
A questionnaire-based assessment of gastrointestinal symptoms in children with type 1 diabetes mellitus
Introduction
Children commonly report gastrointestinal (GI) symptoms (1,2). These GI symptoms can impact adversely on the quality of life of the child and family (3). Anecdotally, children with type 1 diabetes mellitus (T1DM) are reported to complain of GI symptoms more frequently than their healthy peers. Potential explanations for this could include factors such as higher rates of coeliac disease (CD) in T1DM (4), the physiological effects of T1DM (5) or that living with a chronic illness may lead to altered perception of and increased complaints of pain (6).
Two reports have assessed GI complaints in children with T1DM compared to healthy peers (7,8). One study evaluating symptoms in adolescents found a high prevalence of at least one symptom in cases (75%) and controls (77%); however, the intensity of symptoms was not ascertained (7). The other report examined the prevalence of symptoms in children, but its control group was limited to children of hospital staff (8). They found lower rates of symptoms (36.8% cases, 44.9% controls) with no statistical difference between the groups.
To date there are no published data about GI symptoms in New Zealand children with or without diabetes. Consequently, the current study aimed to establish the rate and intensity of GI symptoms in a local population of children with T1DM compared to a group of healthy children. We present the following article in accordance with the SURGE checklist (available at http://dx.doi.org/10.21037/tp-20-139).
Methods
Subjects
All children with T1DM aged 15 years and younger attending the diabetes clinic at Christchurch Hospital (the tertiary referral centre for the mid-South Island of New Zealand) were approached to participate in the study by the first author. Controls were healthy peers or siblings of the case, healthy siblings of children admitted to the paediatric wards at Christchurch Hospital and children of staff at the Paediatric Department at Christchurch Hospital. Children were excluded if their caregiver felt they were unable to communicate complaints. Children or their caregivers were not provided without any specific incentives.
Questionnaire
Caregivers completed a questionnaire regarding GI symptoms (available from authors on request). This 10-question tool was designed to establish the presence and intensity of common GI symptoms in the preceding 6 months. The questionnaire was adapted to suit a New Zealand audience from a questionnaire designed by Saps et al. (9) to study GI symptoms in a community group of school aged children. The caregiver was asked to include the child when completing the questionnaire.
Symptoms assessed were: abdominal pain, nausea, vomiting (either an episode or persistently), diarrhoea, (either an episode or persistently), constipation, bloating and reflux. “Persistently” was defined as more than once in 24 hours for vomiting and greater than a week for constipation and diarrhoea. Respondents were asked to choose an answer from a 5-point Likert scale (0: not at all, 1: a little, 2: somewhat, 3: a lot, 4: a whole lot). A symptom was recorded as “present” if the respondent had complained of or experienced the symptom on at least one day in the past 6 months. A response of “Severe” was created for each symptom if the response on the Likert scale was 3 or above. The presence of upper GI symptoms (nausea, bloating, vomiting or reflux) was recorded as “Upper GI” present/absent, as was the presence of “Lower GI” symptoms (constipation, diarrhoea, persistent constipation, or persistent diarrhoea). A composite GI symptom score for each individual was recorded by summing the Likert scale score for each question.
The questionnaire included questions about demographics, past medical history (PMH) of GI disorders, pre-existing medical conditions, and family history (FH). The result of glycosylated haemoglobin (HbA1c) testing within 3 months of completing the questionnaire was obtained from each case’s hospital records, to serve as a proxy measure of blood sugar control.
Statistical analysis
Results were analysed using Stata/IC 12.1 for Windows (Statacorp, Texas, USA). Data were presented as means or proportions as appropriate. Mean values were compared using two sample t-tests. Odds ratios (OR), Pearson’s χ2 or Fisher’s exact test were used to compare dichotomous responses. Regression analysis was performed to evaluate the impact of background factors on the results, logistic for discrete variables, linear for continuous. P<0.05 was considered statistically significant. 95% CI were reported where appropriate.
Ethical approval
Ethical approval was granted to the study by the Upper South A Regional Ethics Committee, Christchurch New Zealand (URA/10/07/051). Informed consent was attained from the guardian and children prior to entry into the study. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Results
Subjects and demographics
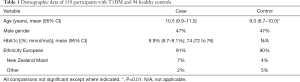
One hundred and fifty cases (88% of eligible population) and 94 controls (38% of distributed questionnaires returned) completed the questionnaire. Although cases were slightly older than controls [10.5 years (95% CI: 9.9–11.0) vs. 9.3 years (95% CI: 8.7–10), P=0.01], the two groups were similar for gender and ethnicity (Table 1). Approximately 30% of the controls were siblings of a case.
