Epidemiologic survey on hospitalized neonates in China
Introduction
In 2002, the National Neonatal Study Group organized a nationwide large-scale epidemiological survey on preterm neonates (hereinafter referred to as the 2002 Data) to summarize the common causes for premature newborns and factors that would affect their outcomes, providing useful information for reducing the incidence and improving the prognosis for such babies (1). However, the 2002 Data did not reflect the up-to-date status of sick newborns in China as it failed to include the classification of diseases for full-term newborns. Hence, based on the 2002 survey, the Group of Neonatology of Chinese Pediatric Society and the Chinese Journal of Contemporary Pediatrics jointly organized this nationwide epidemiological survey on hospitalized neonates to retrospectively investigate the data of neonatology departments in 80 hospitals across 22 provinces (autonomous regions and municipalities) in 2005 to inform studies on the status quo of Chinese newborns.
Subjects and methods
Subjects
Eighty hospitals in 47 cities across the 22 provinces (autonomous regions and municipalities) of the northeast, north, east, northwest, southwest and south-central regions in China participated in this survey. These included the hospitals affiliated to medical schools in provincial capitals, provincial people’s hospitals, provincial maternal and child health hospitals, and provincial children’s hospitals. One general hospital and one maternity and child care center were randomly chosen from each non-capital city. Neonates hospitalized in the neonatology departments of these hospitals who were discharged from January 1, 2005, 0:00 to December 31, 2005, 0:00 were included in the study, with one thousand cases sampled from each hospital. In a department with less than 1,000 patients, all of the neonates would be included. For a department with more than 1,000 infants, those discharged on the 1st-20th, 1st-15th, 1st-10th or 1st-7th day of each month were included, i.e. only 2/3, 1/2, 1/3 or 1/4 of all neonates were selected, making the sample size around 1,000. The sampling ratio was dependent on the total number of patients in each department of a hospital as documented by the Medical Records room, and the number of days for sampling in each month was consistent.
Survey methodology
Preparation
A questionnaire form was designed for pilot survey. A specifically developed computer application was used to create the database. Three meetings were held in Shanghai, Hangzhou and Yanji to revise the survey program and provide training for principal investigators in major regions and provinces. Participants in the pilot survey included Xiangya Hospital of Central South University (Wang Qinghong), Maternal and Child Health Hospital of Hunan Province (Cheng Linxia), Maternal and Child Health Hospital of Yueyang City, Hunan Province (Li Ping), Hunan Provincial People’s Hospital (Li Yun), Xi’an Jiaotong University No.1 Affiliated Hospital (Liu Li), Shandong Yantai Yuhuangding Hospital (Chu Qing), Chengdu Children’s Hospital (Wang Xiaolei), Bao’an District Maternal and Child Hospital of Shenzhen City (Ye Zhenzhi), and Jiujiang Maternal and Child Health Hospital (Hao Ming). A total of 4,736 hospitalized cases were investigated, including 2,904 from obstetrics departments and 1,832 from neonatology departments. The pilot survey was primarily conducted to test the integrity and operability of the questionnaire and make adjustment accordingly. Therefore, the results were not included in the formal investigation.
Quality control
After trained and instructed on specific requirements for filling out the questionnaire form, principal investigators of major regions and provinces would communicate the requirements to hospital staff in the corresponding sites. Completed forms were collected and sent to the Pediatrics Department, Xiangya Hospital of Central South University. Upon examination by a designated reviewer, any hospital providing a large number of blank forms or untruthful contents would be excluded from the study together with all data from it. After data entry, a designated examiner would spot check 1% of the inputted data for consistency with the questionnaire forms. In the case of excessive errors found in the data from any inputter, a new clerk would reenter all of the entries in his place.
Survey procedure
Upon completion, the questionnaire forms were sent to the Pediatrics Department, Xiangya Hospital of Central South University by participating hospitals and, if verified, inputted into computer mainly by graduate students in the Department of Epidemiology and Biostatistics of the Public Health Division of Central South University Xiangya Medical School. Inputted data would not enter the central database until verified through spot check. A new inputter would reenter all of the data in place of his predecessor who produced unqualified entries.
