
Quality improvement in healthcare for patients with inflammatory bowel disease
Introduction
Crohn’s disease (CD) and ulcerative colitis (UC) are the principal sub-types of inflammatory bowel disease (IBD), which is believed to be caused by a complex interaction of environmental, genetic, and immune-regulatory factors. The diagnosis is mainly established through combination of clinical, laboratory, endoscopic, and radiological observations (1).
In a recent systematic review that was published in 2017, the worldwide prevalence of IBD has surpassed 0.3%, with the highest figure of UC as 505 per 100,000 in Norway and CD affecting 322 per 100,000 in Germany. The prevalence of UC was 286 per 100,000 in the USA with CD affecting 319 per 100,000 in Canada (2). The incidence and prevalence of pediatric IBD are also on the rise (3).
In 2018, Crohn’s and Colitis Canada published “a burden-of-illness report” which highlighted the significant direct and indirect financial burden of IBD on the Canadian public healthcare system with the presence of a considerable gap between perceived ideal and actual care in IBD (4).
What is quality improvement (QI) in healthcare?
Quality of healthcare is “the level to which health services for persons and populations increase the likelihood of desired health outcomes and are in agreement with current professional knowledge” (5). The definition, adopted by the World Health Organization (WHO) (6) in 2018, implies more than mere service inputs and system processes. It should reflect the needs and satisfactions of key stakeholders, including communities and service users.
The institute for healthcare improvement in USA (IHI) (7) has developed the “Triple Aim” as a framework to describe a perspective of enhancing health system performance. It is IHI’s belief that new designs must be honed to coincidently pursue three directions: advancing patients’ experience of medical care including both quality and satisfaction, improving the health of populations, and reducing the per capita cost of care.
The span involves both preventive and curative medical care. As it is vital that new evidence is systematically implemented into the provided care, high quality research will remain in the heart of the equation.
Although the history of QI in healthcare dates back to the era of Florence Nightingale in the 1850s (7), a real turning point of its current wave belongs to the landmark paper by McGlynn et al. (8), which found that only 54% of patients in the United States were given the recommended medical care (9). Such findings with simultaneous reports from the Institute of Medicine, documenting quality and safety issues, provided an incentive and the necessary push toward improving the quality of healthcare in the United States. Each component of medical care needs to be audited in relation to the several aspects that include safety, efficacy, accessibility, effectiveness, and equity (6). Besides, the structure serves as a tool to measure changes within the systems and services. For an improvement in quality to be achieved, an objective comparison needs to be performed for the same seven components.
A QI program is essential to all healthcare organizations and systems. It brings about a wide range of advantages, including more favorable outcomes, better efficiencies, cost-effectiveness, enhanced reliability and predictability with preemptive solutions for problems and higher trust by partners with an overall more successful achievement of the organizational goals (10-12).
QI in IBD
In 2000, Balas and Boren found out that there is an average of 17-year gap to incorporate knowledge from randomized controlled trials into routine clinical practice, and even then, the application of knowledge was highly variable (13). Later in 2005, another study specific to IBD showed that 11% of patients have received care which is not recommended in guidelines and may even be potentially harmful (14).
Variations in practice are the surrogate markers for poor quality of care including overuse, underuse or even misuse of healthcare resources (15). Two recent studies in patients with CD and UC have proven significant variations between experts and community practitioners, in addition to variations within the groups in management of each condition (16,17). In patients with CD, the variation was mainly related to treatment in spite of diagnosis consensus. On the other hand, in patients with UC the variation was more pronounced in aspects related to cancer surveillance, dosing of medications, drug monitoring and management of more severe cases. Interestingly, even in tertiary centers, the quality of care seemed to be far from optimum as well. This was reflected in an earlier study that reported suboptimal dosing of mesalazine and immunomodulators, delayed referrals for colorectal screening in eligible patients, deficient attention to metabolic bone loss associations, and complications in addition to unnecessary prolonged use of corticosteroids (18). Besides, there is solid evidence that the pediatric management of IBD is not an exception from variation in care. Two multicentre studies reported a significant variation in treatment prescriptions and clinical outcomes among children newly diagnosed with IBD (19,20).
