
Construction and validation of an early prediction model of delirium in children after congenital heart surgery
Introduction
Congenital heart disease has ranked first for birth defects in China (1). Surgery is an important means for treating congenital heart disease. However, the incidence of postoperative delirium, which mostly occurs within 48 hours of surgery, is 40–66% (2-4). Pediatric delirium, which has been historically underdiagnosed or misdiagnosed (5), can lead to prolonged mechanical ventilation and hospitalization, affect prognosis, increase medical and healthcare costs (2,6,7), and also cause long-term effects. Although the short-term course of delirium has been recorded, the long-term sequelae has not been fully clarified (8). The long-term effects are particularly worrying in children as they require growth and development in addition to rehabilitation. Therefore, prevention has become an important topic in current clinical research.
At present, some studies have investigated the risk factors of delirium in children after cardiac surgery, the known risk factors of pediatric delirium after cardiac surgery include age, disease severity, cyanotic heart disease, dysplasia, mechanical ventilation, sedative and analgesic drugs and so on (2-4). There are no relevant reports on a prediction model of delirium in children after cardiac surgery. More and more children with congenital heart disease receive cardiac surgery every year. It is time-consuming and laborious to implement general delirium prevention measures for all children. Therefore, in view of the fact that postoperative delirium mostly occurs within 48 h, we conducted an observational study to explore the early risk factors of delirium in children after cardiac surgery and develop a prediction model in order to provide a reference for early clinical identification of high-risk groups and the implementation of efficient prevention and management. We present the following article in accordance with the TRIPOD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-187/rc).
Methods
Patient selection
A total of 362 children transferred to the cardiac intensive care unit (CICU) after congenital heart surgery at Shanghai Children’s Medical Center between February 15 and April 15, 2021 were prospectively enrolled in the study using convenience sampling for construction of model, another 96 children enrolled from April 16 and May 15, 2021 for validation of model. The inclusion criteria were: (I) children ≤8 years old without disposing capacity and with informed consent of their parents, (II) length of stay in the CICU ≥12 h, (III) Richmond Agitation-Sedation Scale (RASS) score between −3 and 4 at least once during CICU hospitalization, and (IV) complete medical records and willingness to cooperate with the study. The exclusion criteria were: (I) existing psychosis or nervous system disease (excluding well-controlled epilepsy with no seizure during hospitalization), (II) eye disease, (III) myasthenia, (IV) preoperative delirium, and (V) transfer halfway or unwillingness to cooperate with the study. All patients received routine treatment without delirium prevention measures. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shanghai Children’s Medical Center (No. SCMCIRB-K2021027-1). Informed consent was taken from all the patients’ parents.
Research tools
- RASS provides a score between −5 and +4 to evaluate the degree of sedation and can be used to distinguish delirium subtypes. A score <0 indicates hypoactive delirium, >0 is considered hyperactive delirium, and a score =0 or fluctuating between positive and negative points indicates a mixed type.
- The Cornell Assessment of Pediatric Delirium (CAPD) is used to evaluate whether children have delirium. There are 8 items, with each receiving a score between 0 and 4. The fewer the symptoms and behaviors from items 1–4, the higher the score. The more symptoms and behaviors from items 5–8, the higher the score. A child with a total score >9 points is diagnosed with delirium.
- The Pediatric Risk of Mortality III (PRISM III) evaluates the severity of disease by evaluating systolic blood pressure, heart rate, temperature, pupillary reflex, mental status, total carbon dioxide (CO2) content, partial pressure of oxygen (PaO2), partial pressure of carbon dioxide (PaCO2), pH, blood glucose, creatinine, blood urea nitrogen (BUN), leukocyte count, prothrombin time (PT)/partial thromboplastin time (PTT), platelet count, and other factors on the day of operation. The higher the score, the higher the severity of the disease.
Data collection
On the basis of a literature review, 16 preoperative and intraoperative risk factors related to delirium were included in this study: gender, age, cyanotic heart disease, disease severity, basic diseases affecting function, dysplasia, delirium in the immediate family, previous occurrence of delirium or cognitive impairment in the patient, albumin on the operation day, anesthesia mode, operation time, cardiopulmonary bypass time, aortic cross-clamp time, cardiopulmonary bypass temperature, intraoperative blood transfusion, and use of cardiovascular active drugs.
