
Study on normal reference value of fetal facial profile markers during the first trimester of pregnancy
Introduction
Fetal facial features are characterized by bulges, which is exactly opposite to the facial plane of the adult. The development of the fetal jaw determines the degree of bulging. Mandibular hypoplasia, known as micrognathia, and abnormal development of the maxilla affect the contours of the fetus and facial bulging. These diseases often involve chromosomal abnormalities, and such fetuses may give rise to excessive amniotic fluid due to difficulty in swallowing during continual growth and development, difficulty in eating after birth, and severe respiratory distress syndrome. The challenges encountered by severely affected children can bring a heavy burden to the whole family (1).
The abnormal development of the fetal face is related to dysplasia between the first iliac crest in the embryonic period and the first cleft palate (2). The ossification begins during the 8th week of embryonic growth and develops into the tibia, and temporal bones through intramembranous ossification. By the 11th week of pregnancy, the fetal face is basically developed, so the optimal time for assessment of fetal facial malformation by ultrasound is early pregnancy, actually most facial structures of the fetus have been differentiated during the first trimester.
Initially, Cicero et al. (3) performed ultrasound examination on 3,829 fetuses aged 11–14 weeks. The results showed that the presence and absence of fetal nasal bone defects and chromosomal defects cold be reflected in crown-rump length (CRL), nuchal translucency (NT), nuchal fold (NF) thickness, and ethnicity. Later, Rotten et al. (4) studied 18–28 week fetuses with small jaw deformity and mandibular retraction, and proposed the concept of inferior facial angle (IFA), which is considered to be constant in normal fetuses, with an average angle of (65.5°±8.13°). Borenstein et al. (5) measured the frontomaxillary facial (FMF) angle of 11–13+6 week fetuses with chromosome and trisomy 18, followed by normal fetuses on the 11–13+6-week, and found that the FMF angle decreased with the growth of fetal CRL. The comparison between FMF angle and mandibulomaxillary facial (MMF) angle of the normal fetus decreased with the increase of CRL, and the ratio of FMF to MMF stabilized at 0.74; the ratio of FMF to MMF in trisomy 18 was 0.86 (6). Sepulveda et al. (7) analyzed the normal posterior triangulation of the fetus at 11–13+6 weeks (the posterior nasal coronal section showed a strong echo triangle formed by the primary hernia and bilateral maxillary frontal processes), and the mandible was found after the gap. With the growth of CRL, the gap of the mandible grows. The mandibular gap was not shown in the small jaw deformity fetuses, probably because the mandibular gap was replaced by a bony structure and had been obscured. Palit et al. (8) pointed out that the fronto-naso-mental (FNM) angle diagnosis of small jaw deformity is very objective, and the mean FNM angle of 81 normal fetuses aged 18–35 weeks was 146.4°. As early as 1952, Riedel proposed the definition of A point-nasion-B point (ANB) angle (9). In recent years, some researchers have renamed the ANB angle the maxilla-nasion-mandible (MNM) angle by collecting normal research data (10), and proposed that MNM angle can be used in middle and late pregnancy as a useful tool for assessing abnormal facial contours in the fetus. In addition, the fetal profile line (FPL) is also an intuitive indicator for assessing the facial contour. The FPL is commonly negative in the trisomy 18 (11).
It is worthwhile to affirm the role of indicators of facial contours such as IFA, FNM, and MNM angle in the assessment facial and aneuploidy abnormalities in middle and late pregnancy. Structural malformation, which has a decisive role in prenatal ultrasound diagnosis, and sensitivity is higher than the above indicators; but aneuploid fetuses tend to be more obvious during middle and late pregnancy.
Contrarily, during early pregnancy, the display rate of abnormal fetal structure is inferior to that in the second half of pregnancy. Therefore, the abnormal index of fetal facial contour is very meaningful, and it has the same feasibility as the facial and facial contour indicators in the second half of pregnancy. We aimed to reflect its repeatability in this study. Early detection and diagnosis of fetal facial abnormalities in early pregnancy is critical for rational guidance of pregnancy outcomes. Therefore, this study was mainly aimed at nasal bone display, IFA, FNM, FMF, and MMF angle in normal chromosomal fetuses during early pregnancy (CRL between 45 and 84 mm). A single index may not reflect the real fetal facial contour. Therefore, this study combined with the 8 indexes widely studied at present, in order to establish the range to be more suitable for the Chinese population. We present the following article in accordance with the MDAR reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-21-573/rc).