Comparison of outcomes could be a reliable measure for quality of care and the changes implemented to improve it. Two studies published in 2008 showed that post colectomy mortality rates in high-volume USA hospitals were less than half of those in low-volume hospitals (21,22). Such findings provided a significant proof that variation in care is common, with resultant major variation in clinical outcomes.
Interventions to build QI in IBD
Population health management strategies are those for implementation of the triple aim; moving from volume to value by advancing the quality of care provided, improving population health outcomes, and minimizing healthcare costs (23,24). Adapted from the “National Quality Strategy for Improvement in Healthcare” (25), the triple aim can be divided into the following workable components:
- creating a safer care by reducing possible harms generated during the delivery of healthcare;
- ensuring that providers, patients, families, and communities are committed as partners;
- promoting effective communication, collaboration and coordination of all healthcare components;
- encouraging the most cost-effective, risk-stratified prevention and therapy practices.
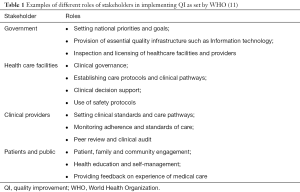
The first step of implementation comprises identification of a high-risk population, leading causes of high costs and discrepancy in care within specific populations (26). When planned at a national or multi-national level, the QI needs to be implemented in harmony among various stakeholders. Table 1 demonstrates examples the roles of all contributing players as set by the WHO vision issued in 2018 for an imperative of universal health coverage to deliver high quality services (11). Governments are encouraged to define the priorities and goals, provide infrastructures for healthcare, facilitate regulations, audit practices, and inspect providers. Healthcare facilities have responsibilities of clinical governance, establishing evidence-based protocols, supporting evidence-guided clinical decisions, setting safety standards and promoting inter-institutional learning. Providers have a duty to abide by clinical guidelines and involve experts in decision making. Patients and public have to be engaged, self-educate, and participate in governance and feeding back their experience.
Full table
The described roles emerged from the five inter-related strategies for the enhancement of people-centered services declared by WHO in December 2017 (6), coordinating services, strengthening accountability, reorienting the model of care, engaging and empowering people, which will all create an enabling environment for positive changes (27).
Quality indicators are “objective measures to evaluate the condition of healthcare by discovering whether evidenced-based, expert-recommended, and patient-centered standards are being applied”. They should be specific and measurable elements of care which help to distinguish between high- and low-quality. The indicators are dynamically reviewed for the structure, process, and outcomes of care (28). Structure measures examine the overall accessibility of healthcare resources like enough staffing, well-recognized access to specialists, and medication availability. Measures of process evaluate the steps of proper care expected to result in a favourable outcome. Outcome measures include mortality, complications, and resolution of symptoms and signs of disease. Other measures should be utilized to make sure that advancement in one area will not negatively affect performance in another area (29). A perfect example would be that spending on equipment should not adversely affect spending on staffing. Inclination for referrals to experts seeking higher standard management should not delay the diagnosis. Reduction of length of hospitalization days has to consider avoidance of premature discharge before completion of treatment.
On more specific relevance to IBD, several sets of quality measures have been developed. “The American Gastroenterological Association” (AGA) developed process measures for IBD in the United States. This system has been used by the “federal health insurance program (Medicare)” to provide financial motivation for gastroenterologists looking after persons with IBD (30). Nonetheless, these measures are primarily used for answerability and reporting for financial incentives, rather than for QI purposes (29).
In 2013, CCFA published ten process measures and 10 outcome measures (31). These measures have been published to help with standardization of the quality of care in patients with IBD.
“The International Consortium for Health Outcomes Measurement (ICHOM) is an organization that defines and reports standardized outcome measure sets across all diseases”. The ICHOM outcome set for IBD was completed in 2016 and focused on the entire care cycle from diagnosis to remission (32).
