
Outcomes and experience after open reduction for chronic Monteggia fracture in children
Introduction
Monteggia fracture-dislocation, first described by Giovanni Monteggia in 1814, is a fracture of the ulna associated with dislocation of the radiocapitellar joint and disruption of the proximal radioulnar joint (1). When the Monteggia lesion is identified in an acute situation, the outcomes are always achieved well. However, many of these injuries in children are chronic at initial presentation, for inadequate radiographs, missing subtle greenstick fractures of the ulna and bowing of the ulna (2). The neglected lesion's common presentation is bony prominence, limited range of motion (ROM), valgus deformity of the elbow, with or without elbow pain, limited supination and pronation of the forearm, and neurological problems (3-6).
The treatment of chronic Monteggia fracture-dislocation (CMF) in children remains controversial and challenging for surgeons. However, in the last years, most orthopedists recommended that surgical treatment is the best option for skeletally immature children. Many surgery options have been reported, such as closed or open reduction of the radial head; whether the annular ligament is reconstructed, if required, what materials will be used; and different osteotomy ways of the ulna, the different fixation methods (7-9). Although most authors reported improved outcomes after surgery, the rate of complications and recurrent instability is the common frustrating challenges. There are many factors that correlated with the therapeutic effect. Currently, the recognized factors related to postoperative elbow performance include age, interval, the presence of deformity of ulna, and degree of neck-shaft angle asymmetry (10). The basic pathological state in CMF is the mismatches of radius and ulna, our team reported the proportional ulnar length (PUL), defined as the length of the ulna/length of the radius, consistently averaged approximately 1.1 in healthy children (11). Therefore, we decided to compare the pre-op PUL to the final follow-up PUL, trying to reveal the proportional change of ulna and radius in CMF for the first time and to evaluate it as useful parameter in preoperative planning. Furthermore, we would like to report our surgical experience from clinical and radiographic findings. We present the following article in accordance with the STROBE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-21-614/rc).
Methods
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The patient’s family members were aware of and agreed to this study, and signed the relevant informed consent. The study was approved by Children’s Hospital of Fudan University Ethics Committee (No. 2020528).
Patients
A retrospective review was performed on patients diagnosed with CMF from January 2008 to May 2019. The inclusion criteria were: (I) more than one month after trauma; (II) no treatment history; (III) at least 2 years of follow-up. Children with bone tumors, secondary radial head dislocation, congenital diseases, and fresh or subacute injury were excluded.
Clinical characteristics
The mean age at the time of surgery and the mean interval from trauma to surgery was calculated. The clinical data of Bado type (12), complaints before the operation, pre-and post-operational Kim score (10), complications, and reduction status were collected.
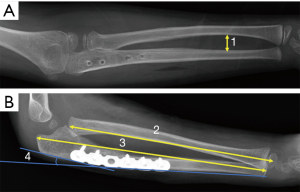
The final reduction status of the radial head was divided into three categories: good (complete reduction without osteolytic change), fair (reduction with subluxation or osteolytic change), or poor (radial head dislocation) (7). The radiological parameters of maximum interosseous distance (MID) from anteroposterior view (appropriate orientation to observe the interosseous membrane), pre-and post-operative PUL from a lateral view (11), lengthening of the ulna (the biggest distance between the two sites of osteotomy after the ulnar lengthening) and the bending angle of the ulna from a lateral view was summarized (Figure 1). The relationship between the lengthening and angulation of ulna and the interval was calculated.
Treatment procedure
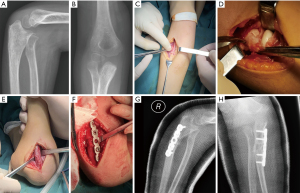
The surgeries were performed under general anesthesia. A 3 to 4 cm incision was made to access the necessary structures. The radial nerve was identified, depressed, and protected. Then, the elbow joint was opened, the radial head was exposed, and the state of the radial head and the annular ligament were assessed. Reduce the ligament if it exists and complete; excise it without reconstruction if impedes reduction of the radial head. Another 4 to 6 cm incision was achieved to have a proximal ulnar osteotomy. The bending angle and the elongation distance of the ulna were confirmed by the reduction of the radial head by means of direct observation (flexion, extension, supination, pronation). Inserting an autogenous cancellous iliac crest bone graft at the ulnar osteotomy site. Then 5- or 6-hole plate was placed at the lateral (or medial) side instead of backside of ulna (Figure 2). The limb was placed into a long-arm cast, with the elbow in 90 to 100 degrees of flexion and the forearm in supination. Cast immobilization was maintained for 6 weeks, then, the exercises were initiated. Six months later, after the ulnar union, removed the implant.
