course of their critical illness. Furthermore, care protocols and patient monitoring on the wards are usually different from the ICU, which can contribute to caregiver uncertainty and anxiety (4). Studies in adults transitioning from the ICU to the ward suggest that this transition can be associated with incomplete or inaccurate physician handoffs and medication reconciliation errors (5-8). Inconsistencies may be exacerbated by delayed or night-time discharges. Furthermore, patients with chronic illness, particularly those with new technology dependence after discharge, are at increased risk for medical errors, prolonged hospitalization and ICU readmissions.
This review article highlights the various challenges associated with transition from the ICU to the ward, identifies gaps in the pediatric literature on this topic, and discusses some potential interventions and strategies to decrease medical error, strain, and caregiver stress during this transition.
Physician handoffs from ICU to ward team
The handoff of patient care between medical providers is an important component of a comprehensive transition of care from the ICU to the ward. The National Academy of Science (formerly Institute of Medicine) highlights effective communication among providers, particularly at vulnerable times like care transitions, as an important aspect of safe, timely, and effective care (9). Details of the physician handoff process should be carefully considered, including which providers should be involved, when the handoff should occur, key content that can be communicated efficiently, and documentation requirements.
Inconsistencies with handoffs
Studies in adult and pediatric patients reveal inconsistencies in providing effective handoffs prior to transition of care from the ICU to ward team. In a prospective study of ten Canadian hospitals, the mean agreement of patient issues between last ICU note and first ward note was only 42% (6), indicating gaps in communication between teams. Similarly, at a large pediatric institution, reliable verbal resident handoff was lacking from the ICU to ward team, with only 76% of patients having completed physician handoff prior to transfer (5). To address this inconsistency, a multidisciplinary team used quality improvement methods to drive the implementation of a standardized, reliable process with interventions including: education regarding the value of an effective handoff, creation of an electronic health record (EHR) template to drive communication, and feedback to providers. Through these efforts, handoff between providers rose to 100%, ensuring that every child leaving the ICU would be met by a receiving team that was familiar with the care plan (5).
Handoff tools
The Center of Excellence on Quality of Care Measures for Children with Complex Needs suggest that transition notes should include two key elements: comprehensive problem lists and treatment plans for each problem (2). The use of EHR templates can drive standard documentation practice at time of transition (5). A validated handoff tool should be considered to ensure key elements are not missed. One such tool that is used at many pediatric institutions nationwide is the I-PASS mnemonic, which includes the following elements: Illness severity, Patient summary, Action list, Situation awareness and contingency plans, and Synthesis by receiver (10). In a multi-center study, the I-PASS handoff tool was associated with a significant decrease in medical errors and preventable adverse events (10). Furthermore, I-PASS has been successfully applied to ICU-to-ward team transitions in pediatric patients (5,11). In one such study, the incorporation of the I-PASS mnemonic in provider handoff between a cardiac ICU (CICU) and the ward team led to more timely and efficient handoffs, improved safety culture survey results, and improved provider and family satisfaction with information conveyed (11).
Medication reconciliation
Medication reconciliation is another aspect of the care transition in which preventable errors may occur. In 2005, the Joint Commission designated inpatient medication reconciliation as a national patient safety goal to reduce medication related errors and adverse events (1). The commission identified transitions of care as an independent risk factor for medication related errors (1).
Medication errors
An ICU stay can increase the risk of incorrect medication reconciliation. Critically ill patients are often initiated on new classes of medications (e.g., respiratory treatments, stress ulcer prophylaxis) upon admission to the ICU while their chronic home medications are temporarily discontinued. Furthermore, ward physicians caring for patients recovering from critical illness are often hesitant to make medication changes until they become comfortable with the patient’s trajectory. The absence of an established checkpoint to re-evaluate the patient’s medication list upon improvement in their clinical status can result in inappropriate continuation of short term medications or discontinuation of chronic medications throughout hospitalization and even after hospital discharge.
For instance, studies in the adult literature report an increased incidence of unintentional discontinuation of chronic pre-admission medications among adults admitted to an ICU (7,12). Specific medications including antiplatelet and anticoagulant medications, inhalers, levothyroxine, gastric acid blocking agents and statins were demonstrated to have a higher risk of discontinuation for patients admitted to the ICU compared to those with only ward admissions (12). On the other hand, 20–30% of adults initiated on short term antipsychotic therapy for ICU delirium have these medications incorrectly prescribed upon discharge from the hospital (13-15). Medications such as bronchodilators and proton pump inhibitors initiated during critical illness are often inappropriately continued after hospital discharge as well (8).
Pharmacist involvement
Development of a structured medication reconciliation process, specifically at ICU discharge, could mitigate some of these preventable medication errors. In two adult ICUs in the Netherlands, medication reconciliation completed shortly before transfer of patients from the ICU to the ward, was associated with a decrease in medication transfer errors from 45% to 15% (16). In this study, the ICU physician and pharmacist created a “best possible ICU medication discharge list”, which contained recommendations regarding timeline for continuation of new medications as well as a list of chronic pre-admission medications that were discontinued in the ICU. This study suggests that clinical pharmacist involvement in transfer medication reconciliation could contribute to decreased medication errors, similar to previous studies evaluating pharmacist participation in medication reconciliation at hospital admission or discharge (17).
