
Understanding basic concepts of developmental diagnosis in children
Introduction
Child development is generally described in terms of streams or domains of development. The four domains or streams of development are, (I) motor development—gross motor and fine motor, (II) speech and language development—expressive and receptive, (III) social and emotional, and (IV) cognitive (1-12). Development in motor adaptive abilities, language and communication, and intellectual capacity provide a basis for social and emotional development (7,8,13,14). Problem solving skills is a reflection of cognitive development, which also includes visual perceptual and visual motor abilities. Development is also described in terms of its progression as either typical or atypical for the age of the child.
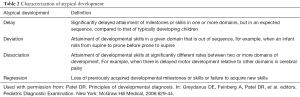
The acquisition of developmental skills is a function of interplay between development of the nervous system and other organ systems, and child’s social and physical environment and stimuli. Typical development is characterized by certain basic tenets. These are, (I) gross motor development progresses in a cephalo-caudal sequence, (II) fine motor development progresses from midline to lateral sequence, (III) primary motor patterns or primitive reflexes are integrated into more complex motor patterns to allow for later, sequential voluntary motor development, (IV) the rate of attainment of developmental skills between infants vary; however, the sequence remains the same, and (V) there is progression from generalized reflexive responses to a more specific and purposeful response pattern (4,7-9). Periodic surveillance and screening help identify infants and children who may need additional evaluation (Table 1), and the application of the basic tenets of typical development allow for an understanding of different patterns of atypical progression of development (Table 2) (1-3,7,8).

Full table
Full table
Definitions
Intelligence quotient (IQ) as measured by individually administered standardized tests, is a widely used measure of cognitive abilities or intelligence. IQ is calculated by dividing mental age (MA) by chronologic age (CA) multiplied by 100, and can be measured reliably in children ≥6 years of age (8,11,13-15). IQ is used as one criterion to define intellectual disability. In addition to sub-average IQ, the definition of intellectual disability requires the presence of limitations in adaptive functioning (as measured by individually administered standardized tests) (16-21). Adaptive functioning comprises conceptual, social, and practical adaptive skills. IQ of 70 or less with a standard error of measurement of 5 is considered to be sub-average. Because it is difficult to accurately and reliably measure IQ in children younger than 6 years of age, the term global developmental delay is used when development is significantly delayed in 2 or more domains. Developmental quotient (DQ) is calculated as follows: DQ = [developmental age (DA)] divided by CA ×100 (7,8). Significant developmental delay is defined as DQ of 70 or less. Atypical development is described as delay, deviation, dissociation or regression (Table 2) (1-3,7-10). DQ is a measure of rate of progression of development in a given domain.
Clinical presentations
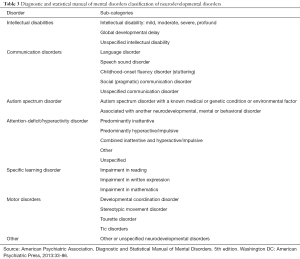
The predominant clinical presentation of atypical development varies in infants, children and adolescents. Various neurodevelopmental disorders are described based on their clinical features; the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) classification of neurodevelopmental disorders is shown in Table 3 (5).
Full table
Infants
Atypical motor development
Parents are more likely to first notice if infant fails to attain expected motor milestones. Often, parents compare infant’s development to other infants. Because typical development occurs within a range of period, most infants with apparent motor delay likely have normal variation or maturational lag (8,10). Cerebral palsy is the most significant cause of motor delay in infancy. In addition to motor delay, infants and children with cerebral palsy have abnormal tone and posture or movements (8-10,13,14,22,23). Delay in attaining motor milestones is an early sign of cerebral palsy. Other clues that parents first notice are listed in Table 4 (22,23). Other major causes of predominant motor delay during infancy include birth injury to the brain, stroke, metabolic insult affecting brain, congenital central nervous system infections and neuromuscular disorders (10,13-15,17,18).

