
Teardrop and sourcil line (TSL): a novel radiographic sign that predicts residual acetabular dysplasia (RAD) in DDH after closed reduction
Introduction
Developmental dysplasia of the hip (DDH) is one of the most common developmental deformities of the lower extremities and one of the leading causes of future osteoarthritis and hip arthroplasty, including hip dislocation, subluxation and acetabular dysplasia (1,2). The key to treatment is early diagnosis and achieving stable concentric reduction. Although the popular method of sonographic hip screening can diagnose DDH as early as possible, delayed diagnoses still occur in some children (3,4). Closed reduction (CR) and spica cast immobilization is one of the main methods used to treat DDH, and MRI is not only useful to confirm successful reduction but may also help to predict outcome by evaluating following dislocation (5-7). However, residual acetabular dysplasia (RAD) after CR is still a major problem in clinical practice, and pelvic osteotomy is indicated if RAD persists (8-11). To establish early and reliable predictors of RAD, several radiographic parameters have been investigated such as the acetabular index (AI), central edge angle (CEA), etc. But, determination of the time when a further procedure is required remains controversial because these parameters need to be observed over a long time period and have some limitations (11-19). Surgeons need some more reliable and easier radiographic parameters that will predict future changes in RAD after CR.
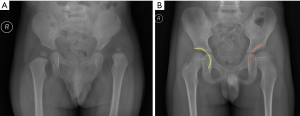
The acetabular teardrop is a landmark seen in the inferior medial acetabulum on the anteroposterior (AP) X-ray of the pelvis. The sourcil is a curved area of dense bone on the weight-bearing surface of the acetabulum and represents a stress distribution within the hip joint indirectly. Both the teardrop and sourcil are correlated with the development of the acetabular (11,19-23), so we hypothesized that if the smoothly curved line produced along the lateral margin of the teardrop that follows the curve of the sourcil [teardrop and sourcil line (TSL)] (Figure 1) could predict the outcome of DDH after CR. To the best of our knowledge, no previous research has combined the teardrop and sourcil to evaluate DDH after CR.
In this study, we retrospectively reviewed dislocated hips treated by CR in our hospital with a follow-up time of at least 2 years. The purpose of this study was to evaluate the new radiographic sign of TSL in pediatric patients with DDH and predict RAD after CR. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-21-401/rc).
Methods
Patients
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Children’s Hospital of Fudan University Ethics Committee (No. 2015181), and individual consent for this retrospective analysis was waived. Hip dislocation cases were collected from October 2011 to December 2017. The inclusion criteria were: (I) dislocation-type DDH treated with CR and spica casting under general anesthesia; (II) at least 2 years of follow-up. Children with neuromuscular disease, endocrine disease, once treated, incomplete information, and hips treated with open reduction because of redislocation immediately after CR were excluded.
A total of 104 patients (125 hips) were enrolled; there were 91 female (87.5%) and 13 male (12.5%) patients. Eighty-three hips (80%) were in patients with unilateral DDH, 21 hips (20%) were bilateral. Of the 83 unilateral cases, 51 (61%) were left hips and 32 (39%) were right hips. The mean age was 18.3±3.9 months (range, 9–32 months) at CR and the average follow-up time was 50.2±14.5 months (range, 24–89 months). An osteotomy was performed in 31 (25%) of the 125 hips at a mean age of 54.9±8.8 months (range, 39–79 months). The osteotomies included 1 Pemberton osteotomy, 27 Salter osteotomies and 3 combined Salter and femoral osteotomies.
Treatment procedure
CR was performed under general anesthesia, and adductor longus tenotomy was applied when soft-tissue contracture. Subsequent immobilization was achieved with a human position hip spica cast, keeping the hips in 90–100° flexion and 40–50°abduction. MRI was used to evaluate the adequacy of reduction within 3 days post-operation. After 3 months the spica cast was changed to a fixed abduction brace, which remained in place for 3–6 months.
Radiologic assessment
Picture Archiving and Communication System (PACS) imaging technology was used to measure the acetabular index (AI) at different time points. We used the lateral osseous margin of the acetabular roof instead of the lateral end of the sourcil when measuring the AI on the anteroposterior (AP) pelvis radiograph. In order to get standard pelvis radiograph, child was in supine position when taking X-ray, with the first toes of both feet were brought together, the pelvis was not rotated or tilted, and the distance between the tube and the film was 100 cm. RAD was determined according to the modified Severin criteria (24): grades I and II were classified as satisfactory and grades III to VI were classified as unsatisfactory. The degree of hip dislocation was classified by the International Hip Dysplasia Institute (IHDI) classification (25). RAD and TSL were judged at the last follow-up or before osteotomy surgery. The time when TSL became continuous after CR was recorded. The cases were divided into two groups according to whether TSL became continuous or not. Two independent doctors measured and collected all data.