Full table
Overall GI symptom score
Eighty percent of controls and 85% of cases reported at least one GI symptom in the preceding 6 months [OR 1.5 (95% CI: 0.7–3.1), P=0.3]. Adjusting for age, sex, FH or PMH of GI condition did not impact on the result (Padj=0.3). Children with diabetes were more likely to have a higher mean GI symptom score than controls [4.9 (95% CI: 4.0–5.8) vs. 3.4 (95% CI: 2.6–4.2), P=0.02].
Specific GI symptoms
The most common symptom reported by children was abdominal pain. Most children (73% of cases and 66% of controls) reported at least “a little” abdominal pain in the preceding 6 months (OR 1.4, 95% CI: 0.8–2.5) (Table 2). For each question the mean response on the Likert scale was higher for cases, scores for abdominal pain 1.3 vs. 1.0 (P=0.02) and reflux 0.4 vs. 0.2 (P=0.01) were statistically significant (Table 2). Children with T1DM were more likely to complain of the presence of any reflux symptoms [OR 2.2 (95% CI: 1.1–4.6)].
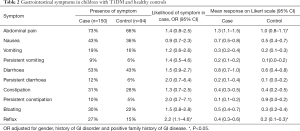
Full table
There was an increased proportion of complaints of “severe” abdominal pain in cases; 17% vs. 5% of controls [fisher’s exact P=0.01; OR 3.6 (95% CI: 1.3–12.3)]. Very few respondents answered 3 or above on the Likert scale for other symptoms; consequently, none of the other comparisons reached statistical significance (data not shown). When examined as symptom complexes, there was no difference in the prevalence of upper GI [61% cases vs. 49% controls, OR 1.6 (95% CI: 0.9–2.8)] or lower GI symptoms between cases and controls [56% vs. 62%, OR 1.3 (95% CI: 0.7–2.2)].
Pre-existing GI conditions
Pre-existing GI conditions included constipation, coeliac disease, and abdominal migraine (Table 3). Cases were more likely to have a pre-existing GI condition, OR 3.0 (95% CI: 1.2–8.4, P=0.01). No children had inflammatory GI condition such as inflammatory bowel disease or eosinophilic oesophagitis. In post hoc analysis when children with CD were excluded from analysis, cases had a mean score of 4.89 (95% CI: 4.00–5.77) vs. controls 3.40 (95% CI: 2.59–4.21), P=0.02.
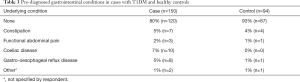
Full table
Other pre-existing medical conditions
The majority of children did not have any other medical problems (93% of cases and 90% of controls). Seven cases (5%) and nine controls (10%) listed a diagnosis of asthma, while three cases (2%) and one control (1%) listed attention deficit hyperactivity disorder as a pre-existing medical condition.
Factors predictive of gastrointestinal symptoms
The presence of T1DM was predictive of a higher GI symptom score (adjusted effect size 1.60, P=0.01). Higher HbA1c, PMH of GI disorder and female gender were predictive of a higher symptom score, whereas ethnicity and age were not. The increased likelihood of each symptom did not change when these factors were adjusted (Table 2). When the model was adjusted for gender, the relationship remained significant (Table 4).

Full table
Discussion
This study confirms that complaints of GI symptoms are common in childhood. Overall, 83% of the total group reported symptoms. The children with T1DM complained of gastrointestinal symptoms as frequently as their peers. However, the intensity of their complaints overall was more severe than their peers. In particular, they complained of more severe abdominal pain and reflux symptoms. Factors associated with a higher GI symptom score in cases included higher HbA1c and female gender.
The overall prevalence of GI symptoms in the current report was higher than reported in most studies, however no other studies have examined 6-month prevalence. A community-based study found weekly prevalence rates of 45% for any GI complaint (3). Most (90%) children complained of abdominal pain during the study period, with a weekly prevalence rate of 38%. Weekly rates for other symptoms (nausea 23%, diarrhoea 9%, constipation 8% and vomiting 7%) (3) were all lower than the 6-month prevalence reported by the current control group (10). In the general paediatric population abdominal pain prevalence rates have been reported at around 50%, again lower than the 73% of cases and 66% of controls in the present study (2,11).
Four children in the current study reported a pre-existing functional GI pain condition; this rate is much lower than the 12.5–25% previously published for pain predominant functional GI conditions (6,12,13). It is likely there are children in the current study with functional abdominal pain syndromes who have not had a formal diagnosis.
Although cases were more likely to have a pre-existing GI condition, the effect size was small (Table 4) and the inclusion of these conditions means the group is reflective of the true population attending clinic. No children had significant inflammatory gut conditions. Exclusion of children with CD did not affect the significance of the difference in mean score.
Two studies have investigated complaints of abdominal symptoms in children with T1DM. A Greek study investigated the prevalence of GI symptoms in a sample of children and adolescents attending a diabetes clinic and a well matched control group of siblings of hospitalized children and offspring of hospital staff (8). As in the current study, they found no difference between cases and controls (36.8% vs. 44.9% in controls; P=0.17). The overall prevalence rate of any GI symptom complaint was much lower than in the current study. Their results suggest that T1DM had no impact on symptom prevalence. However, they did not report the intensity of the symptoms or details of the specific symptoms.