Full table
Atypical development in social and language domains
Another area of concern in infancy and toddler age is atypical progression of development in social, cognitive and language domains. A complete evaluation is indicated in infants or toddlers with following signs: no babbling, no pointing (joint attention) or gestures by 12 months of age; no single words by 16 months; and no 2-word spontaneous phrases by 24 months (11,12,14). Absence of joint attention, the ability to attend to both and object and a person at the same time, is considered an early sign of autism (5,12). Any loss or regression of a previously acquired skill at any age is any indication for complete diagnostic evaluation including neurological, metabolic and genetic as appropriate (15). Developmental regression is often seen in infants and toddlers with autism between 18 and 24 months of age (10,12). Other significant causes of regression before 2 years of age include metabolic conditions such as disorders of amino acid metabolism, lysosomal storage disease, hypothyroidism, mitochondrial diseases, tuberous sclerosis, Lesch-Nyhan syndrome, Rett syndrome, Canavan disease, and Pelizaeus-Merzbacher disease (10). In addition to autism spectrum disorder, other conditions that should be considered in infants with predominant language, cognitive and social deficits include hearing impairment, severe cognitive deficit, genetic disorders, inborn errors of metabolism, hypothyroidism, and severe nutritional or environmental deprivation (1,3,10,15).
Children
Atypical language development
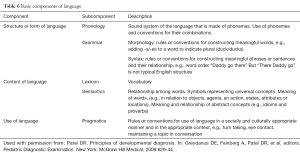
Concerns about development of speech and language (Table 5) are predominant presentations in children. In a typically developing child, intelligibility of speech progresses from about 25% by age 2 years to 100% by age 4 years. In addition to poor intelligibility for given age, persistent baby talk, mispronunciations of words or lack of spontaneous speech suggest speech and language delay (24-30). The basic components of a language are phonology, grammar, lexicon, semantics and pragmatics (Table 6); any of which can be affected in a child with atypical language development (24-30).

Full table
Full table
Autism spectrum disorder, intellectual disability, and developmental language disorder are main causes for atypical language development in a young child (9,11-14,18,20,31). Autism spectrum disorder is characterized by qualitative impairment in social relatedness, stereotypical behaviors and a spectrum of impairment in communication ability, especially social communication (5,12,32). Autism spectrum disorder can be generally recognized between 18 and 24 months of age when parents first bring their child concerned about his or her unusual behaviors or difficulty with social communication (5,12). A child with autism spectrum disorder may not be socially engaged, may demonstrate intense focus on a particular object for a prolonged period, may appear withdrawn at times, have poor eye contact, get attached to a particular object (toy), have specific rituals, and resist change in routine (5,12,32-38). A child with autism has difficulty understanding other person’s feelings, and may not engage in playing pretend games (5,12,22-38). Individuals with Asperger syndrome (also considered to be a form of high functioning autism spectrum disorder) demonstrate normal cognitive and language abilities and predominant deficits in social development (29-41).
A child with predominant cognitive deficit or intellectual disability generally has typical progression of motor development and his or her behaviors are commensurate with MA (18-20). Although a child with intellectual disability has both cognitive and adaptive functioning deficits, his or her social participation is also consistent with MA. In additional to language delay, a child with predominant cognitive deficit has difficulty problem solving and may not be able to relate their behaviors to consequences (18-20). In most cases, no specific etiology can be identified in children with intellectual disability, especially those with mild deficits; a specific cause is more likely to be identified in those with severe deficits (15,17-21). The most common cause of inherited intellectual disability is Fragile X syndrome (19,20). Other major causes of intellectual disability are fetal alcohol syndrome, lead toxicity, iron deficiency, and congenital brain malformations (15,17-21).
Developmental language disorder is characterized by predominant deficit in language development and typical development in other domains—social, motor and cognitive (24-26,30). In addition to autism and intellectual disability, the differential diagnosis of speech and language disorders should include hearing deficit, speech and voice disorders, maturational language delay, and a lack of environmental stimulation for language and learning (24-26). A bilingual home environment is not a cause for language delay. The various sub-types of developmental language disorders have been described that are based on particular aspects of the language that is affected (Table 7) (24-30).