Statistical analysis
The Kolmogorov-Smirnov test analyzed the continuous variable to assess for normality. Continuous variables were collected as the mean ± SD. Categorical data were analyzed with the χ2 test. Comparisons of two groups in terms of PUL, MID, and Kim scores were performed by paired-t-test. The Spearman nonparametric correlation test was used for correlation comparison (The interval and the lengthening of ulna; The interval and the bending angle of ulna; The lengthening and the bending angle of ulna). Two single doctors independently measured and collected all data. The level of significance for all statistical tests was P<0.05. Statistical analysis was performed using SPSS 19.0 (IBM, America).
Results
Eighteen patients, 15 boys (83.33%) and 3 girls (16.67%), were included. There were 11 right-sided injuries (61.11%). The mean age at initial treatment was 6.78±2.67 years old, ranging from 4 to 13 years old. The interval was 11.14±15.74 months, ranging from 1 to 48 months. The follow-up time was 46.58±23.33 months (range, 24–96 months). According to Bado classification, all patients were classified as type I. The most prominent complaints were cosmetic problems and limited ROM (Table 1).
Table 1
| Characteristics | Data |
|---|---|
| Sex, n (%) | |
| Male | 15 (83.33) |
| Female | 3 (16.67) |
| Side, n (%) | |
| Left | 7 (38.89) |
| Right | 11 (61.11) |
| Complains, n (%) | |
| Bony prominence | 10 (55.56) |
| Limited range of motion | 15 (83.33) |
| Pain | 5 (27.78) |
| Valgus deformity | 3 (16.67) |
| Neurological problems | 2 (11.11) |
| Follow-up time* (mth) | 46.58 [24–96] |
| Complications, n (%) | |
| Nonunion | 3 (16.67) |
*, the values are given as the mean, with the range in parentheses.
The details of the reconstructions were showed in Table 2. The annular ligaments were repositioned in 8 (44.44%) patients, while 10 (55.56%) patients had excised scar tissues without any reconstruction. Notably, three patients with a mean ulnar lengthening of 1.52 cm and mean angulation of 22.54° had observed nonunion after more than 6 months of follow-up. Then, reoperation and autogenous cancellous iliac crest bone graft insertion was performed. Eventually, the osteotomy site healed well. Two patients had the symptom of radial nerve issues and recovered several months later after surgery. A good reduction was observed in 15 (83.33%) patients, while 3 (16.67%) patients were fair. The mean posterior bending angle was 12.88° (range, 3 to 25°), and the mean amount of elongation of the ulna was 8.78 mm (range, 3.61 to 17.52 mm) (Table 3). The relationship between the lengthening, angulation of ulna, and the interval was seen in Table 4 and Figure 3. The lengthening of the ulna was significantly proportional to the magnitude of angulation of the ulna (r=0.648, P=0.004), and a positive correlation was also seen between the lengthening and the interval (r=0.632, P=0.005) and the angulation of ulna and the interval (r=0.502, P=0.034). The PUL and MID were significantly increased respectively from pre-operation (1.06±0.03 and 1.11±0.26) to the last follow-up (1.13±0.11 and 1.28±0.27). Postoperatively, the Kim scores were improved, from 59.17±18.17 to 90±6.64 (Table 5).
Table 2
| Characteristics | Data |
|---|---|
| Age* (y) | 6.78 [4–13] |
| Interval* (month) | 11.14 [1–48] |
| Annular ligament, n (%) | |
| Excised scar tissue | 10 (55.56) |
| Reposition | 8 (44.44) |
| Ulnar osteotomy, n (%) | |
| Proximal site | 18 (100.00) |
| Bone graft, n (%) | |
| Iliac | 14 (77.78) |
| Allograft | 4 (22.22) |
*, the values are given as the mean, with the range in parentheses.
Table 3
| Characteristics | Data |
|---|---|
| Bado classification, n (%) | |
| I | 18 (100.00) |
| Final reduction status, n (%) | |
| Good | 15 (83.33) |
| Fair | 3 (16.67) |
| Arthrosis, n (%) | 0 (0) |
| Lengthening* (mm) | 8.78 [3.61–17.52] |
| Osteotomy angle* (°) | 12.88 [3–25] |
*, the values are given as the mean, with the range in parentheses.
