
A clinical primer on intellectual disability
Introduction
Deficits in intellectual and adaptive functioning are the main characteristics of intellectual disability with a reported prevalence between 1% and 3% of the population with some regional variations (1,2). By definition, the onset of intellectual and adaptive deficits has their onset during the developmental period from infancy thorough adolescence. For simplicity, we have used the term persons in this review to include infants, children, adolescents and adults. Also, we recognize that different definitional criteria use the equally valid term intellectual developmental disorder instead of the term intellectual disability to describe the range of disorders of deficits in intellectual and adaptive functioning.
Most persons with intellectual disability have mild intellectual disability, for which an underlying biologic cause is less likely to be identified; whereas, a small percentage of persons who have severe to profound intellectual deficit, an underlying biologic cause is highly likely to be identified (1-4). In addition to clinical evaluation, both the cognitive ability and adaptive functioning are ascertained based on individually administered standardized tests. The effective delivery of healthcare for persons with intellectual disability requires participation and coordination between many different medical as well as other related disciplines and agencies that provide support services for persons with intellectual disability.
In most countries various laws, acts or regulations provide the framework for the legal rights of persons with disabilities, organization of community based support and intervention services, and variable levels of governmental and non-governmental funding for various support services—intervention, educational, vocational, social and other services—for persons who have intellectual and other developmental disabilities (1-4). In the clinical practice setting, the medical practitioner takes a lead role in medical evaluation and treatment as well as providing ongoing preventive healthcare for persons with intellectual disability. Additionally, the medical practitioner also plays an essential role in coordinating appropriate consultations with other specialists, as well as in facilitating access and care through community-based agencies and person.
Intellectual disability is best considered within the broader framework of disability in general. The conceptual framework and definition of disability has evolved over the years from a predominantly medical model to a broader model that encompasses and functionally merges the medical, social and functional aspects of disability (5-7). This has significant individual, societal, economic, political, healthcare delivery and policy implications, making it challenging to construct a unifying definition of disability (5-8).
The medical model of disability considers a person to have a disability based on a disease or health condition that limits their ability to carry out expected individual and societal obligations (5-8). This is accompanied by a range of disability based on severity within the context of the many conditions that can affect an individual’s functioning. The medical model attributes functional limitations associated with disability to the person, which implies that if their condition is cured, then the disability could be remediated (5-8). There is minimal consideration of contribution of the environmental or societal factors in the medical model, which generally views the person with a disability in a sick role (5-8).
The social model, on the other hand, takes into consideration the role of the environmental and societal factors in its construct of disability (5-8). Disability within the context of social model is considered based on the understanding that by itself, functional impairment at an individual level by itself may or may not result in disability; rather, sociocultural expectations and built environment together limit a person’s ability to engage in expected individual and societal obligations (5-8).
It is important to understand the frequently used terms impairment, handicap, and disability (Table 1) (4-8). The World Health Organization (WHO) has developed the International Classification of Functioning, Disability and Health, which comprises three key components: (I) body function and structure; (II) activity; and (III) participation (Table 2) (9-12). The general WHO classification provides a framework for delineating specific disabilities. The three key components of the WHO classification are interrelated and may interact with a given health condition and individual and environmental factors.

Full table

Full table
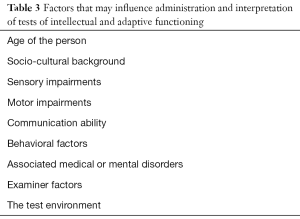
Definition
The term intellectual disability or intellectual developmental disorder is used to describe significantly sub-average intellectual and adaptive functioning based on clinical assessment and as measured by individually administered, appropriately normed, standardized and validated tests of intellectual functioning and adaptive behavior, with onset during the developmental period from infancy through adolescence (10,13-15). According to the WHO classification, “Disorders of intellectual development are a group of etiologically diverse conditions originating during the developmental period characterized by significantly below average intellectual functioning and adaptive behavior that are approximately two or more standard deviations below the mean (approximately less than the 2nd/3rd percentile) (10).” A diagnosis of intellectual disability should not be based solely on the results of tests of intellectual and adaptive functioning; rather, it is based on a combination of clinical assessment and judgment in conjunction with the results of standardized tests of intellectual and adaptive functioning (1,8,10,13,15). The assessment of intellectual functioning and adaptive behavior may be influenced by a number of factors (Table 3) that should be considered in the administration of the tests and interpretation of their results (8,10,13,15,16).
Full table
According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), the deficits in intellectual function include reasoning, problem solving, planning, abstract thinking, judgment, academic learning, and learning from experience (15). The critical components of intellectual functioning included in the DSM-V criteria are verbal comprehension, working memory, perceptual reasoning, quantitative reasoning, abstract thought, and cognitive efficacy (15).