Full table
Disorders of speech include speech sound disorder, stuttering, dysarthria, verbal dyspraxia and resonance disorders (Table 8) (5,25). Disturbance of airflow through nasopharyngeal airway results in either hypernasal or hyponasal voice; it is important to note that airflow obstruction is associated with the production of consonant sounds, and not associated with the production of vowel sounds (25). Selective mutism is not considered a language disorder, rather a specific type of anxiety disorder in which a child consistently fails to be able to speak in a given situation when he or she is expected to speak (5).

Full table
Regression of or failure to acquire expected new skills
In addition to developmental regression seen in children with autism, other conditions in which regression of skills is seen include Rett syndrome and Landau-Kleffner syndrome (LKS) (10,14). A child with Rett syndrome shows regression of acquired skills following a period of relatively typical development during infancy. Rett syndrome is an X-linked disorder predominantly affecting females (10). Other clinical features of Rett syndrome are autistic behavior, abnormal wringing hand movements, deceleration of head circumference, hyperventilation, breath holding, air swallowing, gait dyspraxia, autonomic dysfunction, inappropriate laughing, and intense eye contact (10). Often there is some recovery following a period of regression followed by further deterioration.
The clinical features of LKS are generally recognized between 3 and 8 years of age (10). Following a period of typical development during the first 3 years, the child with LKS loses language skills; whereas, no deficits are noted in cognitive or social development (10). The sleep electroencephalograph in LKS shows seizure pattern (10). Other causes of developmental regression in children older than 2 years of age include some genetic disorders, inborn errors of metabolism, and disorders of white and gray matter (10).
Early learning difficulties and behavioral symptoms
Learning difficulty and associated behavioral symptoms are most apparent first during early elementary grades. Poor academic performance is often the main parental concern. Other indications of learning difficulty include delay in completing assigned school work, inattentiveness in the classroom setting, difficulty learning new skills, and difficulty with reading and comprehension (42,43). Children with learning difficulty are also shy and reluctant to participate in activities with other children. In addition to various types of specific or developmental learning disorders other conditions to be considered in the differential diagnosis in these children include attention deficit hyperactivity disorder (ADHD), hearing or vision impairment, cognitive deficit and developmental coordination disorder (42).
Vision and hearing impairment may be associated with other developmental disabilities. A child with visual impairment might close or cover one eye; squint the eyes or frown; complaint that things are blurry or hard to see; have trouble reading or doing other close-up work, or hold objects close to eyes; blink more than usual or seem cranky when doing close-up work such as looking at a book. A child with complete or partial hearing impairment might not turn to the source of a sound from birth to 3 or 4 months of age; may not say single words, such as “dada” or “mama” by 1 year of age; turn head when he or she sees you but not if you only call out his or her name. This often is mistaken for not paying attention or just ignoring.
Developmental coordination disorder affects school-age children and persists into adolescent years (5). Difficulties in motor coordination will cause substantial impairment in academic function or activities of daily living (5). Early manifestations may include difficulty sucking and swallowing, drooling during infancy, speech difficulties and delayed motor milestones during early childhood. Parents may observe that the child has difficulties with many of the fine motor tasks such as using scissors, tying shoe laces or buttoning or unbuttoning (5). They also may drop objects, have poor handwriting, or will frequently bump into furniture or other people. Differential diagnosis in these children include ADHD, visual impairment, and intellectual disability.
Adolescents
Academic difficulties
The predominant concern in adolescents is difficulty in learning as the burden and complexity of academic work increase with advancing grade levels. Difficulty in learning may affect one or more areas of learning. Children and adolescents with specific learning disorder may present with associated behavioral symptoms. The differential diagnosis of learning disorders should include specific or developmental learning disorder, anxiety, depression, ADHD, and substance use disorders (42-57). Learning is also affected by the adequacy and quality of support system and instructions. Nutritional and psychosocial factors can also affect learning and academic performance.