Table 4
| Variables | Correlation coefficient | P value |
|---|---|---|
| Lengthening & time interval | 0.632 | 0.005 |
| Bending angle & time interval | 0.502 | 0.034 |
| Bending angle & lengthening | 0.648 | 0.004 |
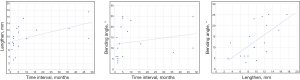
Table 5
| Variables | Preop.* | Last follow-up* | Difference | 95% CI | P value |
|---|---|---|---|---|---|
| PUL | 1.06±0.03 | 1.13±0.11 | −0.07 | −0.03 to 0.00 | 0.047 |
| MID | 1.11±0.26 | 1.28±0.27 | −0.17 | −0.32 to −0.03 | 0.021 |
| Kim scores | 59.17±18.17 | 90±6.64 | −35.83 | −45.86 to −25.81 | 0.000 |
*, the values are given as the mean and the standard deviation. PUL, proportional ulnar length; MID, maximum interosseous distance.
Discussion
Great difficulty and more failures were the descriptions of a CMF. A great advance has been witnessed recently, focusing on exploring the better surgery reduction outcome; however, the consensus has never been made about a perfect protocol procedure to achieve satisfactory results. Our surgical procedure is based on the hypothesis that ulnar osteotomy plays the most crucial role in achieving stable radial head reduction, and all 18 children achieved satisfied outcomes (Kim scores). Hence, we introduced our experience in the treatment of CMF in children and evaluated outcomes from clinical and radiographic findings, especially using the PUL parameter for the first time.
Corrective ulnar osteotomy and relocating the radial head into the intact annular ligament can be safely used to prevent radial head and capitellum deformity (13). More controversial, however, is the condition of annular ligament damage. The ligament reconstruction technique was changed a lot and was controversial. Some literature had investigated the outcomes by comparing annular ligament reconstruction or without it, no consensus was found (14,15). Some authors agreed that the annular ligament and associated anterior capsular structures become a block to anatomic reduction when manual reduction (6,16-18), so open reduction is recommended. In our research, open reduction of the radial head with remnant annular ligament repositioning or without ligament repairing was performed. However, the maintenance of this reduction should be achieved by optical ulnar osteotomy and enough lengthening.
Although a review containing thirty studies with 600 patients showed that proximal ulnar osteotomies (P=0.016) were the most significant predictors for the eventual reduction of the radial head (19), several issues should be addressed about ulnar osteotomy. The first one is the position of the osteotomy. Center of rotation angulation (CORA) and proximal part of ulnar metaphysis were the most mentioned position for osteotomy. However, the nonunion or delayed union problem was more prominent at the CORA site (20,21). Ulnar malunion was also blamed for the difficulty of the radial head reduction (20). Moreover, a proximal osteotomy was recommended for having an unnoticeable posterior curvature and avoiding forearm rotation restriction because the whole interosseous membrane (IOM) remains constant (14). The second issue is quantitative ulnar elongation and posterior bending angle. From our data, the more lengthening, the more angulation was needed. Three patients failed the reduction having an insufficient lengthening or angulation. Then, we ameliorated the technique based on the value of PUL, we concluded that the lengthening of the ulna larger than the normal PUL was warranted. An open wedge angle proportional to the elongation was also needed, which allows for a stable reduction of the radial head in flexion, extension, pronation, and supination. In this way, the outcomes turn out well. This kind of osteotomy not only leaves room for the radial head reduction but also tensions the IOM against forces that would lead to recurrent radial head dislocation (4,22).
The IOM has been reported to play an important role in the longitudinal and transverse stability of the forearm (23). The recommended osteotomy on the proximal side also maintains the IOM’s stouter distal fibers, better translating ulnar correction to the intact radius (24). Soubeyrand et al. (23) describes this structure as the middle radioulnar joint, which is a fibrous joint, allowing pronosupination and ensuring forearm stability. From our research, the obvious difference in MID between pre-operation with the final follow-up of these successful cases also explained the functional effect of IOM. As for the challenging patients with unstable radial head after the scar tissue is dissected and the elongation and angulation of ulna are finished, we might increase supination slightly, and then, the radial head was reduced. This fact highlights the crucial role played by the IOM in forearm stability.
