
Etiological distribution of pertussis-like syndrome in 756 children in Chengdu
Introduction
Pertussis-like syndrome is a syndrome highly similar to whooping cough. Infants with pertussis-like syndrome commonly present with paroxysmal, violent coughing, frequently resulting in reddening of the face and often followed by a high-pitched inspiratory ‘whoop’ sound. Infants may also display cyanotic lips and face or even suffer from seizures after excessive coughing. Compared with common pediatric pneumonia, pertussis-like syndrome may last as long as several months, with alternating periods of relapse and remission. The infants may need frequent hospital admissions, causing great distress and economic burden to the family. In recent years, the incidence of whooping cough has been rising. Notably, pertussis-like syndrome may be severe in infancy and can be life-threatening have reported that the common pathogens causing pertussis-like syndrome in children include respiratory syncytial virus (RSV), adenovirus, Bordetella parapertussis, and M. pneumoniae. The pathogens can be highly diversified. The clinical treatment regimen for pertussis-like syndrome in infants and young children varies at home and abroad. To our knowledge, there have been no reports on the local etiological and clinical features of pertussis-like syndrome in infants and young children in Chengdu or even the entire Sichuan Province. Here, a retrospective analysis was conducted on the etiology of pertussis-like syndrome in infants in Chengdu from 2015 to 2019. This study intended to analyze the etiological distribution of pertussis-like syndrome in infants and young children in Chengdu and provide clinical information to aid in the diagnosis and treatment of pertussis-like syndrome in this region, especially in regard to identifying the most effective treatments for this disease. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/tp-21-140).
Methods
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The Institutional Review Committee approved the retrospective analysis without providing written ethical approval, because it was an objective report complying to the condition of protecting the privacy of the patients. Individual consent for this retrospective analysis was waived.
Baseline data
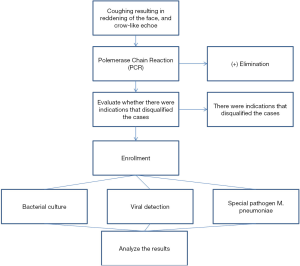
A retrospective analysis was performed of 756 children with confirmed pertussis-like syndrome hospitalized at the Department of Pediatric Respiratory Medicine of Chengdu Women’s and Children’s Central Hospital, from January 2015 to August 2019 (Figure 1). There were 437 male infants and 319 female infants, with an average age of 1.52±0.84 years. The number of seriously ill patients was 526. Pertussis-like syndrome occurred throughout all seasons of the year, although the majority of cases (n=493) occurred in the winter and spring seasons.
Inclusion and exclusion criteria
Inclusion criteria
Pertussis-like syndrome: Presenting with symptoms highly similar to whooping cough such as paroxysmal, violent coughing resulting in reddening of the face and a high-pitched inspiratory ‘whoop’ sound; a positive polymerase chain reaction (PCR) detection of Bordetella pertussis.
Criteria for severe illness: (I) frequent, paroxysmal coughing with cyanosis or decreased oxygen saturation, with a need for nasal cannula oxygenation; (II) paroxysmal, violent coughing with seizures following excessive coughing; (III) dramatic decrease in energy and appetite; (IV) combined with liver function impairment, myocardial damage, electrolyte disturbance, or damage to other systems.
Exclusion criteria
(I) Airway disorders, such as congenital bronchopulmonary dysplasia and bronchiolitis obliterans; (II) recurrent lower respiratory tract infections; (III) autoimmune disorders and congenital immunodeficiency; (IV) being affected by pertussis-like syndrome at the recovery stage of pneumonia (having contracted pneumonia in the past 4 weeks, especially M. pneumoniae pneumonia).