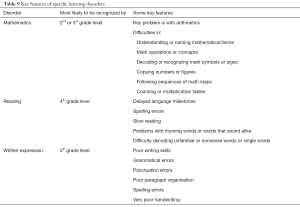
Specific or developmental learning disorder is diagnosed when scores on an individually administered standardized achievement tests (in reading, mathematics, or written expression) are substantially below that expected for the child’s age, intelligence and education level (5,43). Non-verbal specific learning disorder is characterized by difficulty in problem solving ability, and deficits in visual-spatial and visual-perceptual abilities; language-based skills and intelligence are normal. Key features of reading disorder, mathematics disorder and disorder of written expression are summarized in Table 9 (42-58).
Full table
Clinical approach
Surveillance
Developmental and behavioral surveillance is recommended at every preventive or health maintenance visit (1,11). Information should be obtained from multiple sources including care givers and parents, teachers, and academic performance reports. A detailed prenatal, birth, perinatal, neonatal, and developmental history is essential aspect in the diagnostic evaluation of children with atypical development. Parental concerns regarding child’s development and behavior provides a basis for the direction of evaluation. The developmental history should assess areas of typical and atypical progression of milestones in all streams or domains of development—gross motor, fine motor, speech and language, and social (1).
Although, specific emphasis on a particular aspect of physical examination is guided by the presenting symptoms, some aspects are of fundamental consideration in all children. These include serial measurements of growth parameters—height, weight, head circumference, visual acuity, hearing, and a thorough search for congenital anomalies and dysmorphic features. The growth parameters should be plotted on appropriate graphs. In older children and adolescents mental status examination should be included and in adolescents external genital examination sexual maturity rating should be noted.
The pattern of atypical progression of development—delay, dissociation, deviation, regression—is ascertained based on the information obtained from the history and physical examination. Developmental maturation and behavior of the child are closely linked and any evaluation of child’s development should include a behavioral history. Child’s interactions and behavior, both in familiar (home, school) and unfamiliar (community) settings, should be ascertained. Information should be obtained about child’s interactions with peers, parents, other care givers, teachers, and other adults (1). The behavioral history provides the basis to describe any atypical pattern of child’s behavior, such as aggression, impulsivity, decreased social engagement, repetitive behaviors or self-injurious behavior (1). Behavior is generally assessed based on direct observation, spontaneous activities or responsive behaviors across different settings (1). As part of surveillance, information should be obtained about possible risk and protective factors relative to child’s developmental and behavioral concerns (1,3,11).
Screening
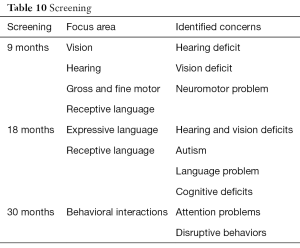
Developmental screening that screen across all streams of development with appropriate standardized screening instrument is recommended as part of the periodic health maintenance examinations in the primary care setting at 9, 18, 24 or 30 months of age (Table 10) (1,11). Although screening is across all streams, certain areas are of specific focus at each visit. In addition, autism specific screening is recommended at 18- and 24-month visits (1,11,12). Examples of standardized tools for general developmental screening, general behavioral screening, language screening, and autism screening are listed in Table 11 (59-67).
Full table

Full table
It is important to use standardized, validated screening tool to reduce the false positive and false negative results, which can have implications for further evaluation. A systematic review analyzed 11 studies that described developmental screens performed by primary care physicians (6). This review determined the sensitivity of these screens to range between 14% and 54% while their specificities ranged between 69% and 100%. There was 1 outlier in this review with a sensitivity of 85% and a specificity of 61%. Sensitivity of the developmental screenings, excluding the outlier, was consistently low. Thus, developmental screens correctly identified children with developmental delays a low number of times. On the other hand, the specificity of the developmental screens was up to the standards of 70%.
Evaluation
A more comprehensive evaluation is guided by findings on developmental surveillance and screening. Specific clinical psychological or neuropsychological evaluation and psychological testing should be performed by clinical psychologists with appropriate expertise and experience in the evaluation of children with atypical development. Based on findings on clinical history and physical examination further medical evaluation may be indicated. Such evaluation may include neuroimaging, electroencephalography, tests for genetic disorders, and specific laboratory tests for inborn errors of metabolism and should be considered in consultation with appropriate medical specialists (11,12,14,15).