After osteotomy, different internal or external fixation was reported to fix the ulna (14,25-28). Dukan et al. described the possibility of using an external fixator intraoperatively to facilitate the various steps of the procedure and achieved good outcomes (29). Nowadays, rigid fixation with plate is more accepted, allowing for a post-operative ROM, minimizing contracture. We modified the technique by putting the plate into the ulnar lateral or medial side instead of the backside. First, it could diminish the stress applied to the plate without plate bending, which reduces the risk of plate breakage. Second, it is more aesthetic and comfortable for patients because the palpable pain or bump will vanish.
In addition to surgery, several factors can affect the prognosis of the disease. Ko et al. recommended that over the skeletal ages of 14 years in boys and 11.5 years in girls, reconstructive surgery must be cautiously indicated and the interval of ≤7 months will have good results after surgery (30). In this study, we found no correlation between age and prognosis, which may be related to the younger average age of our research. In addition, we found that the interval was positively correlated with the angulation and lengthening of the ulna, which may increase the difficulty of surgery and the occurrence of postoperative complications.
The present study had limitations. First, this is a retrospective study to evaluate PUL’s value in the treatment of CMF, however, this is the first to bring up this reference; more randomized controlled trials or prospective studies are required for further validation. Second, all patients need longer follow-ups to confirm if there are any delayed redislocation.
In conclusion, we emphasize the importance of ulnar osteotomy to obtain and maintain the reduction of the radiocapitellar joint in CMF by addressing both length and angular. With the extension of the interval, it is more necessary to increase the lengthening and angulation of the ulna in positive proportion. Enough elongation to at least normal PUL and balanced angulation of the osteotomy is warranted to keep satisfactory outcomes. It is more aesthetic and safer to put the plate into the lateral or medial side of the ulna. The functional effect of IOM cannot be neglected during the surgeries.
Acknowledgments
Funding: The project was sponsored by Shanghai Shenkang Clinical Research Cultivation Project (2019) (No. SHDC12019X28), Natural Science Foundation of Shanghai (No. 20Y11912900) and the Clinical Center of Birth Defects (No. EK2022ZX03) of Children’s Hospital of Fudan University.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-21-614/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-21-614/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-21-614/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The patient’s family members were aware of and agreed to this study, and signed the relevant informed consent. The study was approved by Children’s Hospital of Fudan University Ethics Committee (No. 2020528).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ring D, Waters PM. Operative fixation of Monteggia fractures in children. J Bone Joint Surg Br 1996;78:734-9. [Crossref] [PubMed]
- Fowles JV, Sliman N, Kassab MT. The Monteggia lesion in children. Fracture of the ulna and dislocation of the radial head. J Bone Joint Surg Am 1983;65:1276-82. [Crossref] [PubMed]
- Rodgers WB, Waters PM, Hall JE. Chronic Monteggia lesions in children. Complications and results of reconstruction. J Bone Joint Surg Am 1996;78:1322-9. [Crossref] [PubMed]
- Inoue G, Shionoya K. Corrective ulnar osteotomy for malunited anterior Monteggia lesions in children. 12 patients followed for 1-12 years. Acta Orthop Scand 1998;69:73-6. [Crossref] [PubMed]
- Eamsobhana P, Chalayon O, Kaewpornsawan K, et al. Missed Monteggia fracture dislocations treated by open reduction of the radial head. Bone Joint J 2018;100-B:1117-24. [Crossref] [PubMed]
- Hubbard J, Chauhan A, Fitzgerald R, et al. Missed Pediatric Monteggia Fractures. JBJS Rev 2018;6:e2. [Crossref] [PubMed]
- Nakamura K, Hirachi K, Uchiyama S, et al. Long-term clinical and radiographic outcomes after open reduction for missed Monteggia fracture-dislocations in children. J Bone Joint Surg Am 2009;91:1394-404. [Crossref] [PubMed]