Prior to commencement of the study, bedside nurses were trained in data collection methods. Except for delirium, all other data were collected within 12 h of the child being admitted to the CICU. Among them, the evaluation of disease severity was performed by the doctor, recorded in the electronic medical record system and collected by nurses. Nurses evaluated the delirium of the children at 8:00, 14:00, and 20:00 every day and at times of abnormal situations. Data were recorded until the child left the CICU.
Statistical methods
SPSS 22.0 and R3 5.1 were used for data analysis. Continuous variables are expressed as median and interquartile interval, and the Mann-Whitney test was used for comparison between 2 groups. Categorical variables are expressed as frequency and percentage, and chi square test was used for comparison. P<0.05 from the univariate analysis showed that there was significant difference between groups and it was a potential risk factor. In order to facilitate clinical use, this study obtained the cut-off value of continuous variables with statistical differences through receiver operating characteristic (ROC) curve analysis, converted the continuous variables into categorical variables, and then conducted logistic regression analysis to construct the prediction model and a nomogram was formulated based on the results of logistic regression. C-index and Brier value were used to evaluate the predictive effect of the model. The scoring method of model was applied to the validation group. The validation group evaluated the prediction efficiency of the model by comparing the predicted occurrence of delirium with the actual occurrence of delirium.
Results
Occurrence of delirium in children after cardiac surgery
A total of 379 children who had cardiac surgery were recruited for this study. Seventeen cases were excluded because they did not meet the requirements, including 15 patients with incomplete information, and 2 patients who had a RASS score lower than −3 and died. Finally, 362 children were included in the study. The incidence of delirium was 25.4% (92 of 362 children), including 30 cases of hyperactive delirium, 20 cases of hypoactive delirium, and 42 cases of mixed type. A total of 77 cases of delirium occurred within 48 h of surgery, accounting for 83.7%. Delirium in children mostly stopped within 7 days, and there was only 1 case with delirium duration ≥7 days. Among the 362 children included in the study, 1 child with delirium died. The rest were transferred to the ward after their condition improved (Table 1).
Table 1
| Delirium | Number of patients | Percentage |
|---|---|---|
| Total | 92 | 25.4% |
| Subtypes | ||
| Hyperactive | 30 | 32.6% |
| Hypomanic | 20 | 21.7% |
| Mixed | 42 | 45.7% |
| Time of occurrence (days) | ||
| ≤2 | 77 | 83.7% |
| 2–7 | 15 | 16.3% |
| >7 | 0 | 0% |
| Delirium duration (days) | ||
| ≤2 | 72 | 78.3% |
| 2–7 | 19 | 20.7% |
| >7 | 1 | 1.1% |
| Outcome | ||
| Survived | 91 | 98.9% |
| Expired | 1 | 1.1% |
Univariate analysis of delirium in children after congenital heart surgery
The children were divided into a delirium group and non-delirium group. The results of univariate analysis showed that there were significant differences between the 2 groups in gender, age, cyanotic heart disease, disease severity, dysplasia, albumin, operation time, cardiopulmonary bypass time, aortic cross-clamp time, and cardiopulmonary bypass temperature (P<0.05). The continuous variables of age, disease severity, albumin, operation time, cardiopulmonary bypass time, and aortic cross-clamp time were obtained by ROC curve analysis. The cut-off values to distinguish whether delirium occurred were age <6.5 months, disease severity ≥4 points, albumin <41.5 g/L, operation time ≥148 min, cardiopulmonary bypass time >50 min, and aortic cross-clamp time >40 min. There was no significant difference between the 2 groups with respect to basic diseases, previous delirium in the patient, anesthesia mode, intraoperative blood transfusion, and the use of cardiovascular active drugs (P>0.05, Table 2).