Both hearing screening and vision screening are part of periodic health maintenance or preventive health visits. In addition, parental concerns about a child’s hearing or vision are indications for further audiological testing and complete vision evaluation. In the United States, based on current guidelines, universal hearing screening is done in all newborns by 1 month of age, with a follow-up audiological testing, if indicated, by 3 months of age. Treatment intervention is started by 6 months of age in any infant identified having a hearing loss. Similarly, any concerns about a child’s speech and language development is an indication for complete evaluation by a speech-language pathologist. Often, no specific signs or symptoms are evident suggestive of a developmental disorder; however, based on their observations, parents remain concerned about their child’s development. In these cases, a further evaluation is indicated.
Principles of management
The key principle of management of children with developmental concerns is early intervention. The content and delivery of early intervention services may vary in different health systems. For example, in the United States, many federal and state regulations provide a basis and framework for such services to be delivered within the context of the local formal education system (68,69). When a developmental problem is recognized, the child is enrolled in the early intervention service, while further evaluation may proceed at the same time. This approach is based on the principles of response to intervention concept (68,69). Rather than waiting for a definitive diagnosis, intervention is implemented and further course of action is guided by response to the intervention. Among the major services included in the intervention programs are occupational therapy, physiotherapy and speech therapy. School age children are evaluated further to develop individualized learning plans that include various remediation, accommodation or psychoeducational strategies (43). In addition, environmental risk factors are considered and addressed in home, school and community settings as appropriate. When a specific developmental or behavioral disorder is identified, treatment is tailored to the condition and may include specific behavioral and pharmacological interventions.
Conclusions
The development from infancy through adolescence is described under four main streams or domains of development, namely, (I) gross and fine motor, (II) speech-language, (III) social-emotional, and (IV) cognitive. However, overall typical development progresses concomitantly in all domains. Typical development follows certain well recognized patterns, an understanding of which, helps us identify atypical patterns of developmental progression. Developmental delay, deviation, dissociation and regression are recognized as atypical patterns of development. The predominant clinical presentations of atypical patterns of development vary depending up on the age of the infant or child at presentation. The DQ is used as a measure of rate of development in any given domain; similarly, intelligence quotient is used as measure of intelligence. The clinical approach to developmental diagnosis is based on the principles of regular surveillance, periodic screening and diagnostic evaluation when indicated based on finding on surveillance and screening. Early recognition of atypical development is important as early treatment interventions, based on response to intervention model, have been shown to the most effective.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest:DRP serves as the unpaid Deputy Editor-in-Chief of TP and the unpaid Guest Editor of the focused issue “Neurodevelopmental and Neurobehavioral Disorders in Children”. TP. Vol 9, Supplement 1 (February 2020). Section on clinical presentations is adapted with permission from author’s previous work: Patel DR. Principles of developmental diagnosis. In: Greydanus DE, Feinberg A, Patel DR, et al. editors. Pediatric Diagnostic Examination. New York: McGraw Hill Medical, 2006:629-44. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lipkin PH. Developmental and behavioral surveillance and screening. In: Kliegman RM, St. Geme JW. Nelson Textbook of Pediatrics. 21st edition. Philadelphia: Elsevier, 2019:159-61.
- Pellegrino L. Child development. In: Batshaw ML, Roizen NJ, Pellegrino L. editors. Children with Disabilities. 8th edition. Baltimore: Paul Brookes Publishing, 2019:177-98.
- Myers SM. Diagnosing developmental disabilities. In: Batshaw ML, Roizen NJ, Pellegrino L. editors. Children with Disabilities. 8th edition. Baltimore: Paul Brookes Publishing, 2019:199-224.
- Dixon SD, Stein MT. editors. Encounters with Children: Pediatric Behavior and Development. 4th edition. Philadelphia: Elsevier, 2006.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Washington DC: American Psychiatric Press, 2013:33-86.