Strategies to reduce inappropriately long courses of antipsychotics for ICU delerium include implementation of an algorithm to evaluate patients who are candidates for antipsychotic discontinuation based on delerium scores, as well as creation of a pharmacy-driven electronic handoff tool at ICU discharge. In adults, these interventions were associated with lower rates of antipsychotic prescription at the time of ICU discharge (14,18).
While data regarding medication reconciliation in critically ill children is sparse, children are at higher risk of medication related errors as compared to adults given their need for weight-based dosing and formulation (19). Critically ill children with medical complexity, particularly those taking multiple pre-admission medications, chronic respiratory medications, and chronic non-invasive ventilation have been found to have an increased risk of incorrect medication reconciliation at ICU admission or transfer (20). Future work in pediatrics is needed to quantify medication reconciliation errors around ICU discharge and also to test various improvement initiatives to streamline the reconciliation process during transfer.
Timing of transfer
ICU beds are a necessary and valuable resource for managing patients with life-threatening illnesses, but they are also expensive. ICU strain, defined as demand for ICU beds in excess of supply, can lead to delayed or refused ICU admissions and cancelled elective surgical procedures (21). Strained ICUs are also at risk for providing suboptimal care and experiencing higher rates of adverse events, unplanned ICU readmissions and death (21). This creates pressure to transfer patients out of the ICU in a timely fashion. Multiple studies have examined the impact of adult and to a lesser extent pediatric ICU discharged timing on patient outcomes.
Nighttime transfers
Nighttime ICU discharge is defined as discharge from the ICU at night or “after-hours”, although the time-specific definition often varies by institution and study (22). Nighttime discharge is 1 of 4 most common indicators of ICU strain (21). In adult literature, nighttime discharges have been examined for their impact on adverse patient outcomes including mortality (22-26), unplanned readmission to the ICU (23,24), and hospital LOS (23-25). While data are conflicting, some studies have demonstrated increased hospital mortality for patients following nighttime ICU discharges when adjusted for factors including comorbidities and illness severity (22,24,25). Conversely, weekend ICU discharge has not been associated with increased hospital mortality (22). These studies had similar discrepant results in terms of association between nighttime discharge association and hospital length of stay (LOS) [longer (23) vs. unchanged (24) vs. shorter (25)] and unplanned readmission [higher (23) vs. unchanged (24)]. Discrepancies in the studies’ results are likely due to differences in definitions of nighttime or weekend discharge, local health system, patient population, disease severity, therapy limitations, sample size and study design (22).
The pediatric literature is less robust, and nighttime discharge from the pediatric ICU (PICU) has only been examined in the context of unplanned readmission to the PICU. In 2013, a large retrospective cohort study utilizing the Virtual PICU Systems database (VPS) which included 73 participating North American PICUs, found that discharge time between 4:00 pm and 8:00 am was associated with a higher risk of ICU readmission (27). A similar study also published in 2013, but incorporating more recent data using the same VPS database (now consisting of 90 PICUs), contradicted this association between nighttime discharge and readmission (28). A single site retrospective case control study by Kotsakis et al., found that unplanned readmission was associated with discharge outside their goal discharge time (6:00 am and 11:59 am) on univariable analysis, but this association was no longer significant with multivariable analysis. They still concluded that discharge time of day was one of the few modifiable factors, along with the Pediatric Logistic Organ Dysfunction (PELOD) and Bedside Pediatric Early Warning Signs (BedsidePEWSTM) scores at time of discharge which may decrease ICU readmissions (29).
ICU discharge delays
While nighttime discharge can sometimes represent premature discharge from the ICU, delay in discharge to the ward also can have negative impact. Discharge delays can lead to increased cost, misallocation of resources (30), and place patients at increased risk for ICU-acquired infections which independently influence mortality and additional discharge delays (22). Communication may also fail because provider handoffs typically occur when patients are ready for transfer but infrequently when they actually move between units (30). Discharge delays are more likely to occur at night (22,31) and are associated with high hospital census (31). The most common reason for delayed transfer is lack of ward bed availability (22,31,32). Other reasons include lack of bed/room appropriate for infectious contact precautions, change of primary service (i.e., surgery to medicine) and lack of available patient attendant or sitter (31).
Quality improvement techniques have been leveraged to reduce discharge delay. Kibler et al. improved the transfer process from their ICU to the medical/surgical ward which resulted in decreased average transfer time from 6 hours to <1.4 hours, decreased number of patients experiencing extreme delays (>12 hours), decreased nursing overtime, and improved patient satisfaction scores (33). In this study, implementation of a flag within the EHR when a transfer order was placed, eliminating an external transfer team, utilizing an ICU staff member to communicate need for room cleaning, and ongoing reviews when ICU transfer took >1 hour led to achievement of these metrics (33). In a systematic review of interventions that improve clinical handover between ICU and ward professionals, van Sluisveld et al. found that an ICU liaison nurse (LN), described in the literature as a nurse charged with coordinating care and serving as a liaison between providers in the ICU, providers on the ward, and the patient and family, was shown to reduce discharge delay in 3 out of 4 studies (34).