Statistical analysis
The data were analyzed using IBM SPSS Statistics Version 19.0 (IBM Corporation, Armonk, NY, USA). Continuous variables were collected as the mean ± SD. Categorical data were analyzed with the χ2 test. Continuous results were analyzed using the t-test. Binary logistic regression analysis was used to determine the prognostic factors for RAD. The intraclass coefficient (ICC) with 95% confidence intervals was used to quantify agreement of the continue of TSL between the interobserver and intraobserver. The ICC was interpreted as follows: less than 0.2 as slight agreement, 0.21 to 0.40 as fair agreement, 0.41 to 0.60 as moderate agreement, 0.61 to 0.8 as good agreement and values more than 0.80 as almost perfect agreement. when the classification of TSL was discrepant between the observers, the classification was finally decided by senior surgeon (Bo Ning). Differences were considered significant when P<0.05.
Results
The interobserver (ICC =0.648, 0.533 to 0.739) and intraobserver (ICC =0.781, 0.702 to 0.841) reliability was good for the continue of TSL. Demographic data for the total of 125 hips are shown in Table 1. The mean AI at CR was 38.5°±4.3° (range, 27.6° to 47.6°). The RAD incidence was 73.6% (92/125), non-RAD incidence was 26.4% (33/125) (Table 2). Patients who developed RAD had a significantly larger AI, greater age and higher IHDI grade at CR, but a lower rate of continuous TSL than those who did not (P=0.006, 0.035, 0.049 and 0.000, respectively) (Table 3). The power of the prognostic factors for RAD of AI, age and IHDI grade at CR, and TSL were determined by binary logistic regression analysis, and the results showed that AI at CR and TSL were the prognostic factors for RAD (P=0.017 and 0.001, respectively) (Table 4, Figure 2).
Table 1
| Characteristics | Data |
|---|---|
| Sex, n (%) | |
| Male | 13 (12.5) |
| Female | 91 (87.5) |
| Side, n (%) | |
| Right | 32 (30.8) |
| Left | 51 (49.0) |
| Bilateral | 21 (20.2) |
| IHDI grade, n (%) | |
| III | 65 (52.0) |
| IV | 60 (48.0) |
| Age at CR (months), mean [range] | 18.3 [9–32] |
| Duration of follow-up (months), mean [range] | 50.2 [24–89] |
| Type of osteotomy, n (%) | |
| Pemberton | 1 (3.2) |
| Salter | 27 (87.1) |
| Salter + femoral | 3 (9.7) |
| Age at osteotomy (months), mean [range] | 54.9 [39–79] |
IHDI, International Hip Dysplasia Institute; CR, closed reduction.
Table 2
| Grade | Description | No. of hips |
|---|---|---|
| I | Normal appearance | 4 |
| II | Mild deformity of femoral head and neck or acetabulum | 29 |
| III | Dysplasia or moderate deformity of femoral head and neck or acetabulum, or both | 88 |
| IV | Subluxation of the femoral head | 4 |
| V | Articulation of the femoral head with a false acetabulum | 0 |
| VI | Redislocation | 0 |
Table 3
| AI at CR (°) | Age at CR (months) | Sex† (male/female) | Side† (left/right) | IHDI† (III/IV) | TSL† (yes/no) | |
|---|---|---|---|---|---|---|
| RAD | 39.1±4.0 | 18.7±4.0 | 4/29 | 53/39 | 43/49 | 17/75 |
| Non-RAD | 36.7±4.7 | 17.1±3.3 | 10/82 | 19/14 | 22/11 | 17/16 |
| P | 0.006 | 0.035 | 0.845 | 0.997 | 0.049 | 0.000 |
†, No. of hips. AI, acetabular index; IHDI, International Hip Dysplasia Institute; CR, closed reduction; TSL, teardrop and sourcil line; RAD, residual acetabular dysplasia.
Table 4
| Variables | β | χ2 | P | OR | 95% CI for OR |
|---|---|---|---|---|---|
| AI at CR | 0.135 | 5.653 | 0.017 | 1.145 | 1.024–1.280 |
| Age at CR | 0.099 | 1.925 | 0.165 | 1.105 | 0.960–1.271 |
| IHDI grade | −0.776 | 2.291 | 0.130 | 0.460 | 0.169–1.257 |
| TSL | −1.540 | 10.178 | 0.001 | 0.214 | 0.083–0.552 |
AI, acetabular index; IHDI, International Hip Dysplasia Institute; CR, closed reduction; TSL, teardrop and sourcil line; RAD, residual acetabular dysplasia.