- Sheldrick RC, Merchant S, Perrin EC. Identification of developmental-behavioral problems in primary care: a systematic review. Pediatrics 2011;128:356-63. [Crossref] [PubMed]
- Pellegrino L. Patterns in development and disability. In: Batshaw ML, Pellegrino L, Roizen NJ. editors. Children with developmental disabilities. 6th edition. Baltimore: Paul H Brookes, 2007:217-28.
- Accardo PJ, Accardo JA, Capute AJ. A neurodevelopmental perspective on the continuum of developmental disabilities. In: Accardo PJ. editor. Capute and Accardo’s neurodevelopmental disabilities in infancy and childhood. 3rd edition. Baltimore: Paul H Brookes, 2008:3-26.
- Illingworth RS. The development of the infant and young child: normal and abnormal. 7th edition. London: Churchill Livingstone, 1980:53-72,108-207.
- Pina-Garza JE, James KC. Psychomotor retardation and regression. In: Pina-Garza JE, James KC. editors. Fenichel’s Clinical Pediatric Neurology. 8th edition. Philadelphia: Elsevier, 2019:115-49.
- Council on Children With Disabilities; Section on Developmental Behavioral Pediatrics; Bright Futures Steering Committee, et al. Identifying infants and young children with developmental disorders in the medical home: an algorithm for developmental surveillance and screening. Pediatrics 2006;118:405-20. [Crossref] [PubMed]
- Johnson CP, Myers SM. Council on Children with Disabilities. Identification and evaluation of children with autism spectrum disorders. Pediatrics 2007;120:1183-215. [Crossref] [PubMed]
- Shevell M. Global developmental delay and mental retardation or intellectual disability: conceptualization, evaluation, and etiology. Pediatr Clin North Am 2008;55:1071-84. xi. [Crossref] [PubMed]
- Shevell M, Ashwal S, Donley D, et al. Practice parameter: evaluation of the child with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and The Practice Committee of the Child Neurology Society. Neurology 2003;60:367-80. [Crossref] [PubMed]
- Michelson DJ, Shevell MI, Sherr EH, et al. Evidence report: Genetic and metabolic testing on children with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2011;77:1629-35. [Crossref] [PubMed]
- American Association of Intellectual and Developmental Disabilities. Intellectual Disability: Definition, Classification, and Systems of Supports. 11th edition. Washington, DC: Am Assoc Intellect Dev Disabil, 2010.
- Luckasson R, Borthwick-Duffy S, Buntix WH, et al. Mental retardation: definition, classification, and system of supports. 10th edition. Washington, DC: American Association on Mental Retardation, 2002.
- Purugganan O. Intellectual Disabilities. Pediatr Rev 2018;39:299-309. [Crossref] [PubMed]
- Shapiro BK, O’Neill ME. Developmental delay and intellectual disability. In: Kliegman RM, St. Geme JW. editors. Nelson Textbook of Pediatrics. 21st edition. Philadelphia: Elsevier, 2020:283-93.
- Intellectual disability. Available online: http://www.cdc.gov/ncbddd/dd/mr3.htm. Accessed 2019 Nov 12.
- van Karnebeek CD, Jansweijer MC, Leenders AG, et al. Diagnostic investigations in individuals with mental retardation: a systematic literature review of their usefulness. Eur J Hum Genet 2005;13:6-25. [Crossref] [PubMed]
- Cerebral palsy. Available online: 2019 Nov 12.https://www.cdc.gov/ncbddd/cp/index.htmlaccesses
- Paneth N. Establishing the diagnosis of cerebral palsy. Clin Obstet Gynecol 2008;51:742-8. [Crossref] [PubMed]
- Stuart S. Communication disorders. In: Batshaw ML, Pellegrino L, Roizen NJ. editors. Children with developmental disabilities. 6th edition. Baltimore: Paul H Brookes, 2007:313-24.
