Intrathyroidal ectopic thymus in 8-year-old girl: a case report
Introduction
Ectopic intrathyroidal thymic tissue is a rare congenital variant where most cases are incidentally identified. Ultrasonography is recommended as the reference standard for confirmation the presence of thyroid nodules (1-3). So far, a few cases of ectopic intrathyroidal thymus tissue have been reported (1,2). According to previous reports, ectopic thymus tissue in the thyroid showed similar echogenicity to a normal thymus. Several cases of intrathyroidal thymic tissue that mimic a thyroid nodule have been reported (4). We describe a case of two thyroid nodules, which were found pathologically to be ectopic thymuses, which had connections to the mediastinal thymus gland.
Case presentation
The 8-year-old girl underwent an ultrasound examination in a different hospital for sore throat. After being diagnosed with her thyroid disease, she was admitted to our hospital. The medical history of the patient was insignificant, and in particular, there was no previous irradiation of the neck.
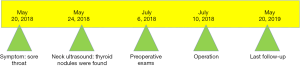
On physical examination, no abnormalities were found. The thyroid gland seemed to be normal in size, and there were no palpable cervical nodes. Neck ultrasonography (US) was performed in our hospital with a 12-MHz linear array transducer of an LOGIQ 9 scanner (GE, Milwaukee, WI USA). The US examinations were reviewed on a Centricity PACS workstation (GE Healthcare, Milwaukee, WI, USA). US examination demonstrated a thyroid gland of normal size as well as the presence of two inhomogeneous nodules with “micro-calcifications” in both lobes (Figure 1A,B). Both of them had irregular margins, and the continuity of the dorsal thyroid membrane was interrupted. Other nodule in region IV of the left neck had an inhomogeneous echotexture; furthermore, a hyperechoic foci was identified in the nodule. Thymic tissue of the patient was normal (Figure 1C). She subsequently underwent a contrast-enhanced computed tomography (CT) scan (Figure 1D,E), and no suspicious lymph nodes were found.
Her past history was significant for allergic purpura. Upon admission, she underwent detailed thorough laboratory evaluation, in addition to performing a blood tests and chest X-ray, which were unremarkable.
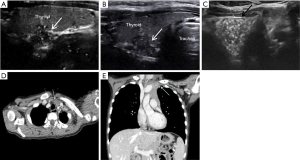
The patient underwent a total thyroidectomy with no notable incidences during the operation. Upon dissection of the specimen, two white focuses were identified in the right and left lobes, which showed a maximum diameter of 0.9 and 1.1 cm respectively. Unfortunately, after surgery, intrathyroidal ectopic thymus was confirmed by pathology and thyroid hormone replacement therapy was performed in her life.
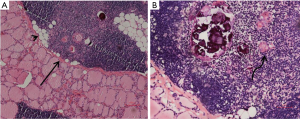
According to microscopic findings, both of the two nodules were composed of ectopic thymic tissue with noticeable Hassall’s corpuscles (Figure 2A,B). Hassall’s corpuscle is the marker of ectopic thymic tissue. In addition, the timeline of this patient’s historical and current information was made as Figure 3.
Discussion
The thymus and inferior parathyroid glands are derived from the third pharyngeal pouches. From the sixth week to the second month of gestation, the pouches migrate together in a caudal and medial direction until they reach their usual locations (5). During their migration, the tail portion of the thymus breaks up into small pieces and commits to descending into the thorax (named the thymopharyngeal tract); however, after some time it usually disappears (6). During its migration, the thymic remnants can be left along the path, and the ectopic thymic tissue may manifest as a neck mass or an incidentally detected mass (7).
In children, US is the modality of choice for evaluating an intrathyroid ectopic thymus because it is a noninvasive, cheap, accurate method and does not expose the patients to ionizing radiation. The US appearance of ectopic thymus is similar to that of a normal thymus (7,8). The possibility of an intrathyroid ectopic thymus should be considered when a mid-low lying intrathyroid lesion, that’s associated with a fusiform shape and multiple linear or punctate internal echoes is detected on US in children. The sonographic appearance of an ectopic thymus shows an echotexture similar to that of the normotopic thymus. Normotopic thymus should be identified and compare the sonographic appearance with that of the nodule (8).The multiple small internal dots echoes in an intrathyroid ectopic thymus could be misinterpreted as micro-calcifications of a malignant thyroid nodule, although the echogenic dots are created by fat, which are located against lymphoid tissue, rather than micro-calcifications (9). The echogenic dots can have similar US mimic characteristics of papillary thyroid carcinoma (PTC). There are several reported cases of intrathyroid ectopic thymus in adults and children, which failed diagnoses were made by ultrasound examination, but the pathology was confirmed by FNA. In addition, current literatures show that clinicians’ understanding of this rare variation is gradually increasing.