“The Promoting Access and Care through Centres of Excellence (PACE)” program is a Canadian initiative to improve the quality of life of patients with IBD through integration of excellence in patient care and research. To reduce variations in clinical care provided to patients with IBD across Canada, the PACE program developed a portfolio of stand-alone structure, process, and outcome of QIs for the diagnosis and management of IBD through a modified RAND appropriateness method which included physicians, nurses, and patients (33). The panel selected 45 QIs. Six were patient-driven, nine addressed service-related aspects and specialist care provided at an IBD clinic. Thirty process indicators included administrative and workflow processes, aspects related to IBD therapy, vaccination, surveillance, and risk management. Six QIs included outcome measures such as steroid use and patients’ satisfaction (33).
Examples of the process and outcome quality indicators in IBD include screening for tuberculosis and hepatitis B before starting biologics, excluding clostridium difficile in persons with IBD and acute diarrhea and ensuring that persons with IBD are well educated about necessary vaccinations (31,33).
Collaborative initiatives are linked practices or systems of care specifically organized to advance standards, quality and end results of care using structured methods. They help sharing of data and best practices between care providers (including physicians) and patients. Thus, such initiatives greatly reduce the variation of management between clinicians and organisations with subsequent levering of global improved outcomes; the most crucial key factor in QI.
In pediatric IBD care, “ImproveCareNow (ICN)” network is a pediatric collaborative of over 95 sites, involving 27,000 patients from USA, UK and Qatar (34). This system allows healthcare providers and patients to share clinical information, patient-reported outcomes, and evidence-based practices to improve clinical care provided to children with IBD. Monthly reports are generated and are sent back to individual sites. These reports engage sites to discuss and implement learning sessions to see where their site is lacking and how to implement changes to enhance the care provided. The sharing of knowledge between sites involved in the ICN allows a wealth of knowledge to help one site see how another site is overcoming certain aspects of care (34). This may act as a guide and provide a framework to enhance the overall quality of care across all sites in the ICN network. Utilizing physician’s global assessment (PGA), ICN investigators have documented a rise in remission rates from 55% to 75% over the past few years; modelling an impressive success story of QI within the field of IBD (35). In another pediatric study from Manitoba, Canada, implementing QI measures resulted in significant reductions in steroid use, IBD-related surgery and hospitalizations and IBD-related emergency room visits (36).
Currently, QI measures and outcomes in pediatric IBD are extrapolated from adult measures and outcomes. This may not be ideal as children are not small adults. For example, one of the current popular quality measures, based on adult studies, is to test for cytomegalovirus (CMV) colitis via sigmoidoscopy in corticosteroid-resistantcolitis (31). An emerging evidence, however, in children with colitis is refuting this recommendation (37).
Linking education to collaborative initiatives can be even more fruitful. In adult IBD management, IBD Qorus is developed by the Crohn’s and Colitis Foundation (38). IBD Qorus is designed to enable rapid data sharing between physicians and persons with IBD. In a study involving many gastroenterologists where a QI education program was implemented for UC, patients’ medical records were audited for 30 gastroenterologists before and after they had participated in the QI education program (39). The audit focused on nine measures; ensuring patient engagement, improving communication, promoting effective treatment practices, guideline-directed vaccinations, careful assessments of disease sub-type and activity, effective education on various topics in UC management, accurate documentation of adverse events, examination of adherence status, and simplification of medication dosing. After the audit was finalized, feedback sessions were conducted for each gastroenterologist. In these sessions, suboptimal care quality was highlighted and action plans were developed for improvement. The same audit was re-performed for the same 30 gastroenterologists after receiving the educational program and improvements ranged from 0–48% (39). This indicated the potential for QI education in advancing performance on key measures of care quality.
It is important to highlight that QI processes may face several challenges including various barriers against collaborative work. Developing evidence-based quality indicators including finding high-quality evidence could be difficult but a much more challenging task is implementing those indicators in routine clinical practice (40). In addition, shortage of funding in most healthcare systems could be an initial hurdle. Nonetheless, effective QI programs would eventually result in significant savings. It is sometimes difficult to directly link a specific intervention to a particular outcome.
Conclusions
Considering the prevalence, the burden and the significant variation of both practice and outcomes for IBD patients, there will be a continuous need for systems of QI. The triple aims of improving patient’s experience, health of populations, and reducing the per capita cost of care can be targeted as standardized objectives for optimization.