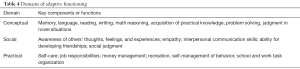
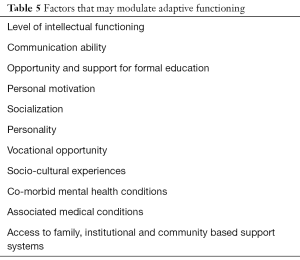
Widely accepted definition and classification systems for intellectual disability consider adaptive functioning in terms of conceptual, social, and practical domains (8-10,13-15) (Table 4). Deficits in adaptive functioning result in failure to meet developmental and sociocultural standards for personal independence and social responsibility. A number of factors (Table 5) may either facilitate or hinder adaptive functioning in one or more activities of daily life, such as communications, social participation, and independent living, across multiple environments such as home, school, work, and community (4,7,8,13,15).
Full table
Full table
Epidemiology
The reported prevalence of intellectual disability is 1% globally and vary from 1% to 3% by country, with a male to female ratio of 2:1 (8,12,13,15-27). Although the prevalence of mild intellectual disability has declined somewhat in recent years, the prevalence of severe intellectual disability has remained same during that time at approximately 0.3–0.5% of population (12,13,16,27). Statistically, the prevalence of intellectual disability in the general population is expected to be 2.5% (13,15). This is based on the understanding that intelligence [measured as intelligence quotient (IQ), by individually administered standardized tests of intelligence] has a typical distribution in the population and applying 2 standard deviations below the mean as a cutoff point (13,15). When one child is diagnosed having severe intellectual disability, the recurrence risk for intellectual disability in subsequent child is estimated to range from 3% to 9% (13,15,16).
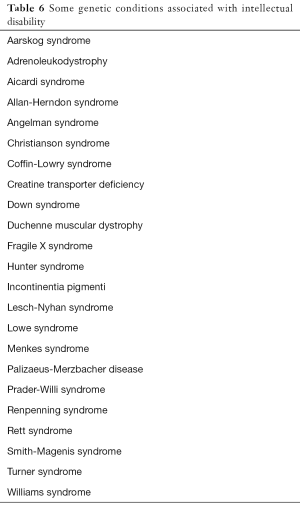
Measured IQ is considered an approximation of intellectual functioning, which may or may not necessarily correlate with the level of adaptive functioning (1,8,13,15,16). However, based on a number of epidemiological studies, persons with an IQ score of 50 or less are considered to have severe intellectual disability; whereas, persons with an IQ above 50 are considered to have mild intellectual disability (13-16). Almost all persons with a measured IQ of ≤50 manifest some degree of adaptive deficits (13-16). Major risk factors for mild intellectual disability are environmental and psychosocial, and include low socioeconomic status, residence in low-income countries, low maternal education, malnutrition, and inadequate access to healthcare (8,11-16,28). On the other hand, in persons with severe intellectual disability, a specific underlying genetic, biological or neurological can be identified in more than 75% of cases (8,11-13,28). The most common identified conditions in persons with severe intellectual disability include chromosomal abnormalities, genetic syndromes (Table 6), congenital brain malformations, neurodegenerative diseases, congenital central nervous system infections, inborn errors of metabolism (Table 7), maternal disease during pregnancy, in utero exposure to toxins, and birth injury (13,15,16,27-30).
Full table
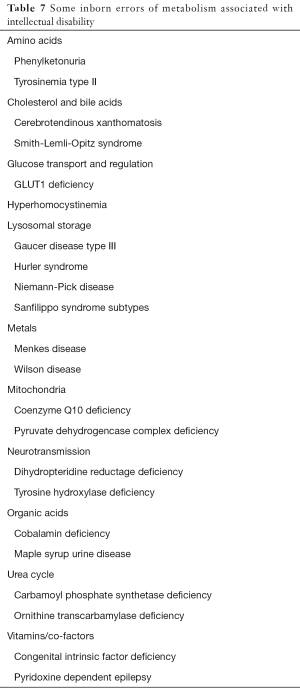
Full table
Clinical features
The clinical symptoms and signs of intellectual disability are generally first recognized during infancy and childhood. The predominant clinical symptoms and signs suggestive of intellectual disability vary depending up on the age at presentation, specific cause and the severity of cognitive deficit (1,4,8,13,15,16). Infants and young children with severe intellectual deficit are highly likely to have an underlying cause and present early with clinical features associated with the underlying condition (13,16,28,30). On the other hand, a large percentage of children with mild range of intellectual deficits are highly unlikely to have an identifiable underlying specific cause or clinical findings, and may not be recognized to have intellectual disability until later in childhood (13,16,28,30). Some children with mild ID may not be recognized until 5–9 years of age (16). Abnormal findings on physical examination such as macrocephaly or microcephaly, dysmorphic features, multiple congenital anomalies, or difficulty with feeding in a newborn should prompt consideration of associated intellectual disability (8,13,16). Gross motor delay is a common presentation ID during infancy; whereas, during pre-school and early school years language, learning and academic difficulty as well as behavioral concerns is common presentation in children with ID (16).