A Swedish study used a postal questionnaire to determine the presence of 13 GI symptoms in a population-based group of adolescent cases and controls (7). Their findings are similar to the present study with a high prevalence of any GI symptom in cases and controls (75% vs. 77%; P=ns). They did not find any difference in prevalence for any of the individual symptoms, but subgroups were affected by environmental and disease specific factors, such as gender and HbA1c.
The current study has shown that children with T1DM complain of more intense symptoms than their peers. The reasons for this may include comorbidity, direct metabolic effects of hyperglycaemia or psychological factors.
Coeliac disease is more prevalent in T1DM (4). However, there is typically a low rate of reported symptoms in undiagnosed children (14,15). The standard local practice is to screen at least biannually, so the prevalence of undiagnosed CD can be assumed to be low and is unlikely to explain the difference in symptom score.
Autonomic neuropathy (AN) has been proposed as an explanation for more intense and frequent GI complaints in older patients (16-18). In children however, autonomic neuropathy is very rare at the onset of diabetes (19) and therefore unlikely to impact upon the rate of GI symptoms.
Perception of sensation from the GI system has been shown to change in both hyperglycaemia and hypoglycaemia (5,20,21). In the current study higher HbA1c was predictive of increased symptom score suggesting persistent hyperglycaemia may contribute to symptom prevalence. However, poor control has been associated (22,23), with symptoms of anxiety and depression, and it may be that higher HbA1c is a marker of psychological distress rather than the cause of the increased symptom complaints.
The complaints of pain in cases may be associated with the child’s reaction to and interpretation of pain. T1DM in children has been shown in a recent meta-analysis to be associated with small to moderate levels of psychological distress (22). Functional abdominal pain is often worse in children with psychological distress (6). There was no measure of psychological upset in the current questionnaire, but it is likely cases experience distress which may affect their interpretation of pain.
The way parents react to their child’s pain can alter the disability that results from that pain (24). In two large population studies of Health Related Quality of Life (HRQL) in children with T1DM (23,25); the children rated their HRQL higher than their parents rated the child’s HRQL. Parent and child were asked to answer the current questionnaire together, but as the completion of the questionnaires was not supervised, it is not possible to know how consistently this was done.
A limitation of the current study is the selection of control group children. All control children were recruited from the same geographical area. Siblings of children with T1DM are not necessarily a true representation of the normal population. The initial intention was to use peers, but recruitment was difficult. Using this group does however control for parenting practises and family history. The cases were older, but in the regression analysis this did not impact on the result. This study had an excellent response rate and it was representative of the diabetes clinic population, but the size of the study also means that the significance of subgroup analysis was limited. Although this questionnaire did have multiple questions, the likelihood of each response is not independent as the symptoms occur in complexes and therefore a Bon Ferroni correction would be too conservative. While the questionnaire has not been independently validated, and therefore results do need to be interpreted with caution, it has been adapted from an independently validated questionnaire.
Conclusions
In conclusion, gastrointestinal complaints were common in this group of children. The children with diabetes complained of more intense symptoms than their peers without diabetes. The reason for this difference in symptom severity may be related to the pathophysiology of T1DM or a psychological response to chronic illness. Further work examining the relationship of metabolic control and GI function as well as the psychological and family reaction to their illness may be useful to determine the reasons for this difference.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at http://dx.doi.org/10.21037/tp-20-139
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-20-139
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-20-139). ASD serves as an unpaid Deputy Editors-in-Chief of Translational Pediatrics from Aug 2020 to Jul 2022. JAP was in receipt of a Freemasons Fellowship in Paediatrics and Child Health. ASD reports personal fees from Abbvie, personal fees from Janssen, personal fees from Nestle, personal fees from Sanofi, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Upper South A Regional Ethics Committee, Christchurch New Zealand (URA/10/07/051). Informed consent was attained from the guardian and children prior to entry into the study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lavigne JV, Saps M, Bryant FB. Models of anxiety, depression, somatization, and coping as predictors of abdominal pain in a community sample of school-age children. J Pediatr Psychol 2014;39:9-22. [Crossref] [PubMed]