Detection of etiological agents
Sample collection and processing
Upon admission, a 0.5–1 mL deep sputum sample was collected from each infant by specialist staff and placed into a disposable, sterilized sputum collector. The samples were subject to bacterial culture. Meanwhile, 2 mL of venous blood was collected into an EDTA-containing tube. The samples were used to detect the following pathogens: respiratory viruses [Q fever rickettsiae, Chlamydia pneumoniae, influenza A virus, influenza B virus, parainfluenza virus (PIV), RSV, and Legionella pneumophila] and antibody titer to M. pneumoniae.
Bacterial culture
The sputum samples were inoculated to the culture plate and then incubated in a 5% CO2 incubator at 35 °C for 48–72 h. The BD Phoenix™ automated identification and susceptibility testing system (Becton,Dickinson and Company) was used to detect the bacteria in strict accordance with the instruction manual and standard operating procedures.
Detection of antibodies to respiratory viruses
Antibodies to respiratory viruses were detected by an indirect immunofluorescence assay.
Detection of antibody titer to M. pneumoniae
An agglutination assay was employed for the serologic test of the IgM antibody titer. An antibody titer above 1:40 indicated a positive result.
Statistical analysis
All statistical analyses were conducted using SPSS 16.0 software (Produced by IBM). The results were expressed as mean ± SD (measurement data) and percentages (count data). The etiological differences between the groups were analyzed by using the chi-square test. A P value <0.05 was considered statistically significant.
Results
Among the 756 children with pertussis-like syndrome, 439 cases were positive for etiological agents. The detection results are reported below.
Basic features of the population
In 756 cases (Table 1), 437 cases of male, female 319 cases, according to whether or not more than 1 year old, one year of age and below 489 cases, 267 cases aged 1, according to census register, children 279 cities, counties and rural 477 cases, 523 cases related vaccination is complete, not completed on schedule in 216 cases, 17 were unknown, on gestational age, 667 cases of full term, premature birth in 89 cases, 642 cases of normal birth weight and low birth weight in 113 cases of macrosomia in 1 case
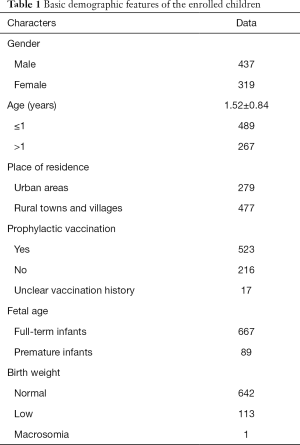
Full table
Results of bacterial detection
Among the 756 cases with pertussis-like syndrome (Table 2), 268 cases were positive for pathogenic bacteria (positive rate 35.45%), including 41 cases positive for Gram-positive bacteria (accounting for 15.29% of all cases positive for pathogenic bacteria) and 227 cases positive for Gram-negative bacteria (84.70%). Among the positive cases, there were 174 cases positive for H. influenzae (65.25%), 29 cases positive for Moraxella catarrhalis (10.82%), 24 cases positive for Streptococcus pneumoniae (S. pneumoniae) (8.95%), 3 cases positive for Escherichia coli (1.11%), 21 cases positive for Klebsiella pneumoniae (7.84%), 12 cases positive for Staphylococcus aureus (4.48%), and 5 cases positive for other rare bacteria (1.85%).
Full table
Results of viral detection
Among the 756 cases with pertussis-like syndrome, the total number of cases positive for antibodies for different types of viruses was 75 (positive rate 9.92%). There were 29 cases positive for RSV (accounting for 38.67% of all cases positive for viruses), 4 cases positive for influenza A virus (5.33%), 7 cases positive for influenza B virus (9.33%), 24 cases positive for PIV (32%), and 7 cases positive for adenovirus (9.33%).
Results of M. pneumoniae antibody titer detection
Among the 756 children with pertussis-like syndrome, 243 patients had an antibody titer to M. pneumoniae ≥1:80.