Methods
Case collection
From September 2018 to December 2019, a total of 1,000 cases of women in their early pregnancy period (11–11+6 weeks) were recruited to this study. All were singleton pregnancies, the women were aged 18–42 years (average 29.1±4.4 years), and the fetal CRL was 45–84 mm (average 67.2±6.7 mm).
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of two hospitals, General Hospital of Ningxia Medical University (No. 2017-182) and Ningxia Maternal and Child Health Care Hospital (Ningxia Children’s Hospital), and informed consent was taken from all the patients.
This study was conducted by 2 experienced operators who had obtained their UK Early Screening Qualifications. When the position of the fetus was not ideal, the pregnant woman was encouraged to exercise until the position of the fetus became satisfactory, and ultrasound images of the median sagittal section, posterior sagittal section, coronal section, and transverse section of the face were captured. Normal frequency was used for the majority of participants, and the frequency was deepened for those with thicker abdominal fat.
Next, NT measurement, amniocentesis, and non-invasive chromosome karyotype analysis were conducted. Using the images from ultrasound, the facial bones, maxillary bone, mandibular bone markers, the existence of the mandibular gap, sagittal section, and the posterior triangle of the nose were measured, followed by measurement of the length of the nasal bone, IFA angle, FNM angle, FMF angle, MMF angle, MNM angle, and FP line. Construct a clear value range suitable for Chinese.
Standard surface section and standard measurement
The median standard sagittal section
The fetus is in a natural stretch state, the sound beam plane is perpendicular to the skin of the fetal neck and back, and the two-dimensional sonogram should show the midline structures of the fetus, such as the diencephalon, rhomboid, nasal bone, nose tip, palate, mandible, and so on.
Measurement of nasal bone length (NBL)
The nasal bone section can show 3 clear lines on the nose, from top to bottom, they are nasal tip, skin and nasal bone. The average of 3 measurements is taken as the final measurement.
IFA angle measurement
The first line is drawn orthogonal to the vertical part of the forehead, drawn at the level of the synostosis of the nasal bones (reference line), a second line is drawn joining the tip of the mentum and the anterior border of the more protrusive lip (profile line), and the angle between the 2 lines is measured as the IFA (Figure 1A).
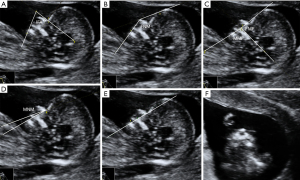
FNM angle measurement
A line is drawn connecting the most prominent point of the forehead bony front with the soft tissue of the nose; the second line is the connection between the anterior border of the mandible and the soft tissue of the nose, and angle between the two lines is measured as the FNM (Figure 1B).
FMF and MMF angle measurement
The upper anterior inflection point of the maxilla constitutes the fulcrum of the FMF angle, the first line of the FMF angle is extended along the upper iliac surface, and the second line is the fulcrum and the forehead anterior border. An extension of the protruding point, the 2 lines intersect as an FMF angle. The first line of the MMF angle coincides with the first line of the FMF angle, and the second line is the extension line of the fulcrum of the FMF angle and the anterior edge of the mandible. The angle between the 2 lines is the MMF angle (Figure 1C).
MNM angle measurement
The angle between the line connecting the forefront of the maxilla to the nasal root and the line connecting the anterior border of the mandible to the nasal root (Figure 1D).
FP line
Consisting of a line that passes through the midpoint of the anterior border of the mandible and the nasion. When the FP line extension line passes through the prefrontal bone, it is defined as 0; when FP line is below the front of the forehead bone, it is defined as negative; when the FP line extension line passes through the front of the forehead bone, it is defined as positive (Figure 1E).
Retronasal triangle view
Observe the presence of the mandibular gap in the retronasal triangle coronal view, sagittal section, and transverse section (Figure 1F).
Main equipment
The GE Voluson E8 color Doppler ultrasound system (GE Healthcare, Chicago, IL, USA) was selected and operated with C-5-D and RA84-8-D probes. The pregnant woman was placed in the supine position and the fetus was screened according to routine early pregnancy ultrasound.
Statistical analysis
The software SPSS 25.0 (IBM Corp., Chicago, IL, USA) was used for statistical analysis, the measurement data were expressed as by mean ± 1.96 standard deviation (SD), and the single-sample t-test was used. A P value <0.05 was considered statistically significant.
Results
A total of 1,000 fetuses were included in this study, among which there were 800 cases for whom amniocentesis, non-invasive karyotype analysis, and normal ultrasound, the above several measurements were able to be obtained. The remaining cases, due to no chromosome examination, fetal body overbuckling, fetal nasal bone not displayed, and poor fetal maxillary display, standard cuts were unattainable, making it impossible to measure their data.
