
Uterine fibroids increase the risk of preterm birth and other adverse birth events: a systematic review and meta-analysis
Introduction
Uterine fibroids (UF) are benign tumors originating from a uterine muscle tissue chamber composed of smooth muscle cells and fibroblasts embedded in the extracellular matrix. Compared with normal myometrium, small myomas have a similar number of leukocytes and less proliferation, but large myomas contain more cell proliferation and fewer leukocytes (1). Age and race are the main risk factors for the development and growth of uterine leiomyoma. Asymptomatic women may find many leiomyomas by chance during clinical ultrasound or examination (2). During pregnancy, the prevalence of hysteromyoma is between 3% and 12% (3,4).
Controversy exists regarding whether uterine fibroids contribute to adverse events during pregnancy and childbirth. Some studies have pointed out that uterine fibroids may also lead to pregnancy-related complications, such as miscarriage, premature rupture of membranes, dysfunction, placental abruption, and higher rates of cesarean section and postpartum hemorrhage (5,6). A different study (7) showed that hysteromyoma increases the risk of cesarean section and preterm premature rupture of membranes. Still, it has no significant effect on preterm birth, postpartum hemorrhage, hip presentation, and low birth weight. Previous meta-analyses have illustrated that hysteromyoma will not lead to abortion but will present the risk of placental abruption, cesarean section, and congenital malformation of a full-term fetus (8-11). However, these previous meta-analyses only observed the incidence of one or a few adverse events, which has limitations. In addition, our analysis believes that advances in medical technology, nursing concepts, and detection methods will also have an impact on the incidence of adverse events during pregnancy. We believe that a meta-analysis to update previous findings is warranted. This study intends to review the latest published literature and conduct a meta-analysis to explore the impact of hysteromyoma on the risk of preterm birth and other obstetric-related outcomes. We present the following article in accordance with the MOOSE reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-215/rc).
Methods
Bibliography retrieval
The English databases PubMed, Medline, Embase and Central were searched from the time of database establishment to April 2022. The retrieval method was medical subject words combined with free words. English search and subject words mainly included “UF OR uterine fibroid OR uterine myoma OR uterine leiomyoma” AND “preterm birth OR preterm delivery”.
Literature screening
The inclusion criteria were as follows: (I) the participants were pregnant women diagnosed with hysteromyoma; (II) the literature type was an observational study, including cohort studies and case-control studies; types of literature were observational studies, including cohort studies and case-control studies; (III) the study set up a case group and a control group. In the cohort study, the case group was pregnant women with uterine fibroids, and the control group was pregnant women without uterine fibroids. In the case-control study, the case group consisted of women with adverse events, and the control group consisted of women without adverse events; and (IV) the study literature included at least one of the following outcome indicators: preterm birth, premature rupture of membranes, placental abruption, cesarean section rate, postpartum hemorrhage, gestational age at delivery, and birth weight.
The exclusion criteria were as follows: (I) news reports, expert opinions, critical literature, and abstracts; (II) republished literature; and III. Inability to obtain enough literature to analyze the data.
Document data extraction
The literatures were screened and the data was extracted by two researchers independently. The main extraction contents included: (I) title, publication date, author, and so on; (II) research type, interventions, outcomes, and so on; and (III) baseline information. Adverse events (preterm birth, premature rupture of membranes, placental abruption, cesarean section, postpartum hemorrhage) were described using incidence as the effect size. Gestational age and birth weight were described with measurement data (weeks and Kg) as effect sizes. If there were questions or differences of opinion in the process of literature screening and extraction, a third researcher assisted in resolving the differences and making a decision through joint discussion if necessary.
Literature quality evaluation
The quality of the observational study was evaluated by Newcastle-Ottawa Scale (NOS). The NOS scale is divided into the NOS evaluation criteria for a cohort study and the NOS evaluation criteria for a case-control study. It is further divided into three blocks (population selection, comparability, exposure evaluation or result evaluation), including 8 items. It is scored by the star system. The full score available for a cohort study is 13 stars, and the full score available for a disease case-control study is 9 stars. Two researchers independently evaluated the quality of the included literature and then performed crosschecking. If there is any difference, the researchers engaged in discussion to reach an agreement, or a ruling was made by the third researcher.