Database creation
Data entries completed in the EpiData application by graduate students from the Department of Epidemiology and Biostatistics of the Public Health Division of Central South University Xiangya Medical School were converted into an SPSS database. To avoid data conflicts, each hospital was assigned a unique code composed of the Pinyin initials of its located region + province + city (omitted if capital) + hospital name. For example, the code for Xiangya Hospital of Central South University would be the initials of “South-central (ZhongNan) + HuNan + XiangYa”, i.e. “ZNHN-XY”; and the code for the Maternal and Child Health Hospital of Xiangtan, Hunan was ZNHN-XT-FY. For ease of quality inspection, each inputter was required to provide the data folder with his name. For example, if John Doe was in charge of entering the data from Xiangya Hospital, the name of the submitted folder should be “ZNHN-XY-John Doe.”
Statistical methods
SPSS11.0 software was used for statistical analysis. Categorical data were tested against the Chi-square distribution. Multivariate analysis of risk factors was conducted by logistic regression analysis with a P value of 0.05 indicative of statistical significance.
Results
Data collection
Data on 43,289 neonate patients were collected from 80 hospitals nationwide. Three hospitals were excluded from the study for data disqualification.
Status of hospitalized neonates
Basic information
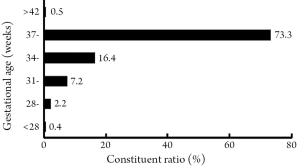
There were 43,289 hospitalized neonates in 80 hospitals across the country in 2005. Among them, premature newborns accounted for 26.2%, while full-term infants accounted for 73.8%, with a higher constituent ratio of premature newborns than the data in 2002 (19.7%) (1) (Figure 1). The male:female ratio was 1.73:1. Infants hospitalized within one week of birth accounted for 65.7%, while 34.3% were admitted one week later. Among the former group, 50.0% were admitted within 24 h of birth, 28.7% in 1-3 days, and 21.3% in 4-7 days; 60.8% of those hospitalized in 24 hrs were admitted within 6 hrs of birth, 17.8% within 7-12 hrs, and 21.4% beyond 12 hrs. As for the distribution of gestational age, neonates born earlier than 28 weeks, after 28 weeks, after 31 weeks, after 34 weeks, after 37 weeks and after 42 weeks accounted for 0.4%, 2.2%, 7.2%, 16.4%, 73.3% and 0.5%, respectively (Figure 2). The highest proportion of premature infants (16.4%) was late-preterm neonates born between week 34 and 36. Neonates with a birth weight less than 1,000 g, more than 1,000 g, more than 1,500 g, more than 2,500 g and more than 4,000 g accounted for 0.3%, 2.6%, 20.7%, 71.9%, 4.5%, respectively. In premature infants, those with a birth weight less than 1,000 g, more than 1,000g, more than 1,500 g, more than 2,500 g and more than 4,000 g accounted for 0.7%, 9.3%, 60.0%, 29.6% and 0.4%, respectively. The proportion of infants with a body weight less than 1,000 g was decreased when compared to the 2002 Data (3.6%). The incidence of small-for-gestational age (SGA) was 25.3% in preterm neonates, remarkably higher than that in full-term infants (6.3%) with significant difference (χ2=2,236.66, P<0.001).
Neonatal diseases
Respiratory diseases found in hospitalized neonates included pneumonia (46.2%, 19,193/41,588), asphyxia (17.1%, 7,147/41,806), meconium aspiration syndrome (MAS, 3.6%, 1,504/41,872), apnea (3.0%, 1,236/41,632), neonatal respiratory distress syndrome (RDS, 2.5%, 1,061/41,640), wet lung syndrome (1.9%, 781/41,597), and pulmonary hemorrhage (0.7%, 300/41,519).