Readmissions to the PICU
Most patients transferred from the ICU to the ward continue to improve and eventually are discharged to home, however a subset of these patients are readmitted to the ICU. The Society of Critical Care Medicine (SCCM), the National Association of Children’s Hospitals and Related Institutions, and the National Quality Forum advocate that early unplanned readmission to the ICU, defined as readmission less than 48 hours from ICU discharge, should be used as a quality metric (35). The growing body of literature on ICU readmissions describes the rate, timing, and characteristics of patients with unplanned readmissions, utilization of transition programs to bridge the transition to the ward and development of clinical markers to predict readmission.
Patient population
Between 2.5–5.4% of PICU discharges will have an unplanned PICU readmission (27,29,36,37) with approximately 1/3 to 1/2 of PICU readmissions occurring within the first 48 hours (27,36). Patients readmitted to the ICU are at higher risk of mortality and have longer ICU and hospital LOS (Table 1). There is varying data regarding the most common diagnoses to require early unplanned PICU readmission, although respiratory and infectious illnesses are consistently found to be the most frequent primary diagnosis categories (27,36). Interestingly, among CICU patients, respiratory diagnoses were the most common reason for readmission, accounting for 42.9% of readmissions, followed by cardiac diagnoses which accounted for 40.2% of readmissions (38). Studies have demonstrated with varying concordance other factors associated with readmission. Factors which have been associated with unplanned PICU readmissions include young age, presence of at least one chronic health condition (27,36), discharge from the ICU outside of the hours of 8:00 am–4:00 pm (27) and discharge from the ICU on respiratory support or sedating medications (36).

Full table
Prediction tools
Given the increased morbidity and mortality of patients requiring readmission to the ICU, prediction models to help identify patients at highest risk for readmission have been explored. There are few validated scores in the adult literature. These include the Sabadell score which is a subjective measure by the ICU physician to predict overall prognosis following discharge (39) and multivariable algorithms described by Badawi and Breslow (40). The SWIFT score, which utilizes five variables including original source of ICU admission, ICU LOS, PaO2/FiO2, Glascow Coma Scale, and PaCO2 to predict risk of readmission, has demonstrated mixed results predicting ICU readmission in adults (41,42). Attempts to apply the SWIFT score to pediatrics have not been successful (43).
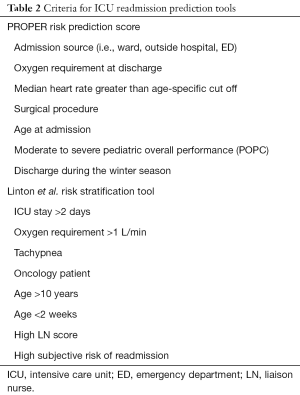
Two prediction tools which have been developed in pediatrics include the PROPER risk predictive score (43) and a validated risk stratification tool developed by Linton et al. (44). The PROPER risk predictive score uses seven objective categories to predict ICU readmission (Table 2) (43). This score predicted early readmissions with a sensitivity of 81% and positive predictive value of 0.5; however it has not been formally validated, and may not be generalizable as it has only been studied in a single center (43). Linton et al. describe an eight factor tool which includes six objective measures and two subjective measures scored by an ICU or LN (Table 2) (44). When the subjective scores were incorporated, patients with 5 or more of these risk factors had a 100% risk of readmission while those with 1 or fewer risk factors had only a 3% chance of readmission, however when the authors removed the subjective components the positive and negative predictive, values decreased (44). These studies highlight the difficulty of accurately predicting which patients will be readmitted, emphasizing the importance of clinical judgement in identifying at risk patients.
Full table
Transition programs
Implementation of transition programs including the utilization of a LN, a critical care outreach team, or medical emergency team (MET) have also been studied as a means to decrease unplanned PICU readmission. These programs utilize staff trained in ICU care to perform routine patient evaluations within the first 48 hours following ICU discharge. In general, studies evaluating transition programs have been small single center studies. While studies evaluating adult transition programs demonstrate mixed results, a meta-analysis demonstrated that transition programs decreased ICU readmission but did not improve the in-hospital mortality rate (45). These findings were primarily driven by a study by Ball et al. which described use of a critical care outreach team that was associated with a decrease in ICU readmission by 6.4% as well as a reduction of in-hospital mortality by 6.8% (46). The data on transition programs for pediatric hospitals is sparse. One single-center study evaluating the benefit of a LN demonstrated a decrease in unplanned PICU readmission from 5.4% to 4.8%, however this did not reach statistical significance (37). Despite not statistically significantly decreasing readmission rate, ward nurses surveyed felt that the role was helpful and over 80% of parents surveyed felt the PICU LN decreased the stress of transition to the ward (37). On the other hand, another single center study evaluating the utility of routine MET assessments in the 48 hours following PICU discharge demonstrated a decrease in unplanned PICU readmissions from 6.8% prior to the initiation of an MET team to 2.0% once the MET team was initiated (47).
Family transition
Hospitalization of a child is a source of anxiety and stress for parents and families. ICU admissions can be even more stressful due to the severity of the child’s medical needs and risk to life. It has been reported that between 10–50% of parents have post-traumatic stress disorder following a child’s admission to the PICU (48-50). Furthermore, families report significant stress during transitions of care (3). The physiological and/or psychosocial distress experienced by patients or families during the transfer from a familiar environment to an unfamiliar one has been labeled ‘transfer anxiety ’or ‘relocation stress’. There are three types of transfer anxiety: (I) primary, relating to time and place of transfer; (II) expectant, relating to preparation quality and (III) fright after transfer, relating to expectations after transfer (51).