Distribution of mixed infections and infections caused by a single type of pathogen
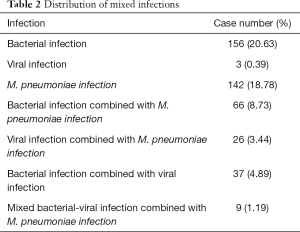
From the perspective of the etiology distribution of infection, bacterial infection, 156 cases (20.63%), and simplex virus infection 3 cases (0.39%), mycoplasma infection, 142 cases (18.78%), mixed bacteria and mycoplasma infection in 66 cases (8.73%), virus and mycoplasma infection in 26 cases (3.44%), bacterial and viral infections of 37 cases (4.89%), bacterial virus merger mycoplasma infection, 9 cases (1.19%).
Discussion
The incidence of pertussis-like syndrome has been dramatically rising in children in recent years. The typical symptoms of pertussis-like syndrome include paroxysmal, violent coughing resulting in reddening of the face, followed by a high-pitched inspiratory ‘whoop’ sound. Small infants may also display cyanosis of the face and lips or experience seizures following excessive coughing. The physiopathologic mechanism of paroxysmal coughing and whooping can be explained as follows: The pathogens entering the body adhere to the ciliated epithelial cells in the mucosa of the trachea, bronchi, and bronchioles, where they proliferate and release toxins. The ciliated columnar epithelial cells degenerate, and the ciliated epithelial cells are paralyzed due to the proliferating pathogens and the toxins released. Protein synthesis in the epithelial cells decreases and the subcellular organelles are damaged. As a result, sticky secretions caused by respiratory tract inflammation cannot be expelled. The retained secretions induce persistent stimuli to the terminal nerves of the respiratory tract, causing paroxysmal coughing via the central nervous system. A clinical study in baboon infants corroborated the above analysis (1). Histopathology of the trachea indicated massive inflammatory cell infiltration and mucus generation. Immunohistochemistry indicated that the bacteria were localized to the surface of the ciliated epithelium of the trachea, damaging the ciliated epithelium. Therefore, respiratory pathogen adhesion to the ciliated epithelium plays a vital role in whooping cough and pertussis-like syndrome. As to whether pertussis-like syndrome can be diagnosed based on clinical manifestations, Miyashita et al. (2) found that the diagnostic sensitivity of paroxysmal coughing in teenagers and adults was 90%. In comparison, the specificity was only 25%. The diagnostic sensitivity of reddening of the face with vomiting and inspiratory whooping following excessive coughing was only 25% and 19%, respectively. However, the specificity of these two symptoms was relatively high, being 80% and 86%, respectively. An elevation in the white blood cell count and lymphocyte count did not show good specificity. Therefore, reddening of the face with vomiting and inspiratory whooping’ following excessive coughing are preferred symptoms for confirming the diagnosis of pertussis-like syndrome in the clinical setting.
The existing etiological studies of pertussis-like syndrome at home and abroad have found that viruses are the primary pathogens causing pertussis-like syndrome in infants and young children. Besides, the etiological distribution displayed region-specific features. Mahmoudi et al. (3) found that RSV was the most frequently detected pathogen (20%), followed by adenovirus (16%), PIV (11%), and metapneumovirus (10%). Saiki-Macedo et al. (4) performed a retrospective analysis of the etiology of pertussis-like syndrome in 288 children under 5 years old. The most frequently isolated pathogen was adenovirus (49%), followed by M. pneumoniae (26%) and influenza B virus (19.8%). König et al. (5) detected etiological agents in 149 pediatric cases with pertussis-like syndrome who had coughed for over seven days. They found that adenovirus was the most common pathogen (22.1%), followed by HPV (12.1%), M. pneumoniae (10%), and RSV (9.4%). Ferrer et al. (6) showed that H. influenzae (16.9%) and S. pneumoniae (15.8%) were the primary pathogens of pertussis-like syndrome. The latest review of the etiology of pertussis-like syndrome pointed out that the influenza virus and PIV were also important pathogens causing pertussis-like syndrome in children (7).