Mild intellectual disability
Eighty-five percent of persons with intellectual disability have mild severity and are less likely to be recognized to have ID before 5–6 years of age (8,13,16). Mild intellectual disability is characterized by measured intellectual and adaptive functioning that is approximately two to three standard deviations below the mean (approximately 0.1–2.3 percentile) (10). The measured IQ for persons with mild ID is between 50–55 and 70 (based on population mean of 100; 1 standard deviation of 15, and margin of measurement error of ±5) (8,10,13-16). Persons with mild ID have difficulty in the acquisition and comprehension of complex language and academic skills (10,13,15,16). They can reach academic skills equivalent to 4th–5th grade level (10,16). In addition to language difficulty, persons with mild ID also have difficulty in arithmetic and writing skills (10,15,16). With appropriate support, they are able to develop basic skills in reading, writing and mathematics. Most are able to write simple letters and complete a simple job application (10,15,16).
Adolescents and adults with mild ID continue to show deficits and limitations in executive functioning such as planning, organizing, priority setting and abstract thinking (15). They also show limitations in tasks that require short-term recall. Persons with mild ID are at an increased risk for being manipulated by others (15). They show limited ability to accurately judge or comprehend the norms of social discourse and interactions, and, often, their behavior in social situations may be considered immature or inappropriate by others (15).
With appropriate support, persons with mild intellectual disability are able to acquire most skills needed for daily household, practical and self-care activities (10,13,15). Persons with mild intellectual disability can be sufficiently skilled as adults to be gainfully employed and able to maintain independence in daily life activities (10,13,15). They can learn simple employment related skills such as report to work at expected time, stay at task, and engage in appropriate social interactions with coworkers (10,13,15). They can also learn to drive and use public transportation. Overall, most persons with mild ID function at mental age of 9–11 years as adults (10,13,15). Persons with mild ID need intermittent support in daily living activities such as self-care, shopping, food preparation and money management (10). They need assistance in making healthcare and legal decisions. Persons with mild ID can acquire basic vocational skills as adults, and may be employed in jobs that do not require application of academic or conceptual skills (10,13,15,16).
Moderate intellectual disability
About 10% of persons with ID have moderate severity and likely to be recognized to have an ID by 3–5 years of age (8,13,16). A moderate ID is characterized by intellectual and adaptive functioning that are approximately three to four standard deviations below the mean (approximately 0.003–0.1 percentile) (10). The measured IQ of persons with moderate ID falls between 35–49 and 50–55 (8,10,13-16).
The rate of acquisition of basic language skills is slow in children with moderate ID (8,10,16). The acquisition and development of language as well as the ability to learn and attain proficiency in academic skills are limited in persons with moderate intellectual disability person (10,15). Persons with moderate ID show significant limitations in reading, writing, mathematics and other skills requiring understanding basic concepts (10,13,15). Persons with moderate ID may develop some basic skills, for example, ability for sight-word reading, copy information, and match number to number of items (10,13,15). They can acquire academic skills equivalent to early elementary school grade level (10,15). Persons with moderate ID experience difficulty in social communication, interpersonal interactions and understanding behavioral norms expected for age and social context (15). With ongoing support, persons with moderate ID can develop meaningful family and personal relationships. They have limitations in social decision-making and social judgment (15). Development of maladaptive behaviors is a significant concern in persons with moderate ID and this can further contribute to difficulty in social interactions and relationships (15).
Persons with moderate ID function at mental age of about 6-8 years as adults (8,10,13,15,16). Persons with moderate intellectual disability need substantial ongoing support as adults to maintain independence in daily living activities and to remain gainfully employed (13). With ongoing support and teaching, persons with moderate ID may be able to acquire basic daily living and job skills. They need continued supervision and guidance in daily activities as well as performing job related tasks. A person with moderate ID can attain relative independence in self-care and daily living tasks such as eating, dressing, elimination and personal hygiene (10,13,15).