Table 2
| Variable | Total (n=362) | Delirium (n=92) | Non delirium (n=270) | χ2/Z | P value |
|---|---|---|---|---|---|
| Preoperative risk factors | |||||
| Gender | 9.453 | 0.007 | |||
| Male | 186 (48.6) | 60 (34.8) | 126 (53.3) | ||
| Female | 176 (51.4) | 32 (65.2) | 144 (46.7) | ||
| Age, months | 12.85 (4.95, 28.93) | 5.95 (3.23, 15.10) | 15.65 (6.45, 34.45) | −5.282 | 0.000 |
| Cyanotic heart disease | 16.243 | 0.000 | |||
| Yes | 41 (11.0) | 21 (21.7) | 20 (7.4) | ||
| No | 321 (89.0) | 71 (78.3) | 250 (92.6) | ||
| Disease severity | 3 (3.00, 3.00) | 3 (3.00, 6.00) | 3 (1.00, 3.00) | −6.618 | 0.000 |
| Basic diseases affecting function | 2.376 | 0.059 | |||
| Yes | 21 (5.8) | 8 (9.8) | 12 (4.4) | ||
| No | 341 (94.2) | 84 (90.2) | 258 (95.6) | ||
| Dysplasia | 4.423 | 0.035 | |||
| Yes | 9 (2.5) | 5 (5.4) | 4 (1.5) | ||
| No | 353 (97.5) | 87 (94.6) | 266 (98.5) | ||
| Delirium in immediate family | / | / | |||
| Yes | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| No | 362 (100.0) | 92 (100.0) | 270 (100.0) | ||
| Delirium or cognitive impairment occurred previously | 0.685 | 0.408 | |||
| Yes | 2 (0.6) | 0 (0.0) | 2 (0.7) | ||
| No | 360 (99.4) | 92 (100.0) | 268 (99.3) | ||
| Albumin | 43 (40.30, 45.40) | 41.35 (38.18, 44.90) | 43.2 (41.10, 45.60) | −2.737 | 0.006 |
| Intraoperative risk factors | |||||
| Anesthesia | 14.998 | 0.091 | |||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron + etomidate | 307 (84.8) | 71 (77.2) | 236 (87.4) | ||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron + etomidate + atropine | 1 (0.3) | 0 (0.0) | 1 (0.4) | ||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron + etomidate + lidocaine | 3 (0.8) | 1 (1.1) | 2 (0.7) | ||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron + etomidate + ropivacaine | 1 (0.3) | 0 (0.0) | 1 (0.4) | ||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron + etomidate + dexmedetomidine | 25 (6.9) | 8 (8.7) | 17 (6.3) | ||
| Sufentanil + midazolam + propofol + sevoflurane + esmeron | 1 (0.3) | 0 (0.0) | 1 (0.4) | ||
| Sufentanil + etomidate + propofol + esmeron + midazolam | 9 (2.5) | 6 (6.5) | 3 (1.1) | ||
| Sufentanil + etomidate + propofol + esmeron | 1 (0.3) | 1 (1.1) | 0 (0.0) | ||
| Sufentanil + etomidate + propofol + esmeron + sevoflurane | 14 (3.9) | 5 (5.4) | 9 (3.3) | ||
| Operation time, min | 135 (114.00, 165.00) | 150 (125.00, 190.00) | 135 (115.00, 160.00) | −3.605 | 0.000 |
| Cardiopulmonary bypass time, min | 59 (44.00, 75.75) | 65 (53.00, 100.00) | 56 (42.00, 70.50) | −4.147 | 0.000 |
| Aortic cross-clamp time, min | 32 (22.00, 46.00) | 38 (27.00, 57.50) | 30 (20.00, 44.00) | −2.745 | 0.001 |
| Cardiopulmonary bypass temperature | 14.096 | 0.007 | |||
| Normothermic | 197 (54.4) | 40 (43.5) | 157 (58.1) | ||
| Mild hypothermia | 115 (31.8) | 38 (41.3) | 77 (28.5) | ||
| Moderate hypothermia | 18 (5.0) | 9 (9.8) | 9 (3.3) | ||
| Deep hypothermia | 3 (0.8) | 0 (0.0) | 3 (1.1) | ||
| Nil | 29 (8.0) | 5 (5.4) | 24 (8.9) | ||
| Intraoperative blood transfusion | 2.845 | 0.092 | |||
| Yes | 336 (92.8) | 89 (96.7) | 247 (91.5) | ||
| No | 26 (7.2) | 3 (3.3) | 23 (8.5) | ||
| Use of cardiovascular active drugs | 1.983 | 0.159 | |||
| Yes | 339 (93.6) | 89 (96.7) | 250 (92.6) | ||
| No | 23 (6.4) | 3 (3.3) | 20 (7.4) | ||
Data are shown as number (percentage) or median (interquartile).