Parents’ ability to participate in care and be present for a hospitalized child are important in providing ideal care but can be difficult when families experience stress and lack of information sharing from the care team (3,52). Inclusion of caregivers via clear communication, empathy, education and providing of resources can help prepare parents and caregivers and keep them involved in their child’s care. A systematic review aimed at describing interventions to support parents through an acute hospitalization identified 12 randomized control trials (53). The most common interventions focused on coping and emotional support, including Creating Opportunities of Parent Empowerment (COPE). These supportive interventions were feasible to implement in the majority of the included studies and, most importantly, were valued by parents. Further, parents who received the coping support interventions had lower anxiety and stress symptoms than controls, although depression symptoms were similar between groups (53).
Perceptions of transition
Perceptions of patients and healthcare staff about ICU to ward transfer can also lend important learnings. Stelfox et al. conducted a multicenter prospective cohort study of adult patients transferred from an ICU to the ward with the aim of assessing perceptions about ICU to ward transfer (30). They conducted standardized surveys of patients, nurses, and physicians from both the ICU and ward. Patients were more likely to report satisfaction with transfer when they had their questions answered, met the ward physician prior to transfer, and were assessed by a nurse within 1 hour of ward arrival (30). All groups recommended that transfer delays be minimized and to avoid night transfers. In this study, 1 in 4 patients awaiting transfer had a major care plan change, further highlighting the importance of updated and repeated communication for delayed transfers (30).
Written information
In addition to supporting coping and emotional well-being of families, many studies have focused on development and standardization of information to help prepare families for transition. Two common strategies are written information and LNs. The use of a written letter with accompanying verbal explanation was evaluated in a group of fifty biological parents of children admitted to the ICU for the first time for an acute illness. Half of the families received the letter and verbal explanation in the 24–48 hours before transfer while the other half received standard care that did not include either of these. Measurement of parental anxiety and stress using a validated scoring system before the information was shared and at time of transfer demonstrated decreased anxiety at time of transfer for the intervention group (54).
A similar program developed a PICU discharge brochure created with family input. The most important information for families in this program included the name and location of the ward they were going to and being informed of the plan for transfer ahead of time. The families also reported wanting information about the ward team members’ names. Feedback obtained via surveys suggested that most families found the use of this brochure to be helpful or very helpful (55). Another hospital trialed a brochure and a standard transfer checklist to be used by the bedside nurse. The use of these tools resulted in increased parental report of feeling prepared for transfer in a timely manner (56).
Transition care providers
Care providers dedicated to patient transition between the ICU and ward have been leveraged to improve the patient and family experience. LNs may be used to support families during the physical time of transition. This role begins with the preparation component and extends to face-to-face check-ins with the patient and family after transfer. The liaison serves to extend the knowledge of the PICU and ensure ward nurses are prepared and well-informed about the patient’s needs. They also ensure patient care plans have been communicated between the PICU and ward teams. Lastly, due to their familiarity to the patient and family, they can assist the family in answering any questions that arise in the transition (37,57). Outcomes have been promising, with one study showing lower PICU readmission after initiating the LN transition role, and >98% of staff and families reporting that the LN made a positive impact on the transition process (37). Other studies have taken a more proactive approach. At Wake Forest Baptist Hospital, providers have trialed the implementation of a dedicated transfer team, including a hospitalist physician, nurse leader and bed logistic personnel, who travel to the ICU each morning to introduce the ward team to the family, obtain a verbal handoff from the ICU and assess stability for transfer for any patient who is predicted to transfer to the wards in the next 24 hours (58).
Children with new technology
Children with chronic respiratory failure and new technology dependence present additional challenges to the medical team when transferring from the ICU to the ward. Children with chronic respiratory failure often have complex needs with multisystem involvement (59). These children with medical complexity (CMC) may require enteral feeding tubes, tracheostomy tubes, home ventilators, suction machines or other equipment in the home. The number of children with chronic respiratory failure and dependence on home ventilation has increased, as has the frequency of hospitalization for CMC (60,61). The cost of care for a ventilator-dependent child in an ICU is significantly higher than the cost of care on the ward (62). While some children with chronic respiratory failure may be discharged directly from the ICU, more CMC are being transitioned home from less-costly ventilator wards. When an older child with new technology dependence is transferring from the PICU, caregivers may already have some familiarity with caring for a child with complex medical needs. When an infant is transferring from the neonatal ICU (NICU), families will also be adjusting to the stress of bringing a child home for the first time regardless of the need for medical equipment in the home. The additional needs of the child with new technology dependence require multidisciplinary involvement in planning for a safe and efficient transition to home.
In addition to the child’s medical status, several other factors will determine the readiness of a child with new technology dependence to transition to home, including: (I) caregiver education; (II) durable medical equipment availability; (III) home nursing availability; (IV) home readiness; and (V) financial resources (63). One or more medical or social factors can significantly delay a child’s transition to home (64). Initiation of early discharge coordination to address these factors in the ICU, prior to transfer to the wards, can reduce the overall hospital LOS without increasing readmission rates (65). With an eye on eventual transition to home, the transition of the child to the ward may require the involvement of a discharge planner, SW, family educator and case worker in addition to the other members of the medical team. Ideally, these team members will meet the family in the ICU as soon as it is determined that the child will require medical equipment in the home to discuss education requirements and the process of transitioning to home.