- Park H, Park KW, Park KB, et al. Impact of Open Reduction on Surgical Strategies for Missed Monteggia Fracture in Children. Yonsei Med J 2017;58:829-36. [Crossref] [PubMed]
- Miller TC, Fishman FG. Management of Monteggia Injuries in the Pediatric Patient. Hand Clin 2020;36:469-78. [Crossref] [PubMed]
- Kim HT, Park BG, Suh JT, et al. Chronic radial head dislocation in children, Part 2: results of open treatment and factors affecting final outcome. J Pediatr Orthop 2002;22:591-7. [Crossref] [PubMed]
- Huang P, Zhu L, Ning B. Forearm Deformity and Radial Head Dislocation in Pediatric Patients with Hereditary Multiple Exostoses: A Prospective Study Using Proportional Ulnar Length as a Scale to Lengthen the Shortened Ulna. J Bone Joint Surg Am 2020;102:1066-74. [Crossref] [PubMed]
- Bado JL. The Monteggia lesion. Clin Orthop Relat Res 1967;71-86. [PubMed]
- Baydar M, Öztürk K, Orman O, et al. Use of Corrective Ulnar Osteotomy and Radial Head Relocation Into Preserved Annular Ligament in the Treatment of Radiocapitellar Instability Secondary to Pediatric Chronic Monteggia Fracture-Dislocation. J Hand Surg Am 2022;47:481.e1-9. [Crossref] [PubMed]
- Rahbek O, Deutch SR, Kold S, et al. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J Child Orthop 2011;5:449-57. [Crossref] [PubMed]
- Soni JF, Valenza WR, Matsunaga CU, et al. CHRONIC MONTEGGIA FRACTURE-DISLOCATION IN CHILDREN SURGICAL STRATEGY AND RESULTS. Acta Ortop Bras 2019;27:244-7. [Crossref] [PubMed]
- Kim HT, Conjares JN, Suh JT, et al. Chronic radial head dislocation in children, Part 1: pathologic changes preventing stable reduction and surgical correction. J Pediatr Orthop 2002;22:583-90. [Crossref] [PubMed]
- Wilkins KE. Changes in the management of monteggia fractures. J Pediatr Orthop 2002;22:548-54. [Crossref] [PubMed]
- Bhaskar A. Missed Monteggia fracture in children: Is annular ligament reconstruction always required? Indian J Orthop 2009;43:389-95. [Crossref] [PubMed]
- Tan SHS, Low JY, Chen H, et al. Surgical Management of Missed Pediatric Monteggia Fractures: A Systematic Review and Meta-Analysis. J Orthop Trauma 2022;36:65-73. [Crossref] [PubMed]
- Lädermann A, Ceroni D, Lefèvre Y, et al. Surgical treatment of missed Monteggia lesions in children. J Child Orthop 2007;1:237-42. [Crossref] [PubMed]
- Wang MN, Chang WN. Chronic posttraumatic anterior dislocation of the radial head in children: thirteen cases treated by open reduction, ulnar osteotomy, and annular ligament reconstruction through a Boyd incision. J Orthop Trauma 2006;20:1-5. [Crossref] [PubMed]
- Song KS, Ramnani K, Bae KC, et al. Indirect reduction of the radial head in children with chronic Monteggia lesions. J Orthop Trauma 2012;26:597-601. [Crossref] [PubMed]
- Soubeyrand M, Wassermann V, Hirsch C, et al. The middle radioulnar joint and triarticular forearm complex. J Hand Surg Eur Vol 2011;36:447-54. [Crossref] [PubMed]
- Horii E, Nakamura R, Koh S, et al. Surgical treatment for chronic radial head dislocation. J Bone Joint Surg Am 2002;84:1183-8. [Crossref] [PubMed]
- David-West KS, Wilson NI, Sherlock DA, et al. Missed Monteggia injuries. Injury 2005;36:1206-9. [Crossref] [PubMed]
- Lu X, Kun Wang Y, Zhang J, et al. Management of missed Monteggia fractures with ulnar osteotomy, open reduction, and dual-socket external fixation. J Pediatr Orthop 2013;33:398-402. [Crossref] [PubMed]
- Yuan Z, Xu HW, Liu YZ, et al. The use of external fixation for the management of acute and chronic Monteggia fractures in children. J Child Orthop 2019;13:551-9. [Crossref] [PubMed]
- Bor N, Rubin G, Rozen N, et al. Chronic anterior monteggia lesions in children: report of 4 cases treated with closed reduction by ulnar osteotomy and external fixation. J Pediatr Orthop 2015;35:7-10. [Crossref] [PubMed]
- Dukan R, Le Hanneur M, Pannier S, et al. Use of an external fixator during one-step surgical management of missed chronic Monteggia injuries. Orthop Traumatol Surg Res 2022;108:102963. [Crossref] [PubMed]
- Ko KR, Shim JS, Park J, et al. Predictors of ideal outcomes after reconstructive surgery for chronic Monteggia fracture in children. J Orthop Sci 2021; [Epub ahead of print]. [Crossref] [PubMed]