Multivariate analysis of delirium in children after congenital heart surgery
The risk factors with statistical significance in univariate analysis (see Table 3) were included in multivariate logistic regression analysis. The results showed that male gender, age <6.5 months, disease severity ≥4 points, and operation time ≥148 min were independent risk factors for delirium (Table 4).
Table 3
| Independent variable | Assignment |
|---|---|
| Gender | Male =1; female =0 |
| Age | <6.5 months =1; ≥6.5 months =0 |
| Cyanotic heart disease | Yes =1; no =0 |
| Disease severity | ≥4 points =1; <4 points =0 |
| Dysplasia | Yes =1; no =0 |
| Albumin | <41.5 g/L =1; ≥41.5 g/L =0 |
| Operation time | ≥148 min =1; <148 min =0 |
| Cardiopulmonary bypass time | >50 min =1; ≤50 min =0 |
| Aortic cross-clamp time | >40 min =1; ≤40 min =0 |
| Cardiopulmonary bypass temperature | Nil =0; normothermic =1; mild hypothermia =2; moderate hypothermia =3; deep hypothermia =4 |
Table 4
| Variable | β value | Standard error | Wald | OR (95% CI) | P value |
|---|---|---|---|---|---|
| Constant | −1.284 | 0.292 | 19.395 | − | 0.000 |
| Gender | 0.580 | 0.287 | 4.085 | 1.786 (1.018−3.134) | 0.043 |
| Age | −1.497 | 0.294 | 25.854 | 0.224 (0.126−0.399) | 0.000 |
| Disease severity | 1.940 | 0.341 | 32.311 | 6.955 (3.564−13.576) | 0.003 |
| Operation time | 0.876 | 0.299 | 8.582 | 2.401 (1.336−4.315) | 0.000 |
OR, odds ratio; CI, confidence interval.
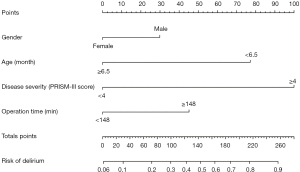
Construction of an early nomogram prediction model for delirium
Based on the independent risk factors of delirium in children after congenital heart surgery, the prediction model was constructed and the nomogram was drawn (Figure 1). The nomogram model obtained a total score based on the scores of each child’s independent risk factors, and the prediction value corresponding to the total score was the predicted probability of delirium in children after congenital heart surgery. The C-index of the model was 0.809 [95% confidence interval (CI): 0.758–0.859]. After 1,000 bootstrap resamples were generated, the adjusted C-index was 0.808 (95% CI: 0.756–0.856), and the area under the curve (AUC) was 0.809 (Figure 2). At this point, the sensitivity of the model was 76.1%, and specificity was 70%. The Brier value of the model was 0.142.
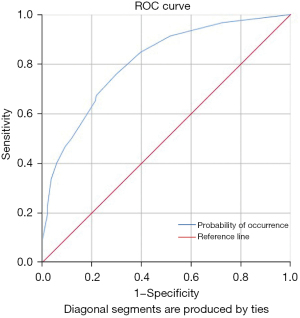
Clinical validation of the early nomogram prediction model
Between April 16 and May 15, 2021, 96 children treated after congenital heart surgery in the CICU of Shanghai Children’s Medical Center were enrolled to verify the effectiveness of the model. Among them, there were 47 males and 49 females, and the average age was 21 months. The model predicted 20 cases of delirium and 20 cases occurred, including 8 false negative and 8 false positive cases. At this time, C-index of the model was 0.747 (95% CI: 0.610–0.885), the sensitivity, specificity, and accuracy of the model were 60%, 89.5%, and 83.3%, respectively. It is worth noting that among the 20 cases of delirium, 14 cases occurred within 48 h after operation, and 10 cases were predicted by the model, with an accuracy of 71.4%, indicating that the model has a stronger ability to predict early postoperative delirium.