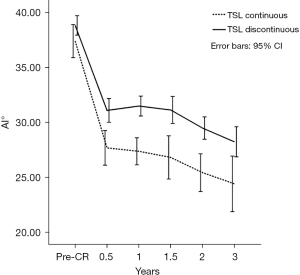
There were 34 hips that displayed continuous TSL. The mean time when TSL became continuous after CR was 20.9±11.8 months (range, 8–57 months). There were no significant differences in AI, age, gender, location or IHDI grade at CR between the TSL continuous group and TSL discontinuous group (Table 5). However, the decrease in AI, especially 6 months post-CR, was faster and the mean values of AI after CR at different time points were lower in the TSL continuous group (P<0.05) (Figure 3). The TSL continuous group had a lower incidence of RAD than the TSL discontinuous group (P<0.001) (Table 5). In the TSL continuous group, there was no significant difference in the time when TSL became continuous after CR between RAD and non-RAD hips (19.5±8.3 vs. 22.4±14.6 months, P=0.485). An ostotomy was performed in 31 hips, the TSL of 87% (27/31) hips pre-operation were displayed discontinuous, and 74% (20/27) became continuous post-operation (Figure 4), all hips developed without RAD (severin grade I: 7 hips, severin grade II: 24 hips).
Table 5
| TSL | AI at CR (°) | Age at CR (months) | Sex† (male/female) | Side† (left/right) | IHDI† (III/IV) | RAD† (yes/no) |
|---|---|---|---|---|---|---|
| Continuous | 37.4±4.3 | 17.5±2.9 | 6/28 | 19/15 | 16/18 | 17/17 |
| Discontinuous | 38.9±4.3 | 18.6±4.2 | 8/83 | 53/38 | 49/42 | 75/16 |
| p | 0.100 | 0.170 | 0.162 | 0.812 | 0.499 | 0.000 |
†, No. of hips. AI, acetabular index; IHDI, International Hip Dysplasia Institute; CR, closed reduction; TSL, teardrop and sourcil line; RAD, residual acetabular dysplasia.

Discussion
RAD represents one of the most frequent causes of secondary osteoarthritis of the hip and is not rare in DDH patients. More than one-third of DDH patients treated with CR have an outcome of RAD, and there is a higher prevalence of RAD with increasing age at reduction. In our study the incidence of RAD was 73.6% (92/125), higher than reported in previous studies (9,12,26). This might be the result of the shorter follow-up time (44.2±14.5 months) and older age (18.3±3.9 months) of the cohort at CR.
RAD is often asymptomatic and the diagnosis relies on radiography. Several radiographic parameters such as AI, CEA, centre-head distance discrepancy (CHDD) and Reimer’s index (RI) have been investigated for predicting RAD. However, there are some disadvantages to those parameters: the measurements of CEA, CHDD and RI are influenced by the shape of the femoral head and the center of the femoral head must be identified precisely. If the ossific nucleus of the femoral head has not appeared, is irregular or is very small, the measurement is unreliable. In addition, CEA is validated for patients aged ≥4 years and CHDD is useless in bilateral cases (11,12).
AI is one of the most popular parameters for predicting RAD (9,18), and a multi-center study suggested that AI would be the best predictor (12). The measurement of AI is based on a horizontal Hilgenreiner line that runs through the triradiate cartilage and a line extending from the superolateral margin of the triradiate cartilage to the most lateral ossified margin of the acetabulum. However, the Hilgenreiner line is difficult to measure after ossification of the triradiate cartilage when the patient is older than 8 years, and it is difficult to mark the exact lateral bony margin of the acetabulum because of irregular and indistinct bony shadows on radiographs of dysplastic hips. Furthermore, the value of AI can be affected by the position in which the radiograph was taken, and it is difficult to keep an uncooperative child in the correct position for the radiograph. With increasing lumbar lordosis, which corresponds to the extent of pelvic extension, the AI increases, and with decreasing lordosis or pelvic flexion, the AI decreases. Similarly, if the pelvis is rotated about the longitudinal body axis, the AI toward the side of the rotation decreases and the AI on the opposite side increases (23). It is often necessary to follow-up the AI for a long time to decide when to initiate the following procedure because the development of the acetabulum is a long and slow process. The surgeon needs an earlier and more definitive index to help determine when to carry out the next step of treatment to promote the development of the hip.
Considering the limitations of singular prognosticating factors, Kim et al. (11) tried to combine the orientation of the sourcil and CHDD to predict the RAD and created a risk scale. However, a limitation to this approach has been raised in that CHDD is only useful in unilateral cases (26).