Nervous system diseases included hypoxic ischemic encephalopathy (HIE, according to the 1996 Criteria) (2) (18.1%, 7,243/40,016), of which mild, moderate and severe cases accounted for 52.0%, 39.9% and 8.1%, respectively; intracranial hemorrhage (7.7%, 3,220/41,747); seizures (3.0%, 1,234/41,676); bilirubin encephalopathy (0.9%, 357/41,535); and intracranial infection (0.8%, 339/41,566).
Gastrointestinal diseases included gastrointestinal bleeding (1.8%, 742/41,647), gastric retention (1.2%, 505/41,722), gastroesophageal reflux (1.1%, 453/41,692), and necrotizing enterocolitis (NEC, 0.4%, 171/41,716).
As for circulatory system diseases, infants with congenital heart diseases accounted for 5.9% of all hospitalized neonates (2,455/41,793).
Infectious diseases found among them included neonatal omphalitis (5.7%, 2,375/41,745) and sepsis (5.0%, 2,060/41,353), and 24.9% of them (1,080/4,342) had a positive blood culture test. Bacterial pathogens consisted of staphylococcus (66.6%), Klebsiella (7.0%), E. coli (6.0%), Gram-positive bacteria (4.0%), Enterococcus (2.7%), Pseudomonas aeruginosa (0.9%) and others (12.8%). Viral infections accounted for 1.3% (560/41,576), the main pathogens being cytomegalovirus, EB virus, herpes simplex virus, rotavirus and hepatitis virus.
Hospitalized infants with neonatal jaundice accounted for 49.1% (17,582/35,792). The proportion of jaundice cases was 48.8% in full-term babies (12,923/26,459) and 49.9% in preterm infants (4,659/9,333). The constituent ratios of jaundice infants were 0.3%, 1.9%, 7.4%, 16.9%, 73.2% and 0.3% in groups with a gestational age less than 28 weeks, more than 28 weeks, more than 31 weeks, more than 34 weeks, more than 37 weeks and more than 42 weeks, respectively. Causes in descending order of frequency included physiologic jaundice (33.0%), infectious jaundice (18.3%), others (17.8%), unknown cause (14.4%), ABO blood group incompatibility (10.2%), breast milk (3.5%), G6PD (2.3%) and Rh blood group incompatibility (0.5%).
Cases with cold injury syndrome accounted for 2.9% of hospitalized neonates (1,205/41,736), in which 32.2% had a hard swollen area smaller than 10%, 44.7% had such area larger than 10%, 20.7% had such area larger than 25%, and 2.4% had such area larger than 50%; patients with degree I, II and II hard swelling accounted for 77.0%, 16.7% and 6.3%, respectively.
Those with congenital malformations accounted for 2.6% of hospitalized neonates (1,083/41,730), mainly including gastrointestinal malformations, chromosomal disorders, head and facial deformities and congenital heart diseases.
Hospitalized cases of blood diseases accounted for 6.7% (2,785/41,737), including anemia (5.7%), neonatal hemorrhagic disease (1.1%), polycythemia (0.9%), DIC (0.3%), and others (1.1%).
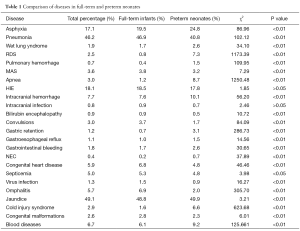
Diseases in full-term and preterm neonates
As shown in this survey, hospitalized preterm infants had a higher incidence of premature infant asphyxia, wet lung syndrome, RDS, pulmonary hemorrhage, apnea, intracranial hemorrhage, gastric retention, gastric reflux, gastrointestinal hemorrhage, NEC, cold injury syndrome, anemia and DIC when compared with full-term babies. On the other hand, full-term neonates had a higher incidence of pneumonia, MAS, bilirubin encephalopathy, convulsions, congenital heart diseases, sepsis, viral infections, omphalitis, congenital malformations and neonatal hemorrhagic diseases (Table 1).
Full table
Diseases affecting both mother and child
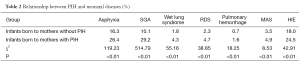
Analysis of one of the diseases that affect both mother and child, pregnancy-induced hypertension (PIH), revealed that newborns of PIH mothers had a remarkably higher incidence of asphyxia, SGA, wet lung syndrome, RDS, pulmonary hemorrhage, MAS and HIE than infants born to those without PIH (Table 2). Each of the differences was highly significant (P<0.01).