Discussion
Incidence of delirium and the research significance of the early nomogram prediction model
The results of this study showed that the incidence of delirium in children in the CICU after congenital heart surgery was 25.4%, which was lower than a similar study of delirium in children after cardiac surgery. The possible reasons are as follows: (I) in this study, nurses assessed delirium at 8:00, 14:00, and 20:00 every day, while assessment of delirium at night was not performed; (II) although the Chinese version of CAPD has good validity and high sensitivity and specificity, it cannot completely replace the gold standard, and there may have been a small number of missed diagnoses and misdiagnoses, especially of hypoactive delirium; and (III) since the evaluation of children was limited to the CICU, some cases of delirium after returning to the ward may have been missed.
Delirium in children after congenital heart surgery mostly occurs within 48 h of the operation. We analyzed 16 relevant influencing factors before and during surgery and constructed an early prediction model that had practical significance for early prevention and intervention after the operation. Delirium is very common in children after congenital heart surgery, greatly impacting on their prognosis (2,6,7) and even causing long-term cognitive impairment. Silver et al. (9) found that the quality of life score of children who had delirium during ICU hospitalization was consistently lower than that of children who had not experienced delirium. However, in reality, few nurses in the ICU have knowledge of children’s delirium. Because the prevalence of delirium in the CICU is high, medical staff must understand the condition in order to implement preventive interventions (10). As the nomogram prediction model provides visualization of the probability, it is more convenient for medical staff when making an evaluation. ICU medical staff can use this model to assess the risk of delirium when a child first enters the ICU after surgery to prevent the occurrence of delirium in advance, reduce the time of mechanical ventilation and hospital stay, and improve the long-term quality of life of the child.
The clinical application of the prediction model found that specificity was high, which was of positive significance for excluding the low-risk population of delirium, but sensitivity was low, reflecting the poor ability of the model to determine the children with delirium. The reason for this may have been that there were still some risk factors affecting the occurrence of delirium after surgery, including the use of sedative and analgesic drugs, mechanical ventilation, and other iatrogenic adverse stimuli. However, in order to prevent delirium early, we only included preoperative and intraoperative risk factors in our prediction model, and this may have had an impact on the accuracy of the model.
Analysis of independent risk factors for delirium in children after congenital heart surgery
The risk of postoperative delirium in male children is higher than that in female children
The gender ratio of children included in this study was close to 1:1, but the occurrence of delirium in male children was 1.8 times that of female children. In his study of delirium in a pediatric CICU, Alvarez et al. (2) also found that delirium in children after cardiac surgery was more likely to occur in males and young patients, and similarly, Silver et al. (11) reported that being a male child was a risk factor of delirium. Other studies have not found gender differences in children with delirium, and gender is not recommended as a risk factor for delirium in the European Society of Anesthesiology evidence-based and consensus-based guidelines on postoperative delirium (12). Therefore, it may be necessary to further expand the scope of research to explore the relationship between gender and delirium.
The younger the age, the higher the risk of delirium
Many studies have shown that children younger than 2 years old are more prone to delirium than older children, which is an independent risk factor for delirium (13-18). Children with congenital heart disease often undergo surgery at a young age and show a high rate of delirium after surgery. Meyburg et al. (19) and Alvarez et al. (2) pointed out that delirium was more likely to occur when age was ≤1 year old, and the younger the age, the higher the possibility of delirium. The best cut-off value was obtained through ROC curve analysis. The results showed that age less than 6.5 months was a risk factor of delirium, and 56.5% of children with delirium were less than 6.5 months old. Compared with older children, the central nervous system in infants and younger children is still immature and may be particularly vulnerable to stress and diseases. Further studies are needed to investigate the pathophysiology of delirium in young patients and the impact of delirium on their long-term neuropsychiatric health.