So far, some retrospective analyses of the etiology of pertussis-like syndrome have been conducted in specific regions of China. An etiological study of pertussis-like syndrome in 263 children in Suzhou revealed that the top three pathogens were Streptococcus pneumoniae, rhinovirus, and M. pneumonia. An etiological survey in 491 children in Chongqing showed that bacteria were the most important pathogens of pertussis-like syndrome. Among all bacterial pathogens, H. influenzae was the most common. Among viral infections, RSV infection ranked first, followed by PIV III. Chlamydia trachomatis was mainly found in infants under three months old. Among mixed infections, mixed viral-bacterial infections had the highest detection rate. In Beijing, the most common pathogens of pertussis-like syndrome in infants and young children were RSV, PIV II and III, Staphylococcus aureus, and M. pneumonia. Paroxysmal coughing was more severe in those with PIV III infection, either alone or mixed with other infections. In addition, these pediatric patients were more likely to suffer from cyanosis and dyspnea (8). These results were consistent with the present study. That is, bacterial infection, M. pneumonia infection, and mixed bacterial-mycoplasma infection were the primary causes of pertussis-like syndrome in Chinese children.
Pertussis-like syndrome usually has a prolonged and relapsing course in children, causing distress and economic burden to children and their parents. The present retrospective analysis of the etiology of pertussis-like syndrome in children in Chengdu identified the main pathogens specific to this region. Our study provides a reliable etiological basis for the clinical treatment of pertussis-like syndrome in children from Chengdu and may assist physicians in improving their decision-making in regard to appropriate medications. Bacterial infections caused by H. influenzae and S. pneumoniae are important causes of pertussis-like syndrome in children. We can be better prepared for preventing pertussis-like syndrome in children by early immunization with pneumonia and H. influenzae pneumonia vaccines. In future studies, we will carry out more analyses of the different types of bacteria causing pertussis-like syndrome in children and their sub-types and drug sensitivity. In conclusion, the present research findings provide a solid foundation for the prevention and clinical treatment of pertussis-like syndrome.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/tp-21-140
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tp-21-140
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tp-21-140). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The Institutional Review Committee approved the retrospective analysis without providing written ethical approval, because it was an objective report complying to the condition of protecting the privacy of the patients. Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zimmerman LI, Papin JF, Warfel J, et al. Histopathology of Bordetella pertussis in the Baboon Model. Infect Immun 2018;86:e00511-18. [Crossref] [PubMed]
- Miyashita N, Akaike H, Teranishi H, et al. Diagnostic value of symptoms and laboratory data for pertussis in adolescent and adult patients. BMC Infect Dis 2013;13:129. [Crossref] [PubMed]
- Mahmoudi S, Banar M, Pourakbari B, et al. Identification of Etiologic Agents of the Pertussis-like Syndrome in Children by Real-time PCR Method. Prague Med Rep 2018;119:61-9. [Crossref] [PubMed]
- Saiki-Macedo S, Valverde-Ezeta J, Cornejo-Tapia A, et al. Identfication of viral and bacterial etiologic agents of the pertussis-like syndrome in children under 5 years old hospitalized. BMC Infect Dis 2019;19:75. [Crossref] [PubMed]
- Wirsing von König CH, Rott H, Bogaerts H, et al. A serologic study of organisms possibly associated with pertussis-like coughing. Pediatr Infect Dis J 1998;17:645-9. [Crossref] [PubMed]
- Ferrer A, Calicó I, Manresa JM, et al. Microorganisms isolated in cases of pertussis-like syndrome. Enferm Infecc Microbiol Clin 2000;18:433-8. [PubMed]
- Cao JY, Pan JH. Progress in etiology, pathogenesis and clinical characteristics of pertussis syndrome. Zhonghua Er Ke Za Zhi 2020;58:158-61. [PubMed]
- Huang H, Deng L, Xiao F, et al. Clinical analysis of children with pertussis and significance of respiratory virus detection in the combined diagnosis. Zhonghua Er Ke Za Zhi 2017;55:580-5. [PubMed]
(English Language Editor: D. Fitzgerald)