Full table
Neonatal outcomes
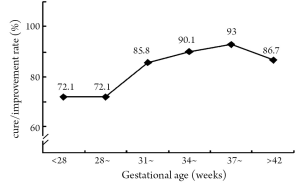
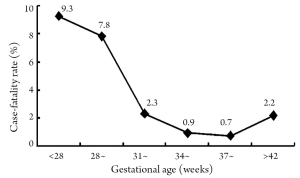
The cure rate was 63.9%, improvement rate 27.3%, discharge against medical advice 7.6%, and mortality 1.2%. Preterm neonates had a lower cure rate (87.2%) and higher mortality (2.0%) than full-term infants (92.9% and 0.7%), both differences being significant (χ2=314.24, P<0.01). With a larger gestational age, both cure rate and improvement rate showed an upward trend (Figure 3) as the case-fatality rate declined (Figure 4). The cure or improvement rates of preterm neonates in three gestational age groups (earlier than 28 weeks, after 28 weeks and 32 to 36 weeks) were higher (72.1%, 76.3% and 89.2%) than those in the 2002 data (50.0%, 61.4% and 73.7%) (1).
Of the deaths, 46.4% died within 24 h of admission, 17.5% died after 24 h, 9.2% between 48 to 72 h and 26.9% later than 72 h. Causes of death in descending order of constituent were respiratory failure (66.1%), heart failure (12.2%), renal failure (4.6%), shock (2.8%), DIC (2.2%) and others (12.1%). This study showed that 49.2% of the deaths had had asphyxia, a proportion higher than that in the surviving cases (15.9%).
Discussion
Regarding the disease distribution among hospitalized newborns in the department of neonatology, pneumonia was the most common respiratory disease, which suggested its major role in neonatal diseases in China. In addition, a high incidence of neonatal jaundice was found (49.1%). Bilirubin encephalopathy was remarkably more common in full-term infants than preterm neonates. Commonly seen in Chinese neonates, jaundice was closely observed by parents and physicians and often treated with timely intervention. However, jaundice in full-term infants was often overlooked as being non-physiological, thus leading to severe neurological damage in some infants, particularly full-term newborns, when monitoring and intervention was not performed in a timely fashion. Therefore, physicians should focus on the care of neonatal jaundice, look for any possible causes and apply appropriate intervention.
This study showed that 17.1% hospitalized newborns had asphyxia. As the leading cause of perinatal death in China, asphyxia was found in 49.2% of the death cases in our survey, a noticeably higher proportion than that in surviving infants (15.9%). Improved techniques of obstetric and pediatric physicians, intensified prenatal care, active treatment of pathological obstetric conditions and strict compliance with the new CPR techniques would be key to reducing the incidence of neonatal asphyxia.
Sepsis was found in 5% of the Chinese hospitalized neonates in this investigation, significantly less than those in India, 2000 (27%) (3). The most common pathogens of neonatal sepsis included Staphylococcus aureus and Klebsiella, which was consistent with the data in India (4), suggesting that sepsis was still a common disease among newborns in China as well as other Asian developing countries where particular efforts were needed for its prevention and control.
With a small gestational age, low weight and underdeveloped organ systems, preterm neonates had a higher incidence of asphyxia, RDS, neonatal bleeding disorders and other complications than full-term infants. Hence, to improve the survival rate and quality of life of preterm babies, physicians should closely monitor the development status of organs and organ systems for early prevention and management of potential complications in preterm babies.
This survey showed that 2.6% of all hospitalized newborns suffered neonatal congenital malformations. As reported by Tomashek et al. (5), congenital malformations were a strong risk factor for neonatal death. Therefore, promotion of eugenics and second-trimester screening for fetal defects would be helpful for early detection, diagnosis and treatment and reducing the incidence of congenital malformations as well as perinatal mortality.