Over the past decade, non-profit IBD organizations have exerted tremendous efforts to lever the quality of healthcare by setting standards and quality indicators, education, collaboration, audition, and clinical governance. Nonetheless, there is a room for more work and development of quality measures and indicators; for example, testing for liver function tests at initial diagnosis of IBD and further work up for those with abnormal tests.
Future continuum of build up for QI necessitates planning and implementation at national and multi-national levels, guided by the population health management strategies, concerting the roles of various stakeholders as set earlier in 2018 by the WHO vision to deliver quality patient-centered services.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hanauer SB. Inflammatory bowel disease: epidemiology, pathogenesis, and therapeutic opportunities. Inflamm Bowel Dis 2006;12 Suppl 1:S3-9. [Crossref] [PubMed]
- Ng SC, Shi HY, Hamidi N, et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 2018;390:2769-78. [Crossref] [PubMed]
- El-Matary W, Moroz SP, Bernstein CN. Inflammatory bowel disease in children of Manitoba: 30 years' experience of a tertiary center. J Pediatr Gastroenterol Nutr 2014;59:763-6. [Crossref] [PubMed]
- Impact Report 2018, Crohn's and Colitis Canada. 2018.
- Budd A, Lukas S, Hogan U, et al. A case study and the lessons learned from in-house alcohol-based hand sanitizer production in a district hospital in Rwanda. J Ser Sci Manag 2016;9:150-9. [Crossref]
- Delivering quality health services. A global imperative for universal health coverage. World Health Organization, OECD, and International Bank for Reconstruction and Development/The World Bank, 2018. Available online: https://www.who.int/maternal_child_adolescent/topics/quality-of-care/definition/en/. Accessed on December 24, 2018.
- The Institute of Healthcare Improvement website. Initiatives: The Triple Aim. Available online: http://www.ihi.org/education/Pages/default.aspx?gclid=EAIaIQobChMIwuyu3Zyq3gIVxbXACh2L1ws9EAAYASAAEgIIWPD_BwE. Accessed on October 27, 2018.
- McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635-45. [Crossref] [PubMed]
- Chun J, Bafford AC. History and background of quality measurement. Clin Colon Rectal Surg 2014;27:5-9. [Crossref] [PubMed]
- Parry GJ. A brief history of quality improvement. J Oncol Pract 2014;10:196-9. [Crossref] [PubMed]
- Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington (DC): National Academies Press, 2001.
- US department of health and human services. Health Resources and Services Administration (HRSA). Qual Improv 2011;1-17.
- Balas EA, Boren SA. Managing Clinical Knowledge for Health Care Improvement. Yearb Med Inform 2000;1:65-70. [PubMed]
- Reddy SI, Friedman S, Telford JJ, et al. Are patients with inflammatory bowel disease receiving optimal care? Am J Gastroenterol 2005;100:1357-61. [Crossref] [PubMed]
- Melmed GY, Siegel CA. Quality improvement in inflammatory bowel disease. Gastroenterol Hepatol (N Y) 2013;9:286-92. [PubMed]
- Esrailian E, Spiegel BM, Targownik LE, et al. Differences in the management of Crohn's disease among experts and community providers, based on a national survey of sample case vignettes. Aliment Pharmacol Ther 2007;26:1005-18. [Crossref] [PubMed]
- Spiegel BM, Ho W, Esrailian E, et al. Controversies in ulcerative colitis: a survey comparing decision making of experts versus community gastroenterologists. Clin Gastroenterol Hepatol 2009;7:168-74, 174.e1.