Education
Children with tracheostomies should have at least two caregivers fully educated on the child’s routine and emergency care (66). Education should be initiated in the ICU whenever possible. Caregivers of children going home with medical equipment should have every opportunity to participate the care of the child to gain experience with the new equipment and to troubleshoot equipment that is not working as expected. Education incorporating videos or simulation can also be considered, if the family is open and ready to learn. If education is initiated in the ICU, progress should be documented in a standardized fashion so that the education plan can be continued by the team on the wards. Additionally, helping families understand the extent of education required to care for their child at home prior to transitioning to the ward will help to set expectations and avoid conflicts on the wards.
Durable medical equipment
Early contact with a durable medical equipment company to order and arrange for the delivery of home medical equipment is important to avoid delays in discharge to home. Longitudinal involvement by the accepting medical team and discharge coordinator while the child is in the ICU may help to identify equipment needs at the time of discharge. If the process of arranging for home equipment is initiated in the ICU, it is important for this information to be shared with the medical team and discharge coordinator on the wards. A list of home equipment should be standardized and available to all staff.
Home nursing
In many parts of the country, there is a critical lack of home nursing available to families with children dependent on technology (67). While not all children going home with new medical equipment will require home nursing, some populations are especially dependent on home nursing to allow for a safe transition to home. Children dependent on a tracheostomy tube and home ventilator should be attended to by an awake and trained caregiver 24 hours a day, which almost always necessitates the presence of a nurse in the home (68). Beginning the search for home nursing while the child is in the ICU can reduce the overall hospital LOS. Delaying the search for home nursing can result in extending hospitalization by weeks to months.
Home environment
Involvement of a SW at the time of transition from the ICU to the ward is important when considering eventual transition to a safe environment out of the hospital. The family’s barriers to a safe discharge home should be identified early. Families with children with new dependence on technology need to consider the appropriateness of their home and means of transportation. An older child who is immobile and newly dependent on a tracheostomy tube and ventilator may be more difficult to care for if the family lives on the third floor of a building without an elevator. This is not only an additional burden on the family, but is also especially important to consider as that child may need to be quickly attended to by emergency medical services personnel in the home. SWs can be instrumental in helping a family identify and mitigate such barriers. Durable medical equipment companies may also assess the home and evaluate the space needed for equipment, electrical capacity and other safety concerns. If a safe home environment cannot be secured, alternative means for discharge, including long-term care, should be considered.
Financial resources
Providers, often SW team members, should help the family to identify financial resources to cover medical needs including home equipment and home nursing. Insurance coverage should be verified early in the process. If a Medicaid waiver program is available, applications should be submitted at an appropriate time to ensure timely coverage for needed resources. Any conversations with private insurance, managed care programs or case managers occurring while the child is in the ICU should be documented and communicated to the medical team and SW at the time of transition to the wards.
Discussion and future directions
Care team recognition that the transition from ICU to the ward can be one of the most stressful periods during a hospitalization is key to providing care to this vulnerable population of patients. For patients and families, this is a time of increased uncertainty. While improved health is likely the trigger for transfer out of the ICU, families have likely become accustomed to the ICU culture, including the higher level of care, more frequent monitoring and different policies/rules (54). The anxiety around this adjustment can be significant and can impact families’ ability to participate in care on the wards. For patients with new technology dependence, families are faced with the added challenges of learning new care needs and equipment as well as the additional psychosocial stresses including securing home nursing, adapting the home environment and financial strain that comes with new technology dependence (27). Promising studies utilizing LNs to bridge transition periods have demonstrated decreased family stress and anxiety (44). Preliminary research exploring the use of hospitalist physicians and nurse leaders to improve the ICU-to-floor transition is being evaluated to understand the impact on ICU LOS, family satisfaction and ICU readmission (58). Further work should continue to explore strategies to improve family experience during transitions of care.
Timing of ICU discharge is an important consideration in ensuring a smooth transition to the wards. Based on the literature, there may be an increased risk of mortality and unplanned ICU readmission for nighttime discharges, as well as negative impact from transfer delays. Both nighttime transfer and delayed discharge-to-ward often reflect limited bed capacity (22) and ICU strain (21). Therefore, the decision to transfer a patient out of the ICU is a challenging balance of benefits and risks, particularly for patients with complex chronic conditions.
Risk stratification of patients and the development of future predictive scoring systems may prevent negative outcomes (i.e., unplanned readmissions) from a premature or delayed discharge from the ICU. Preliminary studies of prediction tools have involved objective criteria combined with LN assessments (54). Ongoing development of ICU readmission prediction tools is needed as readmission increases hospital and ICU LOS and is associated with increased mortality (36,43-45,47,48). Accurate prediction tools would allow providers to better prepare families for transfer and provide more focused support to the ward team and nurses surrounding the care of patients with higher risk of ICU readmission.