- Swain MS, Henschke N, Kamper SJ, et al. An international survey of pain in adolescents. BMC Public Health 2014;14:447. [Crossref] [PubMed]
- Saps M, Seshadri R, Sztainberg M, et al. A prospective school-based study of abdominal pain and other common somatic complaints in children. J Pediatr 2009;154:322-6. [Crossref] [PubMed]
- Porter JA, MacKenzie K, Darlow B, et al. Looking for coeliac disease in children with type 1 diabetes mellitus. J Paediatr Child Health 2014;50:811-6. [Crossref] [PubMed]
- Rayner CK, Jones KL, Ashley Blackshaw L, et al. The diabetic gut--both aching and unfeeling? Pain 2007;131:239-40. [Crossref] [PubMed]
- Devanarayana NM, Mettananda S, Liyanarachchi C, et al. Abdominal pain-predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J Pediatr Gastroenterol Nutr 2011;53:659-65. [Crossref] [PubMed]
- Lodefalk M, Aman J. Gastrointestinal symptoms in adolescents with type 1 diabetes. Pediatr Diabetes 2010;11:265-70. [Crossref] [PubMed]
- Vazeou A, Papadopoulou A, Booth IW, et al. Prevalence of gastrointestinal symptoms in children and adolescents with type 1 diabetes. Diabetes Care 2001;24:962-4. [Crossref] [PubMed]
- Saps M, Sztainberg M, Di Lorenzo C, et al. A prospective community-based study of gastroenterological symptoms in school-age children. J Pediatr Gastroenterol Nutr 2006;43:477-82. [Crossref] [PubMed]
- Saps M, Nichols-Vinueza DX, Mintjens S, et al. Construct validity of the pediatric Rome III criteria. J Pediatr Gastroenterol Nutr 2014;59:577-81. [Crossref] [PubMed]
- Huang RC, Palmer LJ, Forbes DA. Prevalence and pattern of childhood abdominal pain in an Australian general practice. J Paediatr Child Health 2000;36:349-53. [Crossref] [PubMed]
- Korterink J, Devanarayana NM, Rajindrajith S, et al. Childhood functional abdominal pain: mechanisms and management. Nat Rev Gastroenterol Hepatol 2015;12:159-71. [Crossref] [PubMed]
- Sagawa T, Okamura S, Kakizaki S, et al. Functional gastrointestinal disorders in adolescents and quality of school life. J Gastroenterol Hepatol 2013;28:285-90. [Crossref] [PubMed]
- Telega G, Bennet TR, Werlin S, et al. Emerging new clinical patterns in the presentation of celiac disease. Arch Pediatr Adolesc Med 2008;162:164-8. [Crossref] [PubMed]
- Simmons JH, Klingensmith GJ, McFann K, et al. Celiac autoimmunity in children with type 1 diabetes: a two-year follow-up. J Pediatr 2011;158:276-81.e1. [Crossref] [PubMed]
- Bharucha AE, Camilleri M, Forstrom LA, et al. Relationship between clinical features and gastric emptying disturbances in diabetes mellitus. Clin Endocrinol (Oxf) 2009;70:415-20. [Crossref] [PubMed]
- Mjörnheim AC, Finizia C, Blohme G, et al. Gastrointestinal symptoms in type 1 diabetic patients, as compared to a general population. A questionnaire-based study. Digestion 2003;68:102-8. [Crossref] [PubMed]
- Bytzer P, Talley NJ, Hammer J, et al. GI symptoms in diabetes mellitus are associated with both poor glycemic control and diabetic complications. Am J Gastroenterol 2002;97:604-11. [Crossref] [PubMed]
- Group TDR. The effect of intensive diabetes therapy on measures of autonomic nervous system function in the Diabetes Control and Complications Trial (DCCT). Diabetologia 1998;41:416-23. [Crossref] [PubMed]
- Schvarcz E, Palmer M, Aman J, et al. Physiological hyperglycemia slows gastric emptying in normal subjects and patients with insulin-dependent diabetes mellitus. Gastroenterology 1997;113:60-6. [Crossref] [PubMed]
- Schvarcz E, Palmer M, Aman J, et al. Hypoglycaemia increases the gastric emptying rate in patients with type 1 diabetes mellitus. Diabet Med 1993;10:660-3. [Crossref] [PubMed]
- Reynolds KA, Helgeson VS. Children with diabetes compared to peers: depressed? Distressed? A meta-analytic review. Ann Behav Med 2011;42:29-41. [Crossref] [PubMed]
- Frøisland DH, Graue M, Markestad T, et al. Health-related quality of life among Norwegian children and adolescents with type 1 diabetes on intensive insulin treatment: a population-based study. Acta Paediatrica 2013;102:889-95. [Crossref] [PubMed]
- Cunningham NR, Lynch-Jordan A, Barnett K, et al. Child pain catastrophizing mediates the relation between parent responses to pain and disability in youth with functional abdominal pain. J Pediatr Gastroenterol Nutr 2014;59:732-8. [Crossref] [PubMed]
- Kristensen LJ, Birkebaek NH, Mose AH, et al. Symptoms of emotional, behavioral, and social difficulties in the danish population of children and adolescents with type 1 diabetes--results of a national survey. PLoS One 2014;9:e97543. [Crossref] [PubMed]