The acetabular teardrop is a landmark seen in the inferior medial acetabulum on the AP X-ray of the pelvis. The timing of its appearance and configuration of the teardrop have been correlated with various pediatric hip disorders and could predict the outcome of DDH after CR (19-22). The sourcil is a curved area of dense bone on the weight-bearing surface of the acetabulum and represents a stress distribution within the hip joint indirectly. In a normal hip, the sourcil is uniformly thick and semilunar in shape, with a horizontal or downward orientation. However, in the dysplastic hip, the orientation of the sourcil is upward, suggesting an uneven distribution of stress within the hip joint. The shape and orientation of the sourcil have also been used to predict RAD (11,23).
In this study, we tried to find a more reliable and easier parameter to measure. TSL is the curve that makes up the lateral margin of the teardrop and the curve of the sourcil. The results showed that a continuous TSL can be a predictor of RAD (P=0.001). Compared to CHDD, CEA, RI and AI, TSL is not influenced by the shape of femoral head, does not require identification of the exact point at the center of the femoral head and the lateral bony margin of the acetabulum, and can be used in bilateral cases. The improvement of AI post-reduction by a certain age is a reliable predictive factor of the need for later acetabuloplasty (11), and many studies have focused on the cutoff values of AI at different time points post-reduction to predict RAD (9,12,18). In this study, there was no significant difference in the initial AI between the TSL continuous group and discontinuous group, but the level of AI after CR was lower in the TSL continuous group. This meant AI was more likely to become normal in the TSL continuous group and TSL could predict the potential of AI improvement after CR. However, in the TSL continuous group, there was no significant difference between RAD and non-RAD hips at the time point when TSL became continuous after CR (19.5±8.3 vs. 22.4±14.6 months, P=0.485). Unlike other parameters, there is not a cutoff value of the time when TSL becomes continuous after CR that determines progression to RAD.
Acetabular osteotomy for RAD was to decrease the AI and to improve the containment of femoral head, however, it’s difficult for junior surgeon to control the specific improvement of AI and containment intra-operation. In this study, the TSL of 74% (20/27) hips became continuous after osteotomy surgery, and all hips developed without RAD, so it indicated that restore the continuous of TSL maybe an indicator of successful osteotomy and much easier for surgeons to control, but further study is needed. However, there is no consensus on indicator of osteotomy for RAD, especially in cases of borderline dysplasia. In adult hips research shows that Femoro-Epiphyseal Acetabular Roof (FEAR) index could evaluate indication for surgery in borderline dysplasia (27). In children, long-term follow-up for the cases of borderline dysplasia is needed.
The present study had limitations. It was a single center retrospective study, the number of patients was small and the follow-up time was short. Theoretically, there is an upper time limit for TSL becoming continuous after CR that would predict whether RAD occurs or not, but we did not find such a cutoff value in this study. More patients and longer follow-up will be needed in order to further analyze the effectiveness of TSL as a predictive factor.
In conclusion, compared to other parameters, TSL is more visual, easier to measure and useful in bilateral cases. Hence, we suggest that TSL can be a predictor of RAD in DDH after CR and restore the continuous of TSL maybe a potential parameter that can help surgeons to make a judgment intra-operation.