In recent years, PIH, placental abruption and other diseases that affected both mother and child had been a focal concern in maternal and child care. This study revealed that newborns of PIH mothers had a higher incidence of asphyxia, SGA, wet lung syndrome, RDS, pulmonary hemorrhage, MAS and HIE than those born to mothers with a normal blood pressure. Other domestic reports also indicated a remarkably higher incidence of premature birth, neonatal asphyxia, and fetal distress and perinatal mortality in pregnant women with severe PIH than in mothers without serious complications (6,7). Therefore, it would be critical to enhance the self-care awareness of women of childbearing age and strengthen prenatal monitoring for PIH mothers. Termination of pregnancy could be implemented if necessary to reduce maternal and neonatal complications and avoid death.
Data in this study showed a neonatal mortality of 1.2%. Qiao Junying, et al. (8) reported a mortality of 2.7% among NICU infants from 2003 to 2005, where 43.3% of deaths were preterm infants. Wu Qing, et al. (9) reported a neonatal mortality of 3.6% in the hospitalized group in 2005. In the United States (2002), the mortality of late preterm babies was 7.9/1,000 live births, significantly higher than that in full-term newborns (2.4/1,000 live births) (10). Hence, further efforts should be deployed to reduce the neonatal mortality in China. Since most of the deaths occurred within 24 h of admission, the first 24 h became the critical period where focuses should be concentrated on monitoring of vital signs and condition changes and timely treatment. In view of the high mortality of premature infants (2.0%) compared with full-term babies (0.7%), treatment of complications during pregnancy to prevent premature birth, as the key to reducing perinatal morbidity and mortality, would play an important role in boosting the quality of perinatal care.
Acknowledgements
Funding: The survey is supported by Nestle (China) headquarters.
We thank our academic advisers, Professor Song Li (Department of Pediatrics, Third Affiliated Hospital of Peking University) and Professor Shuoqi Li (Epidemiology and Biostatistics Faculty of the Public Health Division, Central South University Xiangya Medical School), for their guidance on this epidemiological survey; Associate Professor Xingli Li (Epidemiology and Biostatistics Faculty of the Public Health Division, Central South University Xiangya Medical School) for the data entry application she developed for the study; and graduate student Mengshi Chen (Department of Epidemiology and Biostatistics of the Public Health Division, Central South University Xiangya Medical School) for work on data compilation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wei KL, Yang YJ, Yao YJ, et al. An initial epidemiologic investigation of preterm infants in cities of China. Chin J Nat Med 2005;7:25-8.
- Group of Neonatology of Chinese Pediatric Society. Diagnostic criteria and clinical staging of hypoxie-ischemicencephalopathy. Chin J Pediatr 1997;35:99-100.
- Sankar MJ, Agarwal R, Deorari AK, et al. Sepsis in the newborn. Indian J Pediatr 2008;75:261-6. [PubMed]
- Deorari AK, Chellani H, Carlin JB, et al. Clinicoepidemiological profile and predictors of severe illness in young infants (< 60 days) reporting to a hospital in North India. Indian Pediatr 2007;44:739-48. [PubMed]
- Tomashek KM, Shapiro-Mendoza CK, Davidoff MJ, et al. Differences in mortality between late-preterm and term singleton infants in the United States, 1995-2002. J Pediatr 2007;151:450-6, 456.e1.
- Lu F. Effect of the severe complications of pregnancy-induced hypertension syndrome on the outcome of perinatal newborn. Modern Hospital 2007;7:31-4.
- Zhang FL. Incidences of pregnancy-induced hypertension syndrome in two different populations. Chin J Nat Med 2007;9:344-5.
- Qiao JY, Luan B. Perinatal deaths in intensive care unit: analysis of 196 cases. Chin J Misdiagn 2007;7:5074-5.
- Wu Q, Li J, Chen M, et al. Ailment varieties and the causes of death in 446 neonatal cases in a general hospital. Pract J Clin Med 2007;4:42-3.
- Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2005. Natl Vital Stat Rep 2006;55:1-18. [PubMed]