Current studies also demonstrate that patient handoffs from the ICU-to-ward are not always complete (2,3). Handoff tools that include a comprehensive problem list with treatment plans (2) and emphasize needs to happen in the next 24–48 hours rather than just the summary of the clinical course (58) should be evaluated as a strategy to improve clarity on treatment plans. In the adult literature, lack of clarity regarding medication plans has been shown to lead to inadvertent discontinuation of home medications (8,9) as well as inappropriate continuation of medications initiated in the ICU (10-14). The pediatrics literature is sparse necessitating further investigation of current practices for medication reconciliation in critically ill children and their association with medication errors and patient harm. This could inform the development and evaluation of interventions to reduce medication error at the time of ICU discharge in children, particularly for children with medical complexity. Structured, pharmacist-driven handoff tools that contain plans for medication re-initiation or discontinuation after resolution of critical illness could serve to reduce medication errors at hospital discharge. Incorporating an ICU discharge medication plan into the verbal handoff to physicians and nurses on the general ward could empower the ward team to proactively reduce medication related errors in this population.
Conclusions
Patient handoffs, medication reconciliation, timing of transfer, risk of readmission, preparing the family, and education on new medical needs are all factors that should be considered when transitioning patients from the ICU to the ward. The challenges of ICU strain may impact optimal transfer timing. However, ongoing exploration of the use of LNs, standardized handoff tools and development of readmission risk assessment tools are promising strategies to improve the ICU to ward transfer process and should be continued. Future studies should focus on initiation of education on new technologies while in the ICU, exploration of pharmacist-led medication reconciliation processes, and innovative ways to improve the family experience during ICU to ward transfer.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Joint Commission on Accreditation of Healthcare Organizations. USA. Using medication reconciliation to prevent errors. Sentinel Event Alert 2006.1-4. [PubMed]
- Leyenaar JK, Desai AD, Burkhart Q, et al. Quality Measures to Assess Care Transitions for Hospitalized Children. Pediatrics 2016;138. [Crossref] [PubMed]
- Solan LG, Beck AF, Brunswick SA, et al. The Family Perspective on Hospital to Home Transitions: A Qualitative Study. Pediatrics 2015;136:e1539-49. [Crossref] [PubMed]
- Leith BA. Transfer anxiety in critical care patients and their family members. Crit Care Nurse 1998;18:24-32. [PubMed]
- Warrick D, Gonzalez-del-Rey J, Hall D, et al. Improving resident handoffs for children transitioning from the intensive care unit. Hosp Pediatr 2015;5:127-33. [Crossref] [PubMed]
- Brown KN, Leigh JP, Kamran H, et al. Transfers from intensive care unit to hospital ward: a multicentre textual analysis of physician progress notes. Crit Care 2018;22:19. [Crossref] [PubMed]
- Ghosheh F, Hamid F, Ruwaida WA, et al. Unintentional discontinuation of long-term medications: Comparison of intensive-care-unit and other settings. Am J Health Syst Pharm 2010;67:1141. [Crossref] [PubMed]
- Pavlov A, Muravyev R, Amoateng-Adjepong Y, et al. Inappropriate discharge on bronchodilators and acid-blocking medications after ICU admission: importance of medication reconciliation. Respir Care 2014;59:1524-9. [Crossref] [PubMed]
- Institute of Medicine CoQHCi, America. Crossing the Quality Chasm—A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001.
- Starmer AJ, Spector ND, Srivastava R, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med 2014;371:1803-12. [Crossref] [PubMed]
- Sheth S, McCarthy E, Kipps AK, et al. Changes in Efficiency and Safety Culture After Integration of an I-PASS-Supported Handoff Process. Pediatrics 2016;137. [Crossref] [PubMed]
- Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA 2011;306:840-7. [Crossref] [PubMed]
- Marshall J, Herzig SJ, Howell MD, et al. Antipsychotic utilization in the intensive care unit and in transitions of care. J Crit Care 2016;33:119-24. [Crossref] [PubMed]
- D'Angelo RG, Rincavage M, Tata AL, et al. Impact of an Antipsychotic Discontinuation Bundle During Transitions of Care in Critically Ill Patients. J Intensive Care Med 2016. [Epub ahead of print]. [PubMed]
- Flurie RW, Gonzales JP, Tata AL, et al. Hospital delirium treatment: Continuation of antipsychotic therapy from the intensive care unit to discharge. Am J Health Syst Pharm 2015;72:S133-9. [Crossref] [PubMed]
- Bosma LBE, Hunfeld NGM, Quax RAM, et al. The effect of a medication reconciliation program in two intensive care units in the Netherlands: a prospective intervention study with a before and after design. Ann Intensive Care 2018;8:19. [Crossref] [PubMed]