- Reddy SI, Friedman S, Telford JJ, et al. Are patients with inflammatory bowel disease receiving optimal care? Am J Gastroenterol 2005;100:1357-61. [Crossref] [PubMed]
- Kappelman MD, Bousvaros A, Hyams J, et al. Intercenter variation in initial management of children with Crohn’s disease. Inflamm Bowel Dis 2007;13:890-5. [Crossref] [PubMed]
- Crandall WV, Margolis PA, Kappelman MD, et al. Improved outcomes in a quality improvement collaborative for pediatric inflammatory bowel disease. Pediatrics 2012;129:e1030-41. [Crossref] [PubMed]
- Kaplan GG, McCarthy EP, Ayanian JZ, et al. Impact of hospital volume on postoperative morbidity and mortality following a colectomy for ulcerative colitis. Gastroenterology 2008;134:680-7. [Crossref] [PubMed]
- Ananthakrishnan AN, McGinley EL, Binion DG. Does it matter where you are hospitalized for inflammatory bowel disease? A nationwide analysis of hospital volume. Am J Gastroenterol 2008;103:2789-98. [Crossref] [PubMed]
- Steenkamer BM, Drewes HW, Heijink R, et al. Defining population health management: a scoping review of the literature. Popul Health Manag 2017;20:74-85. [Crossref] [PubMed]
- Dulai PS, Fisher ES, Rothstein RI. How may the transition to value-based payment influence gastroenterology: threat or opportunity? Clin Gastroenterol Hepatol 2012;10:609-11. [Crossref] [PubMed]
- Hou JK, Gasche C, Drazin NZ, et al. Assessment of gaps in care and the development of a care pathway for anemia in patients with inflammatory bowel diseases. Inflamm Bowel Dis 2017;23:35-43. [Crossref] [PubMed]
- Dulai PS, Singh S, Ohno-Machado L, et al. Population Health Management for Inflammatory Bowel Disease. Gastroenterology 2018;154:37-45. [Crossref] [PubMed]
- WHO Framework on Integrated, People-centred Health Services. Geneva: World Health Organization. Available online: https://www.who.int/servicedeliverysafety/areas/people-centred-care/en/. Accessed on October 20, 2018.
- Shekelle PG, MacLean CH, Morton SC, et al. Acove quality indicators. Ann Intern Med 2001;135:653-67. [Crossref] [PubMed]
- Berry SK, Melmed GY. Quality indicators in inflammatory bowel disease. Intest Res 2018;16:43-7. [Crossref] [PubMed]
- Siegel CA, Allen JI, Melmed GY. Translating improved quality of care into an improved quality of life for patients with inflammatory bowel disease. Clin Gastroenterol Hepatol 2013;11:908-12. [Crossref] [PubMed]
- Melmed GY, Siegel CA, Spiegel BM, et al. Quality indicators for inflammatory bowel disease: development of process and outcome measures. Inflamm Bowel Dis 2013;19:662-8. [Crossref] [PubMed]
- International Consortium for Health Outcomes Measurement (ICHOM) Web site. Inflammatory bowel disease. Available online: https://www.ichom.org/medical-conditions/inflammatory-bowel-disease/
- Bitton A, Vutcovici M, Lytvyak E, et al. Selection of Quality Indicators in IBD: Integrating Physician and Patient Perspectives. Inflamm Bowel Dis 2019;25:403-9. [Crossref] [PubMed]
- ImproveCareNow. Available online: https://www.improvecarenow.org/
- Dotson JL, Cho M, Bricker J, et al. Race Differences in Initial Presentation, Early Treatment, and 1-year Outcomes of Pediatric Crohn's Disease: Results from the ImproveCareNow Network. Inflamm Bowel Dis 2017;23:767-74. [Crossref] [PubMed]
- El-Matary W, Dufault B. Quality improvement in paediatric inflammatory bowel disease: the Manitoba experience. Acta Paediatr 2016;105:e440-2. [Crossref] [PubMed]
- El-Matary W, Stefanovici C, Van Caeseele P, et al. Detection of Cytomegalovirus in Colonic Mucosa of Children With Inflammatory Bowel Disease: Inflammatory Bowel Disease. J Pediatr Gastroenterol Nutr 2018;67:221-4. [Crossref] [PubMed]
- Crohn's & Colitis Foundation Web site. IBD Qorus. Available online: http://www.crohnscolitisfoundation.org/science-and-professionals/ibdqorus/
- Greene L, Moreo K. Quality improvement education to improve performance on ulcerative colitis quality measures and care processes aligned with National Quality Strategy priorities. BMJ Qual Improv Rep 2015;4. [Crossref] [PubMed]
- El-Matary W. Indicators of Quality of Care in Inflammatory Bowel Disease: Seeking the Right Path for Patients. Inflamm Bowel Dis 2017;23:702-3. [Crossref] [PubMed]