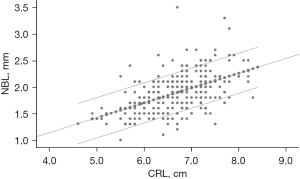
Measurement of normal fetal nasal bone length from 11 to 13+6 weeks of gestation
The average length of the nasal bone was 1.89±0.27 mm, and the 5th and 95th percentiles were 1.41 mm and 2.30 mm, respectively. There was a significant linear correlation between the length of the nasal bone and the fetal head and hip length. This suggested that the length of the nasal bone increases with the increase of fetal CRL in early pregnancy. The linear regression equation is Y=0.280X+0.02 (r=0.71, P<0.05) (Figure 2).
IFA angle measurement of normal fetus from 11 to 13+6 weeks of gestation
The average IFA angle was 64.91°±6.73°, and the IFA angle conformed to the normal distribution curve, which is maintained within a stable range. The 5th and 95th percentiles were 54.00° and 75.69°, respectively (Figure 3). There was no significant correlation between IFA angle and CRL (P>0.05), suggesting that the IFA angle in early pregnancy is not affected by fetal growth and is fixed within a normal range. When the test value was 65.5°, there was no significant difference in the mean value of IFA (P>0.05). This suggested that in the normal fetus, the IFA angle in early pregnancy is basically the same as that in middle and late pregnancy, and the normal IFA angle can be determined. The range can be applied to any gestational age during pregnancy.
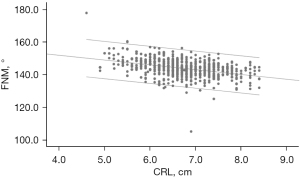
FNM angle measurement of normal fetus from 11 to 13+6 weeks of gestation
The average IFA angle was 143.79°±6.15°, and the IFA angle conformed to the normal distribution curve, which was maintained within a stable range. The 5th and 95th percentiles were 135.91° and 152.29°, respectively. There was a linear correlation between fetal FNM angle and CRL. With the slight increase of FNM angle of fetal growth, the linear regression equation is Y=163.2−2.94X (r=−0.333, P<0.05; Figure 4). This suggests that the FNM angle seems to have a certain correlation with the fetal gestational age.
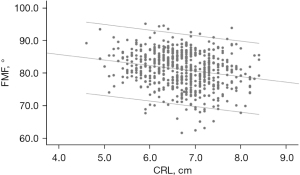
Normal fetus FMF angle and MMF angle measurement results at 11–13+6 weeks of pregnancy
The average FMF angle was 81.06°±5.68°. The FMF angle conformed to the normal distribution curve. The 5th and 95th percentiles were 71.47° and 88.9°, respectively. There was a significant linear correlation between fetal FMF angle and CRL. When the CRL was 4.5–8.4 cm, the range of FMF angle was between 78.17° and 84.48°. As the FMF angle of fetal growth decreased, the linear regression equation was Y=92.53−1.71X (r=−0.21, P<0.001) (Figure 5).
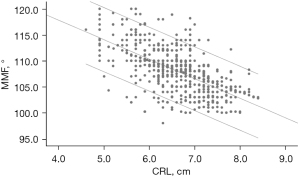
The MMF angle average was 107.71°±4.09°. The FMF angle conformed to the normal distribution curve. The 5th and 95th percentiles were 102.0° and 115.0°, respectively. There was a significant linear correlation between fetal FMF angle and CRL. As the fetal growth FMF angle decreased, when the CRL was 4.5–8.4 cm, the MMF angle ranged from 87° to 101.63°, and the linear regression equation was Y=118.5−3.75X (r=−0.65, P<0.001) (Figure 6).
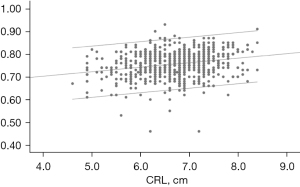
The average value of the FMF angle to the MMF angle was 0.75°±0.05°, which is close to the conclusions of Borenstein et al. (5), and the ratio results did not change significantly with the growth of the fetal CRL; the equation was: Y=0.62+0.02X, r=0.23, P<0.001) (Figure 7). The above results provide a good reference for the facial angle of the fetus in early pregnancy.