The higher the severity of the disease, the higher the risk of delirium
Disease severity (13-17,19,20) also directly affects the incidence of delirium and is an independent risk factor for delirium. There are many methods to measure the severity of disease. Studies have shown that children with delirium have a higher Risk Adjustment for Congenital Heart Surgery-1 (RACHS-1) score. In a study by Patel et al. (3), children with a RACHS-1 score of 2 accounted for 40% of the total number of children with delirium and was usually accompanied by multiple organ dysfunction. Similarly, Alvarez et al. (2) found a statistically significant association between the Society of Thoracic Surgeons and the European Association for Cardiothoracic Surgery Congenital Heart Surgery Mortality Score (STS-EACTS) and delirium, with delirium occurring in 77% of STS-EACTS category 5 and category 4 children. In this study, the severity of children’s condition was judged by PRISM III, and the results showed that the severity of the disease had a statistically significant association with delirium. The cut-off value was obtained through ROC curve analysis. Children with a total score of ≥4 were more likely to have delirium, and the incidence of delirium was 3.8 times that of children with a score of <4.
The longer the operation time and the longer the cardiopulmonary bypass time, the higher the risk of delirium
In this study, the incidence of delirium in children with longer operation time was 1.9 times that of children with shorter operation time. Cardiopulmonary bypass is a necessary condition for most open-heart surgery, but the process is non-physiological. The hypothetical mechanisms leading to delirium include systemic hypoperfusion, cell hypoxia, increased inflammatory mediators, and changes in neurotransmitters (3). Non-pulsatile blood flow affects the automatic regulation function of cerebral vessels and interferes with the matching of cerebral blood flow and metabolism. Hypothermia during cardiopulmonary bypass is not conducive to the release of oxygen. During the warming period, brain metabolism increases and the demand for oxygen in the brain increases. At the same time, the longer the operation time, the longer the cardiopulmonary bypass time, the lower the cerebral perfusion caused by hypotension, the non-pulsatile blood flow affects the self-regulation of micro arteries, and the excessive dilution of blood reduces the oxygen carrying capacity of blood, which will cause cerebral hypoxia, interfere with the normal cerebral oxygen metabolism, and cause postoperative delirium (21).
Insights into postoperative prevention of delirium in children
At present, there is little evidence that drugs are effective or safe in the treatment of delirium in children, while prevention is an effective measure for managing delirium. Identifying the risk factors of delirium can provide an early warning, and these include preoperative, intraoperative, and postoperative risk factors. Delirium in children after congenital heart surgery mostly occurs within 48 h of the operation, indicating that early delirium prediction is needed and the influence of preoperative and intraoperative factors on the occurrence of delirium in children cannot be ignored. Preoperative and intraoperative factors are non-intervenable factors for ICU medical staff. However, a prediction model based on preoperative and intraoperative risk factors can allow early predictions to be made once children enter the CICU after surgery to determine whether they are high-risk for delirium in order to take positive measures to deal with the intervenable postoperative risk factors and achieve prevention as early as possible.
Postoperative children often experience a variety of painful stimuli (4), and analgesia and sedation are basic components of CICU treatment (6). However, while controlling pain and reducing children’s irritability, they are also a risk factor for delirium. Delirium is more likely to occur when using benzodiazepines or opioids, and benzodiazepine exposure is an independent risk factor for delirium in children (2,22-24). Staveski et al. (4) have also found that children with higher sedation and higher opioid exposure are more likely to be delirium positive during the withdrawal of sedatives and/or opioids. In recent years, dexmedetomidine has been increasingly used in children (25-29). Dexmedetomidine is less likely to induce delirium than benzodiazepines (30) and has been recommended by the Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain as the sedative drug for critically ill pediatric postoperative cardiac surgical patients (31), but its application is limited by the dose-related side effects of bradycardia and hypotension. It is particularly important to accurately select and evaluate the correct dose of sedative and analgesic drugs for children with a high risk of delirium. A planned sedative and analgesic program can reduce the possibility of delirium to a certain extent. Adverse postoperative stimuli for children also include mechanical ventilation, physical restraint, invasive drainage tubes, and environmental changes, which may have an impact on the occurrence of delirium. For high-risk children with delirium, medical staff should try to reduce the stimuli, remove any tubes as soon as possible, and reduce physical restraint to children, under the condition of ensuring safety.