Acknowledgments
We would like to thank David Cushley for his help in polishing our paper.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-21-401/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-21-401/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-21-401/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Children’s Hospital of Fudan University Ethics Committee (No. 2015181) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shipman SA, Helfand M, Moyer VA, et al. Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics 2006;117:e557-76. [Crossref] [PubMed]
- Cooper AP, Doddabasappa SN, Mulpuri K. Evidence-based management of developmental dysplasia of the hip. Orthop Clin North Am 2014;45:341-54. [Crossref] [PubMed]
- Sharpe P, Mulpuri K, Chan A, et al. Differences in risk factors between early and late diagnosed developmental dysplasia of the hip. Arch Dis Child Fetal Neonatal Ed 2006;91:F158-62. [Crossref] [PubMed]
- Gul R, Coffey JC, Khayyat G, et al. Late presentation of developmental dysplasia of the hip. Ir J Med Sci 2002;171:139-40. [Crossref] [PubMed]
- Walter SG, Bornemann R, Koob S, et al. Closed Reduction as Therapeutic Gold Standard for Treatment of Congenital Hip Dislocation. Z Orthop Unfall 2020;158:475-80. [Crossref] [PubMed]
- Druschel C, Placzek R, Selka L, et al. MRI evaluation of hip containment and congruency after closed reduction in congenital hip dislocation. Hip Int 2013;23:552-9. [Crossref] [PubMed]
- Walter SG, Endler CH, Remig AC, et al. Risk factors for failed closed reduction in dislocated developmental dysplastic hips. Int Orthop 2020;44:2343-8. [Crossref] [PubMed]
- Morris WZ, Hinds S, Worrall H, et al. Secondary Surgery and Residual Dysplasia Following Late Closed or Open Reduction of Developmental Dysplasia of the Hip. J Bone Joint Surg Am 2021;103:235-42. [Crossref] [PubMed]
- Albinana J, Dolan LA, Spratt KF, et al. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br 2004;86:876-86. [Crossref] [PubMed]
- Farsetti P, Caterini R, De Maio F, et al. Tönnis triple pelvic osteotomy for the management of late residual acetabular dysplasia: mid-term to long-term follow-up study of 54 patients. J Pediatr Orthop B 2019;28:202-6. [Crossref] [PubMed]
- Kim HT, Kim JI, Yoo CI. Acetabular development after closed reduction of developmental dislocation of the hip. J Pediatr Orthop 2000;20:701-8. [Crossref] [PubMed]
- Li Y, Guo Y, Li M, et al. Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. Int Orthop 2018;42:631-40. [Crossref] [PubMed]
- Zhang ZL, Fu Z, Yang JP, et al. Intraoperative Arthrogram Predicts Residual Dysplasia after Successful Closed Reduction of DDH. Orthop Surg 2016;8:338-44. [Crossref] [PubMed]
- Takeuchi R, Kamada H, Mishima H, et al. Evaluation of the cartilaginous acetabulum by magnetic resonance imaging in developmental dysplasia of the hip. J Pediatr Orthop B 2014;23:237-43. [Crossref] [PubMed]
- Wakabayashi K, Wada I, Horiuchi O, et al. MRI findings in residual hip dysplasia. J Pediatr Orthop 2011;31:381-7. [Crossref] [PubMed]
- Zamzam MM, Kremli MK, Khoshhal KI, et al. Acetabular cartilaginous angle: a new method for predicting acetabular development in developmental dysplasia of the hip in children between 2 and 18 months of age. J Pediatr Orthop 2008;28:518-23. [Crossref] [PubMed]
- Miyake T, Tetsunaga T, Endo H, et al. Predicting acetabular growth in developmental dysplasia of the hip following open reduction after walking age. J Orthop Sci 2019;24:326-31. [Crossref] [PubMed]
- Gotoh E, Tsuji M, Matsuno T, et al. Acetabular development after reduction in developmental dislocation of the hip. Clin Orthop Relat Res 2000;174-82. [Crossref] [PubMed]
- Bowerman JW, Sena JM, Chang R. The teardrop shadow of the pelvis: anatomy and clinical significance. Radiology 1982;143:659-62. [Crossref] [PubMed]
- Kahle WK, Coleman SS. The value of the acetabular teardrop figure in assessing pediatric hip disorders. J Pediatr Orthop 1992;12:586-91. [Crossref] [PubMed]
- Erkula G, Celikbas E, Kilic BA, et al. The acetabular teardrop and ultrasonography of the hip. J Pediatr Orthop B 2004;13:15-20. [PubMed]
- Smith JT, Matan A, Coleman SS, et al. The predictive value of the development of the acetabular teardrop figure in developmental dysplasia of the hip. J Pediatr Orthop 1997;17:165-9. [Crossref] [PubMed]
- Kim HT, Kim JI, Yoo CI. Diagnosing childhood acetabular dysplasia using the lateral margin of the sourcil. J Pediatr Orthop 2000;20:709-17. [Crossref] [PubMed]
- Morbi AH, Carsi B, Gorianinov V, et al. Adverse Outcomes in Infantile Bilateral Developmental Dysplasia of the Hip. J Pediatr Orthop 2015;35:490-5. [Crossref] [PubMed]
- Narayanan U, Mulpuri K, Sankar WN, et al. Reliability of a New Radiographic Classification for Developmental Dysplasia of the Hip. J Pediatr Orthop 2015;35:478-84. [Crossref] [PubMed]
- Mansour E, Eid R, Romanos E, et al. The management of residual acetabular dysplasia: updates and controversies. J Pediatr Orthop B 2017;26:344-9. [Crossref] [PubMed]
- Wyatt M, Weidner J, Pfluger D, et al. The Femoro-Epiphyseal Acetabular Roof (FEAR) Index: A New Measurement Associated With Instability in Borderline Hip Dysplasia? Clin Orthop Relat Res 2017;475:861-9. [Crossref] [PubMed]