MNM angle measurement of normal fetuses from 11 to 13+6 weeks of gestation
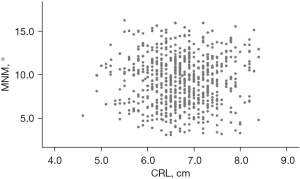
The mean value of MNM angle was 9.55°±2.84°, the FMF angle conformed to the normal distribution curve, and the 5th and 95th percentiles were 4.80° and 14.20°, respectively. There was no significant linear correlation between fetal MNM angle and fetal CRL (r=0.008, P>0.1), which did not increase or decrease with fetal growth (Figure 8). de Jong-Pleij et al. (1) believe that the mean MNM angle of the 16–36 weeks fetus is 13.5°, and the mean value of the MNM angle is significantly different when the test value is 13.5° (P<0.001). The results showed that MNM angle was stable in a normal range from 11 to 13+6 weeks, and the mean value may be smaller than that in the middle and late stages of pregnancy.
FP line measurement of normal fetus from 11 to 13+6 weeks of gestation
Among 177 cases with “0” value, the effective percentage was 22.1%; among 623 cases with “positive” value, the effective percentage was 77.9%; there were 0 “negative” value cases. The FP line did not change significantly with the growth of the fetus.
Observation of mandibular gap in normal fetus from 11 to 13+6 weeks of gestation
A total of 795 cases of obvious mandibular gap were observed, the effective percentage was 99.4%; the narrowing of mandibular gap was 5 cases, and the effective percentage was 0.6%.
Discussion
Fetuses with chromosomal abnormality, especially trisomy 18 and trisomy 21, often have typical facial features, such as small jaw, flat face, and so on, and ultrasound screening for fetal facial profile markers, jaw, and nasal bone development can improve the diagnostic rate. However, previous prenatal ultrasound screening has been limited to subjective observation by the operator, and has lacked a unified diagnostic criterion. Further, most of the ultrasound measurements proposed by researchers regarding the development of the jaw are mostly limited to the fetus in the second half of pregnancy. This may be because most structural abnormalities are often manifested in the second half of pregnancy, or that the position of the fetus in early pregnancy is not ideal and it is not easy to retain the facial angle.
The standard surface section for our routine work during early pregnancy (11–13+6 weeks) for NT screening is the median sagittal section, which needs to show the diencephalon, rhomboid, nasal bone, maxilla, mandible, and spine. Consistent with the required surface section of the study, the measurement of NBL, IFA, FNM, FMF, MMF, MNM angle, and FP line requires the marked nasal bone, forehead, maxilla, and mandible to be clearly displayed. In addition, from the perspective of embryonic development mechanism, the maxillary branch of the first branchial arches develops into the maxilla and zygomatic arch; however, the mandible is developed from the mandibular branch. Nasal bone begins to develop when the embryo reaches 6 weeks, and at 9–11 weeks, the nasal bones began to ossify. The secondary tendons a fused by the lateral frontal processes perpendicular to the sides of the tongue, and then turn into a horizontal position and ossify, eventually forming the maxilla and frontal bone. By the 11th gestational week, the fetal face is basically developed (2). Therefore, the above angle measurement avoids missed diagnosis and false positives caused by non-ossification, so that the screening of facial deformities can be advanced to early pregnancy. The nasal bone and the frontal bone are anatomically independent. When the measurement needs to mark the nasal root position, the junction of the nasal root and the forefront of the frontal bone can be used as a marker point, and the measurement of IFA, MNM angle, and FP line indicators is not affected.
The abovementioned development of fetal nasal bones is basically completed at 11 weeks, and the average and normal range of fetal nasal bones at 11–13+6 weeks are helpful to predict the shortness of fetal nasal bone development in early pregnancy. Sonek et al. (12) have published a comprehensive measurement of the length of each gestational age of the fetus (NBL), and believe that the NBL of fetuses with trisomy 21 in early pregnancy is shorter than that of normal fetuses with a corresponding CRL, but the difference between the normal value and the abnormality is small. Therefore, it is considered that the measurement of the length of the nasal bone is not effective in screening during early pregnancy. This study concluded that the range of nasal bone length combined with NT measurements can help to improve the detection rate of fetal facial abnormalities.