Severe intellectual disability
About 4% of persons with ID have severe ID, and are highly likely to be recognized as having severe ID by 3 years of age or earlier (8,13,16). Severe ID is characterized by intellectual and adaptive functioning that are approximately four or more standard deviations below the mean (less than approximately the 0.003rd percentile) (10). The measured IQ of persons with severe ID falls between 20–25 and 35–40 (10,13,15). In addition to severe deficit in intellectual functioning, persons with severe ID may also have motor impairments and other associated conditions that further limit intellectual and adaptive functioning (8,15). Persons with severe ID function at mental age between 3 and 5 years as adults (8,10,15,16). Persons with severe ID need extensive, regular, consistent, and lifetime support in daily living activities, and are care dependent (13,15).
Persons with severe ID have significantly limited language and communication ability. They have significant limitations in spoken language; communication may be limited to use of single words or phrases (10,15). Their communication ability may be improved with use of augmentative communication methods. They often use gestures to communicate basic needs. Persons with severe ID have significant limitations in understanding concepts of numbers, quantity, time, management of money and problem solving (10,13,15,16). The social interactions and relationships for persons with severe ID are largely limited to immediate family members and care takers.
A person with severe ID requires intensive support in all activities of daily living including self-care and personal hygiene (10,15). They are not able to make sound judgments or decisions that may affect the wellbeing of self or others and require constant supervision (15). Maladaptive behavior, including self-harm, is a significant concern in persons with severe ID (15).
Profound intellectual disability
Approximately 1% of persons with ID have profound ID and recognized by 2 years of age (8,13,15,16). A profound ID is characterized by intellectual and adaptive functioning that are approximately four of more standard deviations below the mean (approximately less than the 0.003rd percentile) (10). Persons with profound ID have IQ less than 20–25 (8,13,15,16). Persons with profound ID function at about 3 years of mental age and need high intensity, pervasive support across all environments (8,10,15,16). They have significant limitations in self-care, continence, communication and mobility. They may need complete custodial or nursing care and are total care dependent (13,15). Severe ID is also associated with other impairments such as motor and sensory disorders that further limit acquisition and use of motor, adaptive or social skills. Severe and profound ID are differentiated primarily based on differences in limitations of adaptive behavior because the validity and reliability of standardized tests of intelligence are not clearly established when used in persons with intellectual functioning that is below the 0.003rd percentile person (10).
Persons with profound ID have substantial deficits in academic or conceptual skills. With intensive and persistent teaching and assistance, it is possible for a person with profound ID who do not have associated motor or sensory impairments, to develop some capacity for self-care (13,15). Some may be able to develop some capacity for nonverbal communication with use of augmentative communication methods. A person with profound ID may respond to familiar persons or caretakers with gestures and facial emotional cues (15). A person with profound ID needs constant supervision and is total care dependent in all aspects of daily living.
Undetermined severity
The standardized tests for assessment of intellectual and adaptive functioning are generally difficult to administer in very young children and the results may not be reliable or valid (10,15). This may also be the case in older children with associated other conditions that may pose barriers to effective testing, such as motor or sensory impairments and co-morbid medical or mental health disorders. When intellectual or adaptive functioning cannot be reliably assessed, based on standardized tests, a diagnosis of intellectual disability and its severity is made based on findings of clinical evaluation (8,10,15,16).
Etiological testing
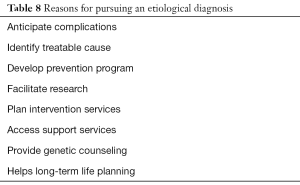
The value of identifying a specific cause of intellectual disability, especially in case of mild intellectual disability, is subject to debate (30-33) (Table 8). Because a biologic cause is more likely to be identified in severe intellectual disability, an etiological diagnosis should be pursued in all such cases. In many cases, certain disease specific clinical findings may indicate additional tests to identify a cause.
Full table
The initial diagnosis of intellectual disability is considered mainly based on clinical presentation. Key components of diagnostic evaluation are a complete medical history (Table 9), general physical examination, dysmorphology examination and neurological examination (2,13,28,30,32). A diagnosis of intellectual disability requires an assessment of the person’s cognitive and adaptive abilities using individually administered standardized instruments by qualified professionals. Standardized test of intellectual and adaptive functioning should be appropriate for the population being tested. Standardized testing should be age appropriate, take into account the mental age of the child, be culturally sensitive, and accommodate for any motor, behavioral, or language variations (1,13,15,16). Hearing and vision should be assessed in all children as part of their intellectual disability evaluation (16,30).