- Sharp HM, Hillenbrand K. Speech and language development and disorders in children. Pediatr Clin North Am 2008;55:1159-73. [Crossref] [PubMed]
- Simms MD. Language disorders in children: classification and clinical syndromes. Pediatr Clin North Am 2007;54:437-67. [Crossref] [PubMed]
- McLeod S, McKinnon DH. Prevalence of communication disorders compared with other learning needs in 14,500 primary and secondary school students. Int J Lang Commun Disord 2007;42:37-59. [Crossref] [PubMed]
- Lindsay G, Dockrell JE, Strand S. Longitudinal patterns of behaviour problems in children with specific speech and language difficulties: child and contextual factors. Br J Educ Psychol 2007;77:811-28. [Crossref] [PubMed]
- Mawhood L, Howlin P, Rutter M. Autism and developmental receptive language disorder- a follow-up comparison in early adult life. I: Cognitive and language outcomes. J Child Psychol Psychiatry 2000;41:547-59. [Crossref] [PubMed]
- Nelson NW. Language and literacy disorders: Infancy through adolescence. Boston: Allyn Bacon Pearson Imprint, 2010.
- Baio J, Wiggins L, Christensen DL, et al. Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2014. MMWR Surveill Summ 2018;67:1-23. [Crossref] [PubMed]
- Centers for Disease Control and Prevention. Autism spectrum disorders. Available online: https://www.cdc.gov/ncbddd/autism/index.htmlaccessed. 2019 Nov 12.
- Rapin I, Tuchman RF. Autism: definition, neurobiology, screening, diagnosis. Pediatr Clin North Am 2008;55:1129-46. [Crossref] [PubMed]
- Wing L, Potter D. The epidemiology of autistic spectrum disorders: is the prevalence rising? Ment Retard Dev Disabil Res Rev 2002;8:151-61. [Crossref] [PubMed]
- Hughes JR. A review of recent reports on autism: 1000 studies published in 2007. Epilepsy Behav 2008;13:425-37. [Crossref] [PubMed]
- Matson JL, Shoemaker M. Intellectual disability and its relationship to autism spectrum disorders. Res Dev Disabil 2009;30:1107-14. [Crossref] [PubMed]
- de Bildt A, Sytema S, Kraijer D, et al. Prevalence of pervasive developmental disorders in children and adolescents with mental retardation. J Child Psychol Psychiatry 2005;46:275-86. [Crossref] [PubMed]
- Folstein SE. The clinical spectrum of autism. Clin Neurosci Res 2006;6:113-7. [Crossref]
- Battaglia A, Carey JC. Etiologic yield of autistic spectrum disorders: A prospective study. Am J Med Genet Part C 2006;142C:3-7. [Crossref] [PubMed]
- Cohen D, Pichard N, Tordjman S, et al. Specific genetic disorders and autism: clinical contribution towards their identification. J Autism Dev Disord 2005;35:103-16. [Crossref] [PubMed]
- Myers SM, Johnson CP. Council on Children with Disabilities. Management of children with autism spectrum disorders. Pediatrics 2007;120:1162-82. [Crossref] [PubMed]
- Lagae L. Learning disabilities: definitions, epidemiology, diagnosis, and intervention strategies. Pediatr Clin North Am 2008;55:1259-68. [Crossref] [PubMed]
- Church RP, Lewis MEB. Specific learning disabilities, In: Batshaw ML, Pellegrino L, Roizen NJ. editors. Children with developmental disabilities. 8th edition. Baltimore: Paul H Brookes, 2019:395-422.
- Shaywitz BA, Shaywitz SE. Dyslexia. Continuum, 2001:17-36.
- Shaywitz SE, Shaywitz BA. Dyslexia. In: Kliegman RM, St. Geme JW. editors. Nelson Textbook of Pediatrics. 21st edition. Philadelphia: Elsevier, 2020:267-26946.
- Grizzle KL. Developmental dyslexia. Pediatr Clin North Am 2007;54:507-23. [Crossref] [PubMed]
- Shelley-Tremblay J, O'Brien N, Langhinrichsen-Rohling J. Reading disability in adjudicated youth: prevalence rates, current models, traditional and innovative treatments. Aggress Violent Behav 2007;12:376-92. [Crossref]
- Shalev RS. Dyscalculia. Continuum, 2001:60-73.