- Mekonnen AB, McLachlan AJ, Brien JA. Pharmacy-led medication reconciliation programmes at hospital transitions: a systematic review and meta-analysis. J Clin Pharm Ther 2016;41:128-44. [Crossref] [PubMed]
- Kram BL, Schultheis JM, Kram SJ, et al. A Pharmacy-Based Electronic Handoff Tool to Reduce Discharge Prescribing of Atypical Antipsychotics Initiated in the Intensive Care Unit: A Quality Improvement Initiative. J Pharm Pract 2018. [Epub ahead of print]. [PubMed]
- Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA 2001;285:2114-20. [Crossref] [PubMed]
- DeCourcey DD, Silverman M, Chang E, et al. Medication Reconciliation Failures in Children and Young Adults With Chronic Disease During Intensive and Intermediate Care. Pediatr Crit Care Med 2017;18:370-7. [Crossref] [PubMed]
- Rewa OG, Stelfox HT, Ingolfsson A, et al. Indicators of intensive care unit capacity strain: a systematic review. Crit Care 2018;22:86. [Crossref] [PubMed]
- Yang S, Wang Z, Liu Z, et al. Association between time of discharge from ICU and hospital mortality: a systematic review and meta-analysis. Crit Care 2016;20:390. [Crossref] [PubMed]
- Hanane T, Keegan MT, Seferian EG, et al. The association between nighttime transfer from the intensive care unit and patient outcome. Crit Care Med 2008;36:2232-7. [Crossref] [PubMed]
- Azevedo LC, de Souza IA, Zygun DA, et al. Association Between Nighttime Discharge from the Intensive Care Unit and Hospital Mortality: A Multi-Center Retrospective Cohort Study. BMC Health Serv Res 2015;15:378. [Crossref] [PubMed]
- Priestap FA, Martin CM. Impact of intensive care unit discharge time on patient outcome. Crit Care Med 2006;34:2946-51. [Crossref] [PubMed]
- Santamaria JD, Duke GJ, Pilcher DV, et al. The timing of discharge from the intensive care unit and subsequent mortality. A prospective, multicenter study. Am J Respir Crit Care Med 2015;191:1033-9. [Crossref] [PubMed]
- Czaja AS, Hosokawa PW, Henderson WG. Unscheduled readmissions to the PICU: epidemiology, risk factors, and variation among centers. Pediatr Crit Care Med 2013;14:571-9. [Crossref] [PubMed]
- Edwards JD, Lucas AR, Stone PW, et al. Frequency, risk factors, and outcomes of early unplanned readmissions to PICUs. Crit Care Med 2013;41:2773-83. [Crossref] [PubMed]
- Kotsakis A, Stevens D, Frndova H, et al. Description of PICU Unplanned Readmission. Pediatr Crit Care Med 2016;17:558-62. [Crossref] [PubMed]
- Stelfox HT, Leigh JP, Dodek PM, et al. A multi-center prospective cohort study of patient transfers from the intensive care unit to the hospital ward. Intensive Care Med 2017;43:1485-94. [Crossref] [PubMed]
- Johnson DW, Schmidt UH, Bittner EA, et al. Delay of transfer from the intensive care unit: a prospective observational study of incidence, causes, and financial impact. Crit Care 2013;17:R128. [Crossref] [PubMed]
- Williams TA, Leslie GD, Brearley L, et al. Discharge delay, room for improvement? Aust Crit Care 2010;23:141-9. [Crossref] [PubMed]
- Kibler J, Lee M. Improving Patient Transfer between the Intensive Care Unit and the Medical/Surgical Floor of a 200-Bed Hospital in Southern California. J Healthc Qual 2011;33:68-76. [Crossref] [PubMed]
- van Sluisveld N, Hesselink G, van der Hoeven JG, et al. Improving clinical handover between intensive care unit and general ward professionals at intensive care unit discharge. Intensive Care Med 2015;41:589-604. [Crossref] [PubMed]
- Scanlon MC, Mistry KP, Jeffries HE. Determining pediatric intensive care unit quality indicators for measuring pediatric intensive care unit safety. Pediatr Crit Care Med 2007;8:S3-10. [Crossref] [PubMed]
- Bernard AM, Czaja AS. Unplanned pediatric intensive care unit readmissions: a single-center experience. J Crit Care 2013;28:625-33. [Crossref] [PubMed]
- Caffin CL, Linton S, Pellegrini J. Introduction of a liaison nurse role in a tertiary paediatric ICU. Intensive Crit Care Nurs 2007;23:226-33. [Crossref] [PubMed]
- Bastero-Miñón P, Russell JL, Humpl T. Frequency, characteristics, and outcomes of pediatric patients readmitted to the cardiac critical care unit. Intensive Care Med 2012;38:1352-7. [Crossref] [PubMed]
- Fernandez R, Serrano JM, Umaran I, et al. Ward mortality after ICU discharge: a multicenter validation of the Sabadell score. Intensive Care Med 2010;36:1196-201. [Crossref] [PubMed]
- Badawi O, Breslow MJ. Readmissions and death after ICU discharge: development and validation of two predictive models. PLoS One 2012;7. [Crossref] [PubMed]
- Gajic O, Malinchoc M, Comfere TB, et al. The Stability and Workload Index for Transfer score predicts unplanned intensive care unit patient readmission: initial development and validation. Crit Care Med 2008;36:676-82. [Crossref] [PubMed]
- Oakes DF, Borges IN, Forgiarini LA Junior, et al. Assessment of ICU readmission risk with the Stability and Workload Index for Transfer score. J Bras Pneumol 2014;40:73-6. [Crossref] [PubMed]