Innovation and limitations of this study
This study attempted to analyze preoperative and intraoperative factors in order to manage delirium in children after congenital heart surgery, which mostly occurs within 48 hours of the operation. A limitation of our study lies in the incomplete understanding of the risk factors of delirium in children after cardiac surgery at home and abroad, and as a result, the selection of measurement indicators may not have been comprehensive. Further, although the Chinese version of CAPD has good validity and high sensitivity and specificity, it cannot completely replace the gold standard, and there may have been a small number of missed diagnoses and misdiagnoses. In addition, the preliminary investigation and later verification application were limited to a third-class pediatric hospital in Shanghai, the sample was relatively limited, and there may have been problems with acceptance and overall applicability of the prediction model.
Conclusions
The nomogram for early prediction of delirium in children after congenital heart surgery established in this study used age, gender, disease severity, and operation time to provide timely evaluation of the probability of delirium and improve the recognition of delirium in children after congenital heart surgery.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the TRIPOD reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-187/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-187/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-187/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shanghai Children’s Medical Center (No. SCMCIRB-K2021027-1). Informed consent was taken from all the patients’ parents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hoffman JIe. The global burden of congenital heart disease. Cardiovasc J Afr 2013;24:141-5. [Crossref] [PubMed]
- Alvarez RV, Palmer C, Czaja AS, et al. Delirium is a Common and Early Finding in Patients in the Pediatric Cardiac Intensive Care Unit. J Pediatr 2018;195:206-12. [Crossref] [PubMed]
- Patel AK, Biagas KV, Clarke EC, et al. Delirium in Children After Cardiac Bypass Surgery. Pediatr Crit Care Med 2017;18:165-71. [Crossref] [PubMed]
- Staveski SL, Pickler RH, Khoury PR, et al. Prevalence of ICU Delirium in Postoperative Pediatric Cardiac Surgery Patients. Pediatr Crit Care Med 2021;22:68-78. [Crossref] [PubMed]
- Semple D, Howlett MM, Strawbridge JD, et al. A Systematic Review and Pooled Prevalence of Delirium in Critically Ill Children. Crit Care Med 2022;50:317-28. [Crossref] [PubMed]
- Dervan LA, Di Gennaro JL, Farris RWD, et al. Delirium in a Tertiary PICU: Risk Factors and Outcomes. Pediatr Crit Care Med 2020;21:21-32. [Crossref] [PubMed]
- Traube C, Mauer EA, Gerber LM, et al. Cost Associated With Pediatric Delirium in the ICU. Crit Care Med 2016;44:e1175-9. [Crossref] [PubMed]
- Feroz S, Donnelly KM. Not just to survive but to thrive: delirium in the pediatric cardiac ICU. Curr Opin Cardiol 2020;35:70-5. [Crossref] [PubMed]
- Silver G, Doyle H, Hegel E, et al. Association Between Pediatric Delirium and Quality of Life After Discharge. Crit Care Med 2020;48:1829-34. [Crossref] [PubMed]
- Staveski SL, Pickler RH, Lin L, et al. Management of Pediatric Delirium in Pediatric Cardiac Intensive Care Patients: An International Survey of Current Practices. Pediatr Crit Care Med 2018;19:538-43. [Crossref] [PubMed]
- Silver G, Traube C, Gerber LM, et al. Pediatric delirium and associated risk factors: a single-center prospective observational study. Pediatr Crit Care Med 2015;16:303-9. [Crossref] [PubMed]
- Aldecoa C, Bettelli G, Bilotta F, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol 2017;34:192-214. [Crossref] [PubMed]
- Cano Londoño EM, Mejía Gil IC, Uribe Hernández K, et al. Delirium during the first evaluation of children aged five to 14 years admitted to a paediatric critical care unit. Intensive Crit Care Nurs 2018;45:37-43. [Crossref] [PubMed]