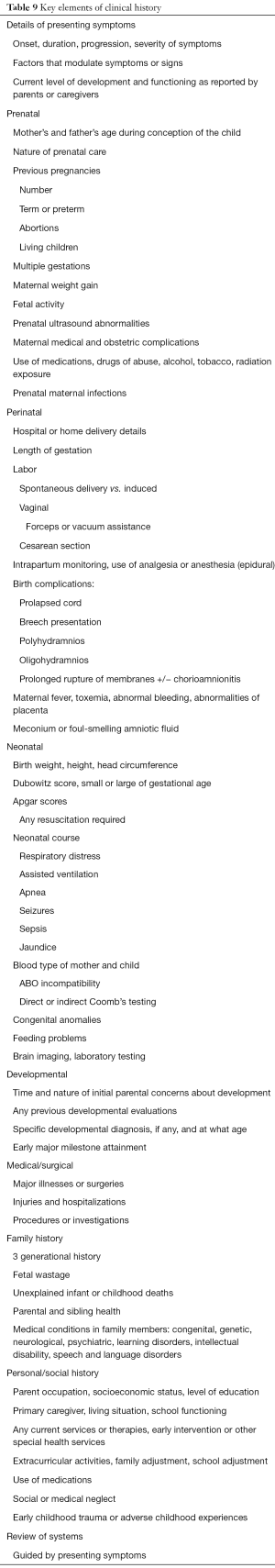
Full table
Many conditions associated with severe to profound intellectual disability can be suspected based on their characteristic clinical features. On the other hand, in a large percentage of cases, especially in mild intellectual disability, no clinical characteristics suggestive of a specific condition are found. Laboratory tests for genetic disorders or abnormalities, laboratory tests for inborn errors of metabolism and neuroimaging studies are the main evaluation tools used to confirm or identify any specific etiology of intellectual disability. Such an extensive evaluation should be considered in consultation with appropriate professionals with expertise and experience in specific disciplines (8,16,30-37). The likelihood of identifying the etiology of intellectual disability by various laboratory tests and neuroimaging studies vary based on the severity of intellectual disability and the presence or absence of abnormal findings on clinical evaluation (1,16,29-34).
Newborn screening programs, where available and instituted, identify a number of inborn errors of metabolism. Early identification of treatable inborn errors of metabolism is important to improve long-term outcomes (34,35). Beyond the newborn period, in the absence of large scale implementation of newborn screening for inborn errors of metabolism, an evaluation for metabolic disorder is considered based on findings on clinical evaluation. Some of the finding that may suggest an inborn error of metabolism include a family history of IEM or unexplained neonatal death, consanguinity, failure to thrive, recurrent vomiting, seizures, lethargy, developmental regression, abnormal movements, hypotonia, facial dysmorphism, and enlarged spleen or liver (30,31,34,35). Specific tests of inborn errors of metabolism (Table 10) should be considered in consultation with metabolic geneticist (30,31,34,35).
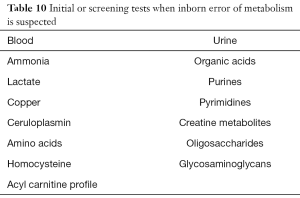
Full table
If a specific genetic diagnosis is suspected, work-up with appropriate genetic tests is considered in consultation with a geneticist. A chromosomal microarray test is recommended as a standard initial test in the evaluation of intellectual disability (30). If chromosomal microarray testing is not diagnostic, additional testing with exome or whole genome tests may be indicated (29-31,37,38). Fragile X testing should be included in all work-up as it is one of the most common genetic causes of intellectual disability (30). In females with moderate to severe intellectual disability, testing for Rett syndrome (methyl CpG-binding protein 2) is recommended (30,31). The overall yield of microarray analysis in the evaluation of intellectual disability is estimated to be 15%; whole exome sequencing is reported to add additional 30% and whole genome sequencing an additional 15% to overall yield (16,30-32).
Brain magnetic resonance imaging (MRI) scan is indicated in the presence of abnormal neurological history and examination findings. With abnormal neurological findings, 30–40% of MRI scans show abnormalities (16,30,32). In the absence of specific abnormal neurological findings, about 10% of scans show abnormal findings (16,30,32). However, in most cases it is difficulty to establish the significance of abnormal findings on neuroimaging as a cause of intellectual disability.
General comments on management
Improved prenatal care, improved access to maternal-child health, newborn screening for inborn errors of metabolism, and improved immunization rates, contribute to reduced rates of intellectual disability (16,27,28). The underlying cause, clinical manifestations, and cognitive and adaptive abilities vary widely between persons with intellectual disability. Such heterogeneity requires individualized considerations for treatment depending on individual needs; it is not within the scope of this review to describe in detail comprehensive management of all primary and associated conditions in persons who have intellectual disability. Notwithstanding the heterogeneity and need for individualized considerations, certain general principles of treatment for persons with ID provide a framework for their overall healthcare, which include the following (1,16,38-54):
- Treatment of medical complications;
- General preventive medical care;
- Treatment of co-morbid medical and mental health conditions;
- Treatment of challenging behaviors;
- Rehabilitation services;
- Educational support;
- Vocational training;
- Social support;
- Support for community based living;
- Support for appropriate level of employment;
- Transition to services from children focused to those more appropriate for adults;
- Guardianship, financial and legal considerations.