- Shalev RS, Gross-Tsur V. Developmental dyscalculia. Pediatr Neurol 2001;24:337-42. [Crossref] [PubMed]
- Butterworth B. The development of arithmetical abilities. J Child Psychol Psychiatry 2005;46:3-18. [Crossref] [PubMed]
- Shalev RS, Manor O, Gross-Tsur V. Developmental dyscalculia: a prospective six-year follow-up. Dev Med Child Neurol 2005;47:121-5. [Crossref] [PubMed]
- Shalev RS, Auerbach J, Manor O, et al. Developmental dyscalculia: prevalence and prognosis. Eur Child Adolesc Psychiatry 2000;9 Suppl 2:II58-64. [Crossref] [PubMed]
- Katusic SK, Colligan RC, Weaver AL, et al. The forgotten learning disability: Epidemiology of written-language disorder in a population-based birth cohort (1976-1982), Rochester, Minnesota. Pediatrics 2009;123:1306-13. [Crossref] [PubMed]
- Deuel RK. Dysgraphia. Continuum, 2001:37-59.
- Rosenberger PB. Management of learning disabilities. Continuum 2001.125-30.
- Goldston DB, Walsh A, Arnold EM, et al. Reading problems, psychiatric disorders, and functional impairment from mid- to late adolescence. J Am Acad Child Adolesc Psychiatry 2007;46:25-32. [Crossref] [PubMed]
- Feldman E, Levin BE, Lubs H, et al. Adult familial dyslexia: A retrospective developmental and psychosocial profile. J Neuropsychiatry Clin Neurosci 1993;5:195-9. [Crossref] [PubMed]
- Soares N, Evans T, Patel DR. Specific learning disability in mathematics: a comprehensive review. Transl Pediatr 2018;7:48-62. [Crossref] [PubMed]
- Squires J, Potter L, Bricker D. The ASQ users’ guide. 3rd edition. Baltimore: Paul H Brooks Publishing, 2009.
- Glascoe FP, Marks KP, Poon K, et al, eds. Identifying and addressing developmental-behavioral problems: a practical guide for medical and non-medical professionals, trainees, researchers, and advocates. Nonensville: TN, PEDStest.com, 2013.
- Survey of Wellbeing of Young Children. Accessed Nov 1, 2019. Available online: https://www.theswyc.org/
- Squires J, Bricker DD, Twombly E. Ages and Stages Questionnaires: Social-Emotional-2 (ASQ:SE-2): a parent-completed, child-monitoring system for social-emotional behaviors. Baltimore: Paul Brooks Publisching, 2016.
- Briggs-Gowan MJ, Carter AS, Irwin JR, et al. The Brief-Infant Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. J Pediatr Psychol 2004;29:143-55. [Crossref] [PubMed]
- Gardner W, Lucas A, Kolko DJ, et al. Comparison of the PSC-17 and alternative mental health screens in an at-risk primary care sample. J Am Acad Child Adolesc Psychiatry 2007;46:611-8. [Crossref] [PubMed]
- Wetherby AM, Prizant BM. Communication and Symbolic Behavior Scales: Developmental Profile. Baltimore: Paul Brooks Publishing, 2002.
- Robins DL, Casagrande K, Barton M, et al. Validation of the Modified Checklist for Autism in Toddlers, Revised with Follow-up (M-CHAT-R/F). Pediatrics 2014;133:37-45. [Crossref] [PubMed]
- Rutter M, Bailey A, Lord C. The Social Communication Questionnaire (SCQ) manual. Los Angles: Western Psychological Services, 2003.
- Lipkin PH, Okamoto J. Council on Children with Disabilities, et al. The Individuals With Disabilities Education Act (IDEA) for Children With Special Educational Needs. Pediatrics 2015;136:e1650-62. [Crossref] [PubMed]
- National Center for Learning Disabilities Response to Intervention Acrion Network. Available online: http://www.rtinetwork.org/learn/what. Accessed 2019 Nov 12.