- Trogrlić Z, van der Jagt M, Lingsma H, et al. Improved Guideline Adherence and Reduced Brain Dysfunction After a Multicenter Multifaceted Implementation of ICU Delirium Guidelines in 3,930 Patients. Crit Care Med 2019;47:419-27. [Crossref] [PubMed]
- Trogrlić Z, van der Jagt M, Bakker J, et al. A systematic review of implementation strategies for assessment, prevention, and management of ICU delirium and their effect on clinical outcomes. Crit Care 2015;19:157. [Crossref] [PubMed]
- Paterson RS, Kenardy JA, De Young AC, et al. Delirium in the Critically Ill Child: Assessment and Sequelae. Dev Neuropsychol 2017;42:387-403. [Crossref] [PubMed]
- Malas N, Brahmbhatt K, McDermott C, et al. Pediatric Delirium: Evaluation, Management, and Special Considerations. Curr Psychiatry Rep 2017;19:65. [Crossref] [PubMed]
- Ista E, van Beusekom B, van Rosmalen J, et al. Validation of the SOS-PD scale for assessment of pediatric delirium: a multicenter study. Crit Care 2018;22:309. [Crossref] [PubMed]
- Meyburg J, Dill ML, Traube C, et al. Patterns of Postoperative Delirium in Children. Pediatr Crit Care Med 2017;18:128-33. [Crossref] [PubMed]
- Zuppa AF, Curley MAQ. Sedation Analgesia and Neuromuscular Blockade in Pediatric Critical Care: Overview and Current Landscape. Pediatr Clin North Am 2017;64:1103-16. [Crossref] [PubMed]
- Horvath R, Shore S, Schultz SE, et al. Cerebral and somatic oxygen saturation decrease after delayed sternal closure in children after cardiac surgery. J Thorac Cardiovasc Surg 2010;139:894-900. [Crossref] [PubMed]
- Smith HAB, Gangopadhyay M, Goben CM, et al. Delirium and Benzodiazepines Associated With Prolonged ICU Stay in Critically Ill Infants and Young Children. Crit Care Med 2017;45:1427-35. [Crossref] [PubMed]
- Holly C, Porter S, Echevarria M, et al. CE: Original Research: Recognizing Delirium in Hospitalized Children: A Systematic Review of the Evidence on Risk Factors and Characteristics. Am J Nurs 2018;118:24-36. [Crossref] [PubMed]
- Mody K, Kaur S, Mauer EA, et al. Benzodiazepines and Development of Delirium in Critically Ill Children: Estimating the Causal Effect. Crit Care Med 2018;46:1486-91. [Crossref] [PubMed]
- Jiang L, Ding S, Yan H, et al. A retrospective comparison of dexmedetomidine versus midazolam for pediatric patients with congenital heart disease requiring postoperative sedation. Pediatr Cardiol 2015;36:993-9. [Crossref] [PubMed]
- Pan W, Wang Y, Lin L, et al. Outcomes of dexmedetomidine treatment in pediatric patients undergoing congenital heart disease surgery: a meta-analysis. Paediatr Anaesth 2016;26:239-48. [Crossref] [PubMed]
- Riker RR, Shehabi Y, Bokesch PM, et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: a randomized trial. JAMA 2009;301:489-99. [Crossref] [PubMed]
- Kang X, Tang X, Yu Y, et al. Intraoperative dexmedetomidine infusion is associated with reduced emergence agitation and improved recovery profiles after lung surgery: a retrospective cohort study. Drug Des Devel Ther 2019;13:871-9. [Crossref] [PubMed]
- Simonini A, Brogi E, Conti G, et al. Dexmedetomidine reduced the severity of emergence delirium and respiratory complications, but increased intraoperative hypotension in children underwent tonsillectomy. A retrospective analysis. Minerva Pediatr (Torino) 2021. [Epub ahead of print]. doi:
10.23736/S2724-5276.21.06330-8 .10.23736/S2724-5276.21.06330-8 - Motta E, Luglio M, Delgado AF, et al. Importance of the use of protocols for the management of analgesia and sedation in pediatric intensive care unit. Rev Assoc Med Bras (1992) 2016;62:602-9. [Crossref] [PubMed]
- Smith HAB, Besunder JB, Betters KA, et al. 2022 Society of Critical Care Medicine Clinical Practice Guidelines on Prevention and Management of Pain, Agitation, Neuromuscular Blockade, and Delirium in Critically Ill Pediatric Patients With Consideration of the ICU Environment and Early Mobility. Pediatr Crit Care Med 2022;23:e74-110. [Crossref] [PubMed]