The optimum model of care for persons who have intellectual disability is an interdisciplinary care model in the setting of a clinical service or medical center. Primary care medical practitioner provides preventive and general medical care as well as facilitates and coordinates specialty consultative care and access to needed support services.
Like most countries in the world, in the United States, several federal and state laws, regulations and acts provide the regulatory basis for the development, implementation and funding of various services for persons with developmental disabilities (55). Most intervention and service programs are developed and implemented within or linked to formal educational systems at local or community level. Programs are structured to meet the age appropriate differences in the needs of children, adolescents and adults with intellectual disability. For young children under 3 years of age, early intervention services provided by local community agencies are used and the Individualized Family Service Plan is implemented for these families. For children and adolescents between 3 and 16 years of age an Individualized Education Plan is developed to provide appropriate educational interventions in the least restrictive environment possible along with related support services. Between 14 and 16 years of age, plan for transition of services to adult oriented settings is considered. The Individualized Transition Plan includes consideration of adult oriented services, vocational training, and needs for independent living. When the adolescent graduates from formal educational system as a young adult, continued support services are provided based on the development and implementation of an Individualized Habilitation Plan. The scope and intensity of interventions and support services vary depending upon the needs of the person and the severity of the intellectual disability.
Conclusions
Significant limitations in both intellectual and adaptive functioning with onset during developmental period are the core features of intellectual disability. The level of adaptive functioning and the intensity of supports needed are the main criteria used to categorize intellectual disability levels of severity. The level and limitations of both the intellectual and adaptive functioning of a person are based on a comprehensive clinical evaluation as well as individually administered standardized tests of intellectual and adaptive functioning. The use of measured IQ in determining severity of intellectual disability has limitations, especially at higher levels of IQ and therefore IQ alone is not considered sufficient criteria to determine whether a person should be considered to have an intellectual disability nor to determine its severity. Psychosocial and environmental factors are the main contributors of mild intellectual disability, which comprises 85% of persons who have intellectual disability. The clinical symptoms and signs of intellectual disability depend on the age at initial presentation and the severity of the deficits; the more severe the deficits, earlier the age at presentation. An evaluation for an underlying specific cause for intellectual disability is recommended and such work-up includes genetic testing, metabolic testing and neuroimaging. The main strategies for management of persons who have intellectual disability are general medical care, treatment of comorbid conditions, treatment of behavioral symptoms, special education, vocational training, and community-based supports. In most countries, there are specific laws and acts that protect the rights of persons with disabilities as well as provide a framework and variable level of funding for their care.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest:DRP serves as the unpaid Deputy Editor-in-Chief of TP and the unpaid Guest Editor of the focused issue “Neurodevelopmental and Neurobehavioral Disorders in Children”. TP. Vol 9, Supplement 1 (February 2020). The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Patel DR, Apple R, Kanungo S, et al. Intellectual disability: definitions, evaluation and principles of treatment. Pediatric Medicine 2018;1:11. [Crossref]
- Patel DR, Greydanus DE, Merrick J, et al. Introduction to intellectual and developmental disabilities. In: Rubin IL, Merrick J, Greydanus DE, et al. editors. Health Care for People with Intellectual and Developmental Disabilities across the Lifespan. Cham: Springer, 2016:5-12.
- Patel DR, Merrick J. Neurodevelopmental disabilities: introduction and epidemiology. In: Patel DR, Greydanus DE, Omar HA, et al. editors. Neurodevelopmental Disabilities, New York: Springer, 2011:1-13.
- Patel DR, Greydanus DE, Calles JL Jr, et al. Developmental disabilities across the lifespan. Disease-a-Month 2010;56:304-97. [Crossref] [PubMed]
- Patel DR, Brown KA. An overview of the conceptual framework and definitions of disability. Int J Child Health Hum Dev 2017;10:247-52.
- Smart JF, Smart DW. Models of disability: implications for the counseling profession. J Couns Dev 2006;84:29-40. [Crossref]
- Mitra S. The capability approach and disability. J Disabil Policy Stud 2006;16:236-47. [Crossref]
- Harris JC. Intellectual Disability: Understanding its Development, Causes, Classification, Evaluation, and Treatment. Oxford: Oxford University Press, 2006.
- World Health Organisation Classification of Functioning Disability and Health. Available online: http://apps.who.int/classifications/icfbrowser/. Accessed January 21, 2020.
- World Health Organisation. Disorders of intellectual development. Available online: https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f605267007. Accessed January 21, 2020.
