A rare case report of acquired rubber band syndrome due to an unnoticed rubber band on a baby’s ankle
Introduction
Acquired rubber band syndrome is a rare condition that easily lead to disastrous consequences in younger children, who are worn rubber band for decorative purpose. When the band is worn for a long duration, it may cause constrictive effects on limbs and even burrows through the skin and soft tissues and resulting in distal edema, compartment syndrome and impaired limbs’ functions. Previous cases reported the acquired rubber band syndrome were occurred on children’s wrist mostly, but we should not ignore that the rubber band syndrome can also occurred on children’s ankle. In this report, we introduced a case of a 7-month-old girl presented symptoms of redness and swelling of the left ankle and diagnosis with the left ankle soft tissue infection at local hospital. After receiving ineffective anti-infection treatment for 1 month, the girl was transferred to our hospital. After we gave her a careful examination, a rubber band lying in the left ankle crease was found, and it had cut through the skin and soft tissues. Thus, the girl was taken an emergency surgery to remove the band, and she got excellent recovery postoperatively. Previous reports suggest the cardinal features of acquired rubber band syndrome is a linear constricting scar around the joint, however, this feature may not obvious for the band hidden in a skin crease. Therefore, if children presented skin infection symptoms surrounding the crease, clinicians should keep vigilant and rule out a rubber band which was around and hidden in the skin crease. We present the following case in accordance with the CARE Guideline (1).
Case presentation
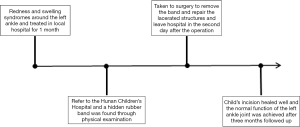
A 7-month-old girl presented with redness and swelling around her left ankle for 2 months. One month earlier, the girl with the diagnosis of left ankle soft tissue infection and had undergone antibiotic treatment at a local hospital. After received the conservative therapy for 1 month, her symptoms were failed respond to the antibiotic treatment and worsened progressively. To get further treatment, she was bought to our hospital by her parents. On physical examination, the girl presented a linear circumferential constriction mark in the left ankle crease, with symptoms of redness and swelling. She was in good health without fever, lymphangitis or lymphadenopathy symptoms, the capillary filling was normal and active movements of the toes were present. When opening the ankle crease, a hidden rubber band was found and the surrounding soft tissues were lacerated (Figure 1). On further probing, girl’s parents said the rubber band may from a sock and they had not noticed it before. Therefore, the girl was performed an emergency surgery with the purpose to remove the rubber band and repair the lacerated tissues. Postoperatively, the symptoms of redness and swelling in the left ankle disappeared gradually, the girl was discharged on the second postoperative day. The redness and swelling syndromes of the left ankle was disappeared, operative incision healing well and the normal function of the left ankle joint was achieved after three months followed up (Figure 2).

Discussion
The present case emphasizes a rare condition of unnoticed rubber band in the ankle contributing to rubber band syndrome in an infant. Rubber band syndrome is a rare condition found in small children who mainly live in specific geographical regions (2). The rubber bands are tied around wrist, ankle, arm or fingers of children for decorative purpose or on religious regions (3). Sometime, a rubber band was accidently worn by the child or likely to lie hidden in the skin crease that the parents may forgot to release it. Along with the increasing in children’s limbs, the band can slowly breach the soft tissues and this pathological process is surprisingly painless or without neurovascular symptom (2,3).
Rubber band syndrome was first reported in 1965 by Hogeboom (4). So far, there are only a few cases were reported in English, and all the reported cases occurred in children’s wrist (2-12). In this case, a 7-month-old girl presented infection symptoms and was diagnosed with soft tissue infection in her left ankle. However, she failed respond to antibiotic treatment until the remaining rubber band was found. As the symptoms arising by the rubber band may mimic several pathologies, such as infection, congenital constriction bands or compartment syndrome, thus it is hard to distinguish the differential diagnosis. Some previous reports suggested ultrasound or magnetic resonance imaging can be a useful investigation to localize the rubber band, especially for that have penetrated tendons or neurovascular structures (7-12). In this report, although the rubber band was remained in the superficial layer of myofascia, the skin crease covered it and caused a misdiagnosis at first. Thus, doctors should raise a clinical suspicion when encounter a child presented an infectious disease which surrounds the skin crease, and a careful examination should be carried out to rule out the unnoticed band which has burrowed into the soft tissues.