The IFA angle measurement requires a straight line to be drawn perpendicular to the forehead of the nose bone. This may cause some measurement errors. In the past, many academics thought that the average value of the 18–28 weeks IFA angle was fixed at 65.5°, the mean minus 2 standard deviations was the diagnostic criterion, and the IFA <50° could be diagnosed as a micrognathia malformation. However, this is not enough. With the continuous improvement of prenatal diagnostic techniques and the importance of early diagnosis of fetal facial deformities, we need to establish relevant reference ranges for different gestational weeks. The study found that the average value of IFA in early pregnancy was 64.91°, the abnormal value was 51.5°, which was below 2 times the standard deviation. This is slightly different from the diagnosis of most researchers. It may be that the fetal mandible in early pregnancy is a forward and downward growth relative to the maxilla, and the formation of the IFA angle requires the most prominent leading edge of the soft tissue of the upper or lower lip. However, referring to the results of many researchers measuring micrognathia fetuses, most of the measured values are far below 50°, which means that when the measured value is far less than 50° or even 51.5°, the mild small mandible is insensitive to angle measurement and difficult to diagnose. This indicates that diagnosing the small mandible at an early gestational time has a clear degree of confidence.
The study also pointed out that the measurement of FNM angle is inconsistent with the results of other researchers. Palit et al. proposed a cut off value of 142° to define micrognathia (8). Our study concluded that the average FNM angle of normal fetuses was 143.79° from 11 to 13+6 weeks, the abnormal value was 131.5°, which was below 2 times the standard deviation. Luedders et al. (13) also questioned the views of Palit et al. In their small jaw (range, 100° to 134°), FNM angle measurements were much lower than 142°, and even many normal controls were lower than 142°. This study found that FNM angle decreased slightly with the increase of fetal CRL, which also indicates that the fixed value of 142° is not enough to be strong evidence for the diagnosis of small mandible, and is not conducive to the diagnosis of early pregnancy.
Borenstein et al. reported that the 2 facial indicators of FMF and MMF angle in early pregnancy were studied in the diagnosis of trisomy 18 fetus (6). The FMF angle reflects the median facial dysplasia, and the MMF angle reflects the relationship between the upper jaw and the lower jaw. This study showed that both the FMF angle and the MMF angle decrease with the increase of fetal CRL, which is consistent with Borenstern’s conclusion. When the CRL is in the 4.5–8.4 cm interval, the FMF angle range is close to that of the Borenstern but MMF angle is significantly smaller than their conclusion. The ratio of the 2 angles was fixed at 0.75 and did not change with the growth of CRL. This is close to the fixed value of 0.74 obtained by Borenstern. The ratio data can better reflect the change of the whole face as it indicates that both FMF angle and MMF angle have different angles. It is an indicator that better reflects facial contour abnormalities, but it ignores the influence of the nose on the entire facial profile markers. In addition, these 2 angles are applied to the maxillary branch as a marker point, indicating the importance of the maxillary branch in these 2 angle measurements; the maxillary branch does not directly affect the facial bump, but is directly affected by the accuracy of development and measurement. The above studies indicate that FMF and MMF angle in early pregnancy can be used as indicators for the evaluation of micrognathia, but the ratio data seems to be more reliable in assessing the developmental abnormalities of the fetal face as a whole.
The concept of the MNM angle originated from the ANB angle of the adult to evaluate the cephalogram of the anterior and posterior maxilla and mandible. de Jong-Pleij et al. (1) obtained a mean fetal MNM angle of 13.53° for 16–36 weeks gestation, and there was no significant correlation between MNM angle and gestational age, findings with which our study is consistent. However, our study concluded that the mean MNM angle is smaller than the average of the MNM angles of the above researchers, and it is surprising that the MNM is smaller at 14–39 weeks of normal Korean fetal pregnancy, with an average of only 4.7° (standard deviation 3.3°). All of the above studies show that it is not easy to accurately measure the MNM angle, and the range of normal values of MNM is very narrow (4.80°–14.20°), requiring accurate measurement. Therefore, whether the normal range of MNM angles is related to the facial features of ethnic groups, and whether it is possible to obtain a more reference value for expanding the sample size remains to be studied.
When the FP line is negative, it often indicates that the fetus has a micrognathia deformity or a tilted forehead. This is common in the trisomy 18. Studies have also shown that the trisomy 21 fetus exhibits a positive FP line (14); however, the data of “positive” values in this study were 623 cases, accounting for 77.9% of the total. Inconsistent with the previous researchers’ conclusions, the reason for the analysis is that the facial profile markers of the fetus are different from that of adults, characterized by protrusions, which suggests that the normal value of the FP line in the fetal period cannot be negative. At the same time, it also implies the error of FP line “0” in normal fetus. Therefore, if the FP line is negative, it is more likely to suggest trisomy 18, which also highlights the value of FP line for diagnosing micrognathia. It can also be used to distinguish between trisomy 18 and trisomy 21. This study also found that the normal fetus has a gap in the mandible during early pregnancy. Only 5 cases of the mandible had narrowed gaps but the gaps still existed, considering that the surface section was not standard or may be caused by individual differences. Sepulveda et al. (7) believe that the gap width of the mandible in early pregnancy increases with the increase of CRL, but for fetuses with small mandibles, the gap almost disappears as the gap of the mandible. This study showed that the gap between the normal fetus and the mandible exists. The conclusions were generally consistent, suggesting that the possibility of micrognathia can be ruled out in the presence of fetal mandibular gap in early pregnancy.