- World Health Organization. Better health, better lives: children and young people with intellectual disabilities and their families. Copenhagen: Denmark, WHO Regional Office for Europe, 2010. Available online: http://www.euro.who.int/__data/assets/pdf_file/0003/125751/e94414.pdf. 1/21/2010
- World Health Organization Atlas: Global Resources for Persons with Intellectual Disabilities. 2007 WHO pp 1-108. Available online: https://apps.who.int/iris/bitstream/handle/10665/96353/9789241563505_eng.pdf;jsessionid=30C096378016EAEE4DB7324DC8044A63?sequence=1. Accessed 1/21/2020.
- Schalock RL, Borthwick-Duffy SA, Buntinx WHE, et al. editors. Intellectual disability: Definition, classification, and systems of supports. Washington, DC: American Association for Intellectual and Developmental Disabilities, 11th edition, 2009.
- Schalock RL, Luckasson R. A systematic approach to subgroup classification intellectual disability. Intellect Dev Disabil 2015;53:358-66. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edition. Washington DC: American Psychiatric Press, 2013:31-86.
- Shapiro BK, O’Neill ME. Developmental delay and intellectual disability. In: Kliegman RM, St Geme III JW, Blum NJ, et al. editors. Nelson Textbook of Pediatrics. 21st edition. Philadelphia, PA: Elsevier, 2020:283-93.
- Zheng X, Chen G, Song X, et al. Twenty-year trends in the prevalence of disability in China. Bulletin of the World Health Organization 2011;89:788-97. [Crossref] [PubMed]
- Kwok HW, Cui Y, Li J. Perspectives of intellectual disability in the People's Republic of China: epidemiology, policy, services for children and adults. Curr Opin Psychiatry 2011;24:408-12. [Crossref] [PubMed]
- Lin LP, Lin JD. Perspectives on intellectual disability in Taiwan: epidemiology, policy and services for children and adults. Curr Opin Psychiatry 2011;24:413-8. [Crossref] [PubMed]
- Anagnostopoulos DC, Soumaki E. Perspectives of intellectual disability in Greece: epidemiology, policy, services for children and adults. Curr Opin Psychiatry 2011;24:425-30. [Crossref] [PubMed]
- Ispanovic-Radojkovic V, Stancheva-Popkostadinova V. Perspectives of intellectual disability in Serbia and Bulgaria: epidemiology, policy and services for children and adults. Curr Opin Psychiatry 2011;24:419-24. [Crossref] [PubMed]
- Jeevanandam L. Perspectives of intellectual disability in Asia: epidemiology, policy, and services for children and adults. Curr Opin Psychiatry 2009;22:462-8. [Crossref] [PubMed]
- Mercadante MT, Evans-Lacko S, Paula CS. Perspectives of intellectual disability in Latin American countries: epidemiology, policy, and services for children and adults. Curr Opin Psychiatry 2009;22:469-74. [Crossref] [PubMed]
- Sonnander K, Claesson M. Classification, prevalence, prevention and rehabilitation of intellectual disability: an overview of research in the People's Republic of China. J Intellect Disabil Res 1997;41:180-92. [Crossref] [PubMed]
- Njenga F. Perspectives of intellectual disability in Africa: epidemiology and policy services for children and adults. Curr Opin Psychiatry 2009;22:457-61. [Crossref] [PubMed]
- Girimaji SC, Srinath S. Perspectives of intellectual disability in India: epidemiology, policy, services for children and adults. Curr Opin Psychiatry 2010;23:441-6. [Crossref] [PubMed]
- Maulik PK, Mascarenhas MN, Mathers CD, et al. Prevalence of intellectual disability: a meta-analysis of population-based studies. Research in Developmental Disabilities 2011;32:419-36. [Crossref] [PubMed]
- Huang J, Zhu T, Qu Y, et al. Prenatal, perinatal and neonatal risk factors for intellectual disability: a systemic review and meta-analysis. PLoS One 2016;11:e0153655. [Crossref] [PubMed]
- Chiurazzi P, Pirozzi F. Advances in understanding – genetic basis of intellectual disability. F1000Research 2016;5:599. [Crossref] [PubMed]
- Moeschler JB, Shevell M. Comprehensive evaluation of the child with intellectual disability or global developmental delays. Pediatrics 2014;134:e903-18. [Crossref] [PubMed]
- Michelson DJ, Shevell MI, Sherr EH, et al. Evidence report. Genetic and metabolic testing on children with global developmental delay: report of the Quality Standards Subcommittee of the American Academy of Neurology and Practice Committee of Child Neurology. Neurology 2011;77:1629-35. [Crossref] [PubMed]