In our case, the thyroid nodules showed an ill-defined margin with multiple hyperechoic foci in the mid-portion of the two lobes; moreover, the US presentations were very similar with malignant thyroid nodules, with marked hypoechogenicity, irregular margins, microcalcifications, and taller rather than wide shapes (5,10). We performed a total thyroidectomy to confirm the differential diagnosis of intrathyroidal thymic tissue and to exclude thyroid malignancy because her parents requested surgical therapy and refused fine needle aspiration (FNA). In this case, we took full advantage of CT and ultrasound examination to show the accurate shape of the lesions, so as to analyze the lesions as accurately as possible. There is no doubt that this was very important for the diagnosis and retrospective study of the disease. Limitation in this case was that we did not use other ultrasound techniques (such as ultrasound elastic imaging or contrast-enhanced ultrasound) to do further research for this case in order to distinguish the thyroid ectopic thymic tissue from thyroid carcinoma. And FNA was also not accepted.
In conclusion, intrathyroidal thymic tissue is rare and may be confused with a malignant thyroid nodule because of hyperechoic dots that mimic calcifications. In children, intrathyroidal thymic tissue should be considered as part of the differential diagnosis for thyroid nodules. The sonographic findings of an ectopic thymus were similar to those of the thymus; therefore, we should be familiar with US findings of normal thymic tissue. If sonography results are inconclusive and further evaluation is required, other techniques (such as ultrasound elastic imaging or contrast-enhanced ultrasound or FNA, etc.) may be useful for confirmative diagnosis.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient and her parent for publication of this manuscript and any accompanying images.
References
- Frates MC, Benson CB, Dorfman DM, et al. Ectopic Intrathyroidal Thymic Tissue Mimicking Thyroid Nodules in Children. J Ultrasound Med 2018;37:783-91. [Crossref] [PubMed]
- Park SH, Ryu CW, Kim GY, et al. Intrathyroidal thymic tissue mimicking a malignant thyroid nodule in a 4-year-old child. Ultrasonography 2014;33:71-3. [Crossref] [PubMed]
- Kim A, Kang SH, Bae YK. Ectopic intrathyroidal thymus accompanied by intrathyroidal parathyroid as a cause of a solitary thyroid nodule in adult. Int J Clin Exp Pathol 2014;7:6375-8. [PubMed]
- Patel MN, Komlos M, Racadio JM. Intrathyroidal thymic tissue mimicking a thyroid nodule in a 4-year-old child. J Clin Ultrasound 2013;41:319-20. [Crossref] [PubMed]
- Hernandez-Cassis C, Poniecka A, Vogel CK, et al. A six-year-old boy with a suspicious thyroid nodule: intrathyroidal thymic tissue. Thyroid 2008;18:377-80. [Crossref] [PubMed]
- Lignitz S, Musholt TJ, Kreft A, et al. Intrathyroidal thymic tissue surrounding an intrathyroidal parathyroid gland, the cause of a solitary thyroid nodule in a 6-year-old boy. Thyroid 2008;18:1125-30. [Crossref] [PubMed]
- Durmaz E, Barsal E, Parlak M, et al. Intrathyroidal ectopic thymic tissue may mimic thyroid cancer: a case report. J Pediatr Endocrinol Metab 2012;25:997-1000. [Crossref] [PubMed]
- Vlachopapadopoulou EA, Vakaki M, Karachaliou FE, et al. Ectopic Intrathyroidal Thymus in Childhood: A Sonographic Finding Leading to Misdiagnosis. Horm Res Paediatr 2016;86:325-9. [Crossref] [PubMed]
- Yildiz AE, Ceyhan K, Sıklar Z, et al. Intrathyroidal Ectopic Thymus in Children: Retrospective Analysis of Grayscale and Doppler Sonographic Features. J Ultrasound Med 2015;34:1651-6. [Crossref] [PubMed]
- Aydin S, Fatihoglu E, Kacar M. Intrathyroidal ectopic thymus tissue: a diagnostic challenge. Radiol Med 2019;124:505-9. [Crossref] [PubMed]