Conclusions
In summary, this study established a range of normal reference values for facial features and angles during early pregnancy, If the measurement is not within this range, the possibility of fetal facial development abnormalities and chromosome abnormalities should be suspected. Finding abnormalities in early pregnancy can not only provide clinicians with sufficient time to evaluate fetal prognosis, providing a reference for prenatal early detection and diagnosis of fetal micrognathia and other facial abnormalities.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-21-573/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-21-573/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-21-573/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of two hospitals, General Hospital of Ningxia Medical University (No. 2017-182) and Ningxia Maternal and Child Health Care Hospital (Ningxia Children’s Hospital), and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- de Jong-Pleij EA, Ribbert LS, Manten GT, et al. Maxilla-nasion-mandible angle: a new method to assess profile anomalies in pregnancy. Ultrasound Obstet Gynecol 2011;37:562-9. [Crossref] [PubMed]
- Thomson A. A description of congenital malformation of the auricle and external meatus of both sides in three persons. Proc R Soc Edi 1845;3:433.
- Cicero S, Longo D, Rembouskos G, et al. Absent nasal bone at 11-14 weeks of gestation and chromosomal defects. Ultrasound Obstet Gynecol 2003;22:31-5. [Crossref] [PubMed]
- Rotten D, Levaillant JM, Martinez H, et al. The fetal mandible: a 2D and 3D sonographic approach to the diagnosis of retrognathia and micrognathia. Ultrasound Obstet Gynecol 2002;19:122-30. [Crossref] [PubMed]
- Borenstein M, Persico N, Kaihura C, et al. Frontomaxillary facial angle in chromosomally normal fetuses at 11+0 to 13+6 weeks. Ultrasound Obstet Gynecol 2007;30:737-41. [Crossref] [PubMed]
- Borenstein M, Persico N, Strobl I, et al. Frontomaxillary and mandibulomaxillary facial angles at 11+0 to 13+6 weeks in fetuses with trisomy 18. Ultrasound Obstet Gynecol 2007;30:928-33. [Crossref] [PubMed]
- Sepulveda W, Wong AE, Viñals F, et al. Absent mandibular gap in the retronasal triangle view: a clue to the diagnosis of micrognathia in the first trimester. Ultrasound Obstet Gynecol 2012;39:152-6. [Crossref] [PubMed]
- Palit G, Jacquemyn Y, Kerremans M. An objective measurement to diagnose micrognathia on prenatal ultrasound. Clin Exp Obstet Gynecol 2008;35:121-3. [PubMed]
- Riedel RA. The reliability of maxillary structure to cranium in malocclusion and in normal occlusion. Angle Orthod 1952;22:140-5.
- Roelfsema NM, Hop WC, Wladimiroff JW. Three-dimensional sonographic determination of normal fetal mandibular and maxillary size during the second half of pregnancy. Ultrasound Obstet Gynecol 2006;28:950-7. [Crossref] [PubMed]
- Nicolaides KH, Salvesen DR, Snijders RJ, et al. Fetal facial defects: associated malformations and chromosomal abnormalities. Fetal Diagn Ther 1993;8:1-9. [Crossref] [PubMed]
- Sonek JD, Cicero S, Neiger R, et al. Nasal bone assessment in prenatal screening for trisomy 21. Am J Obstet Gynecol 2006;195:1219-30. [Crossref] [PubMed]
- Luedders DW, Bohlmann MK, Germer U, et al. Fetal micrognathia: objective assessment and associated anomalies on prenatal sonogram. Prenat Diagn 2011;31:146-51. [Crossref] [PubMed]
- de Jong-Pleij EA, Ribbert LS, Pistorius LR, et al. The fetal profile line: a proposal for a sonographic reference line to classify forehead and mandible anomalies in the second and third trimester. Prenat Diagn 2012;32:797-802. [Crossref] [PubMed]