- Shevell M, Ashwal S, Donley D, et al. Practice parameter: evaluation of the child with global developmental delay. Neurology 2003;60:367-80. [Crossref] [PubMed]
- VanKarnebeck CDH, Janswiejer MCE, Leenders AGE, et al. Diagnostic investigation in individuals with mental retardation: A systematic literature review of their usefulness. Eur J Human Genet 2005;13:6-25. [Crossref]
- van Karnebeek CD, Stockler-Ipsiroglu S. Treatable inborn errors of metabolism causing intellectual disability: A systematic literature review. Molecular Genetics and Metabolism 2012;105:368-81. [Crossref] [PubMed]
- van Karnebeek CD, Stockler-Ipsiroglu S. Early identification of treatable inborn errors of metabolism in children with intellectual disability: the Treatable Disability Endeavor protocol in British Columbia. Paediatr Child Health 2014;19:469-71. [Crossref] [PubMed]
- Vissers LELM, Glissen C, Veltman JA. Genetic studies in intellectual disability and related disorders. Nature Reviews 2016;17:9-18. [Crossref] [PubMed]
- Bowling KM, Thompson ML, Amaral MD, et al. Genomic diagnosis for children with intellectual disability and/ or developmental delay. Genome Medicine 2017;9:43. [Crossref] [PubMed]
- McCarthy J, O'Hara J. Ill-health and intellectual disabilities. Curr Opin Psychiatry 2011;24:382-6. [Crossref] [PubMed]
- Evenhuis H, Henderson CM, Beange H, et al. Healthy Ageing - Adults with Intellectual Disabilities: Physical Health Issues. Geneva, Switzerland: World Health Organization, 2000.
- Matson JL, Shoemaker ME. Psychopathology and intellectual disability. Curr Opin Psychiatry 2011;24:367-71. [Crossref] [PubMed]
- McGuire BE, Bayley AA. Relationships, sexuality and decision-making capacity in people with an intellectual disability. Curr Opin Psychiatry 2011;24:398-402. [Crossref] [PubMed]
- Torr J, Davis R. Ageing and mental health problems in people with intellectual disability. Curr Opin Psychiatry 2007;20:467-71. [Crossref] [PubMed]
- Walsh PN. Health indicators and intellectual disability. Curr Opin Psychiatry 2008;21:474-8. [Crossref] [PubMed]
- Chaplin R. Mental health services for people with intellectual disabilities. Curr Opin Psychiatry 2011;24:372-6. [Crossref] [PubMed]
- Evans E, Howlett S, Kremser T, et al. Service development for intellectual disability mental health: a human rights approach. J Intellect Disabil Res 2012;56:1098-109. [Crossref] [PubMed]
- Salvador-Carulla L, Symonds S. Health services use and costs in people with intellectual disability: building a context knowledge base for evidence-informed policy. Curr Opin Psychiatry 2016;29:89-94. [Crossref] [PubMed]
- Muñoz-Solomando A, Townley M, Williams R. Improving transitions for young people who move from child and adolescent mental health services to mental health services for adults: lessons from research and young people's and practitioners' experiences. Curr Opin Psychiatry 2010;23:311-7. [Crossref] [PubMed]
- Balogh R, McMorris CA, Lunsky Y, et al. Organising healthcare services for persons with an intellectual disability. Cochrane Database Syst Rev 2016;4:CD007492. [PubMed]
- Robertson J, Emerson E, Hatton C, et al. Efficacy of community-based rehabilitation for children with or at significant risk of intellectual disabilities in low and middle income countries: a review. J Appl Res Intellect Disabil 2012;25:143-54. [Crossref] [PubMed]
- Kliever C, Biklen D, Peterson AJ. At the end of intellectual disability. Harvard Educational Review 2015;85:1-28. [Crossref]
- Werner S, Yalon-Chamovitz S, Tenne Rinde M, et al. Principles of effective communication with patients who have intellectual disability among primary care physicians. Patient Education and Counseling 2017;100:1314-21. [Crossref] [PubMed]
- Munir KM. The co-occurrence of mental disorder in children and adolescents with intellectual disability/intellectual developmental disorder. Curr Opin Psychiatry 2016;29:95-102. [Crossref] [PubMed]
- Scott HM, Havercamp SM. Systematic review of health promotion program focused on behavioral change for people with intellectual disability. Intellect Dev Disabil 2016;54:63-76. [Crossref] [PubMed]
- Ploter AJ, Marshall KJ. Postsecondary education program for students with an intellectual disability: facilitators and barriers to implementation. Int Dev Disabl 2015;53:58-69. [Crossref]
- Individuals with Disability Education Act. Available online: https://sites.ed.gov/idea/. 1/21/2020.