- Kaur H, Naessens JM, Hanson AC, et al. PROPER: Development of an Early Pediatric Intensive Care Unit Readmission Risk Prediction Tool. J Intensive Care Med 2018;33:29-36. [Crossref] [PubMed]
- Linton S, Grant C, Pellegrini J, et al. The development of a clinical markers score to predict readmission to paediatric intensive care. Intensive Crit Care Nurs 2009;25:283-93. [Crossref] [PubMed]
- Niven DJ, Bastos JF, Stelfox HT. Critical care transition programs and the risk of readmission or death after discharge from an ICU: a systematic review and meta-analysis. Crit Care Med 2014;42:179-87. [Crossref] [PubMed]
- Ball C, Kirkby M, Williams S. Effect of the critical care outreach team on patient survival to discharge from hospital and readmission to critical care: non-randomised population based study. BMJ 2003;327:1014. [Crossref] [PubMed]
- Lobos AT, Fernandes R, Willams K, et al. Routine Medical Emergency Team Assessments of Patients Discharged From the PICU: Description of a Medical Emergency Team Follow-Up Program. Pediatr Crit Care Med 2015;16:359-65. [Crossref] [PubMed]
- Nelson LP, Gold JI. Posttraumatic stress disorder in children and their parents following admission to the pediatric intensive care unit: a review. Pediatr Crit Care Med 2012;13:338-47. [Crossref] [PubMed]
- Stowman S, Kearney CA, Daphtary K. Mediators of Initial Acute and Later Posttraumatic Stress in Youth in a PICU. Pediatr Crit Care Med 2015;16:e113-8. [Crossref] [PubMed]
- Bronner MB, Knoester H, Bos AP, et al. Follow-up after paediatric intensive care treatment: parental posttraumatic stress. Acta Paediatr 2008;97:181-6. [Crossref] [PubMed]
- Coyle MA. Transfer anxiety: preparing to leave intensive care. Intensive Crit Care Nurs 2001;17:138-43. [Crossref] [PubMed]
- Solan LG, Beck AF, Shardo SA, et al. Caregiver Perspectives on Communication During Hospitalization at an Academic Pediatric Institution: A Qualitative Study. J Hosp Med 2018;13:304-11. [PubMed]
- Doupnik SK, Hill D, Palakshappa D, et al. Parent Coping Support Interventions During Acute Pediatric Hospitalizations: A Meta-Analysis. Pediatrics 2017;140. [Crossref] [PubMed]
- Bouvé LR, Rozmus CL, Giordano P. Preparing parents for their child's transfer from the PICU to the pediatric floor. Appl Nurs Res 1999;12:114-20. [Crossref] [PubMed]
- Linton S, Grant C, Pellegrini J. Supporting families through discharge from PICU to the ward: the development and evaluation of a discharge information brochure for families. Intensive Crit Care Nurs 2008;24:329-37. [Crossref] [PubMed]
- Van Waning NR, Kleiber C, Freyenberger B. Development and implementation of a protocol for transfers out of the pediatric intensive care unit. Crit Care Nurse 2005;25:50-5. [PubMed]
- Manente L, McCluskey T, Shaw R. Transitioning Patients from the Intensive Care Unit to the General Pediatric Unit: A Piece of the Puzzle in Family-Centered Care. Pediatr Nurs 2017;43:77-82. [PubMed]
- Cristiano J, Beekman D, Summers E. An Innovative Approach to the ICU to Ward Transition of Care. J Hosp Med 2015;10:abstr 311. Available online: , accessed August 29, 2018.https://www.shmabstracts.com/abstract/an-innovative-approach-to-the-icu-to-ward-transition-of-care/
- Edwards JD, Houtrow AJ, Lucas AR, et al. Children and Young Adults Who Received Tracheostomies or Were Initiated on Long-Term Ventilation in PICUs. Pediatr Crit Care Med 2016;17:e324-34. [Crossref] [PubMed]
- Cristea AI, Carroll AE, Davis SD, et al. Outcomes of children with severe bronchopulmonary dysplasia who were ventilator dependent at home. Pediatrics 2013;132:e727-34. [Crossref] [PubMed]
- Benneyworth BD, Gebremariam A, Clark SJ, et al. Inpatient health care utilization for children dependent on long-term mechanical ventilation. Pediatrics 2011;127:e1533-41. [Crossref] [PubMed]
- Edwards JD, Rivanis C, Kun SS, et al. Costs of hospitalized ventilator-dependent children: differences between a ventilator ward and intensive care unit. Pediatr Pulmonol 2011;46:356-61. [Crossref] [PubMed]
- Barnhart SL, Carpenter A. Caring for the Ventilator Dependent Child: A Clinical Guide. New York: Humana Press, 2016:89-119.
- Graf JM, Montagnino BA, Hueckel R, et al. Children with new tracheostomies: planning for family education and common impediments to discharge. Pediatr Pulmonol 2008;43:788-94. [Crossref] [PubMed]
- Baker CD, Martin S, Thrasher J, et al. A Standardized Discharge Process Decreases Length of Stay for Ventilator-Dependent Children. Pediatrics 2016;137. [Crossref] [PubMed]
- Sherman JM, Davis S, Albamonte-Petrick S, et al. Care of the child with a chronic tracheostomy. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 2000;161:297-308. [PubMed]
- Hefner JL, Tsai WC. Ventilator-dependent children and the health services system. Unmet needs and coordination of care. Ann Am Thorac Soc 2013;10:482-9. [Crossref] [PubMed]
- Sterni LM, Collaco JM, Baker CD, et al. An Official American Thoracic Society Clinical Practice Guideline: Pediatric Chronic Home Invasive Ventilation. Am J Respir Crit Care Med 2016;193:e16-35. [Crossref] [PubMed]