Previous reports suggested rubber band constriction can cause compartment syndrome, especially for the cases presented more acute (2,4,5,9). Although some signs and symptoms such as increased pain, loss of digital motion, and continued swelling can help to detect the impending compartment syndrome, for the younger age of the child these signs may confuse doctors to make right decisions. If the diagnosis of compartment syndrome is uncertain, some researchers suggested the compartment pressures should be performed and the pressures of 30 to 45 mmHg are a relative indication for fasciotomy of the affected limb (9,13). In this report, the girl presented a good capillary filling of her toes that we did not perform fasciotomy during the operation, and this is a limitation that may increase the risk of compartment syndrome. In some other reports, they presented the impending compartment syndrome cases caused by a rubber band constriction at the wrist (5,6,9,12). Under early intervention, these acute cases can get a good functional outcome, but we still can not take rubber band constriction lightly and should prompt recognition to prevent the devastating effect of compartment syndrome.
Conclusions
To my knowledge, it is the first report regarding the rubber band constriction contributed to rubber band syndrome occurred at the lower limb. Owing to the rubber band hidden by the skin creases or burrowed into the soft tissues, it was not easily distinguished the rubber band syndrome from other pathologies. Therefore, it is necessary to pay attention to the details of physical examination and even utilize extra-investigative measures to rule out the possibility of the foreign body, for instance, an unnoticed rubber band.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The child’s parents agreed the informed consent for the publication of the report, and the accompanying images. They read the submission version of the report, and confirmed the report’s content was correct to the best of their knowledge.
References
- Riley DS, Barber MS, Kienle GS, et al. CARE guidelines for case reports: explanation and elaboration document. J Clin Epidemiol 2017;89:218-35. [Crossref] [PubMed]
- Arora A, Agarwal A. Dhaga syndrome: a previously undescribed entity. J Bone Joint Surg Br 2004;86:282-4. [Crossref] [PubMed]
- Agarwal A, Kant KS, Verma I. The rubber band syndrome: the forgotten rubber band in the wrist. Hand Surg 2013;18:407-10. [Crossref] [PubMed]
- Hogeboom FE, Stephens KA. The dangerous rubber band. J Dent Child 1965;32:199-201. [PubMed]
- Gaur SC, Swarup A. Progressive constriction band caused by black magic thread. J Hand Surg Br 1991;16:349. [Crossref] [PubMed]
- Kumar KM, Shankarappa M. Rubber band syndrome of the arm. J Hand Microsurg 2013;5:83. [Crossref] [PubMed]
- Kumar M, Sharma KK, Chauhan LK, et al. Rubber Band (Dhaga) Syndrome of the Wrist. Indian J Pediatr 2018;85:1136-7. [Crossref] [PubMed]
- Kumar P, Kumar B, Singh K. A constriction ring of the thigh secondary to a rubber band. Plast Reconstr Surg 1995;95:209-10. [Crossref] [PubMed]
- McIver MA, Gochman RF. Elastic bands on the wrist: a not so "silly" complication. Pediatr Emerg Care 2011;27:428-9. [Crossref] [PubMed]
- Meier R, Haug L, Surke C, et al. Acquired Constriction Ring: A Case of Rubber Band Syndrome. Pediatr Emerg Care 2019;35:e113-5. [Crossref] [PubMed]
- Sreekanth R, Khanapur RI, Thomas BP. The elastic band (Dhaga) syndrome: physicians and surgeons be aware. J Hand Surg Am 2014;39:810-1. [Crossref] [PubMed]
- Aggarwal AN, Kini SG, Arora A, et al. Rubber band syndrome--high accuracy of clinical diagnosis. J Pediatr Orthop 2010;30:e1-4. [Crossref] [PubMed]
- Bae DS, Kadiyala RK, Waters PM. Acute compartment syndrome in children: contemporary diagnosis, treatment, and outcome. J Pediatr Orthop 2001;21:680-8. [Crossref] [PubMed]