Statistical method
This study used the Cochrane software RevMan 5.4 [The Cochrane Collaboration, 2020) for statistical analysis of all data. Unadjusted odds ratio (OR) and 95% confidence interval (CI) were calculated from literature raw data. The risk factor ORs of cohort studies and controlled pathology studies could be pooled. The measurement data were statistically described by mean difference (MD) and 95% CI. Statistical significance was considered when P<0.05 in the fixed effects model or random effects model. The chi-square test was applied for heterogeneity test. When the I2>50%, the random effects model was used because of heterogeneous. When I2≤50%, the fixed effects model was adopted because of no heterogeneous. Subgroup analyses were used to explore sources of heterogeneity. The potential publication bias was estimated by Egger test. Two-way P<0.05 indicated statistical significance.
Results
Literature search results
In this study, 345 relevant articles were obtained through database retrieval. After the retrieved and collected articles were deduplicated by EndNote X9 management software (Clarivate Analytics, Philadelphia, PA, USA), they were preliminarily screened through reading topics and abstracts according to the pre-determined inclusion and exclusion criteria and then further reading of the full text for re-screening. Finally, 11 articles meeting the criteria were included. The specific screening process and results are shown in Figure 1.
Basic characteristics and quality evaluation of literature
A total of 11 studies were included according to the screening criteria. The basic information of the included literature is shown in Table 1. The time of publication was from 2010 to 2021. The included literature was relatively new. The literature types were observational studies, including 7 retrospective cohort studies and 4 case-control studies. The study populations included the United States, France, Italy, Japan, Turkey, Cameroon, and China. The 11 studies included 12,522 pregnant women diagnosed with hysteromyoma and 301,391 pregnant women without hysteromyoma in the control group. There was no difference in maternal age between the hysteromyoma and control group, with an average of 28.6–36.1 years. All articles had studied the risk of uterine fibroids for preterm birth and explored other obstetric related outcome indicators, including <37 weeks of preterm birth, <34 weeks of preterm birth, premature rupture of membranes, placental abruption, cesarean section rate, postpartum hemorrhage, gestational age at delivery, and birth weight.
Table 1
| ID | Research type | Country | Sample size | Maternal age, years | Outcome indicators | Quality assessment |
|---|---|---|---|---|---|---|
| Blitz 2016 (12) | Retrospective cohort study | USA | 522/9,792 | 33.3/30.9 | 1, 7, 8 | 9 |
| Cagan 2020 (13) | Retrospective cohort study | Turkey | 25/147 | 35.0/33.0 | 1, 6 | 7 |
| Ciavattini 2015 (14) | Case control study | Italy | 219/219 | 34.8/34.8 | 1, 3, 6 | 9 |
| Egbe 2018 (15) | Case control study | Cameroon | 38/188 | 31.4/27.4 | 1, 2, 3 | 8 |
| Girault 2018 (16) | Retrospective cohort study | France | 301/12,216 | 36.1/31.3 | 1, 2, 3, 4, 5, 7, 8 | 9 |
| Kellal 2010 (17) | Case control study | France | 117/234 | NR | 1 | 8 |
| Lai 2012 (18) | Retrospective cohort study | USA | 401/14,703 | 33.7/28.6 | 1, 2, 5, 7, 8 | 8 |
| Murata 2021 (19) | Retrospective cohort study | Japan | 5,354/81,016 | 35.1/31.1 | 1, 3, 4, 5, 7 | 9 |
| Stout 2010 (20) | Retrospective cohort study | USA | 2,058/61,989 | 35.1/30.0 | 1, 2, 3, 5, 6 | 8 |
| Sundermann 2021 (21) | Prospective cohort study | USA | 475/4,147 | NR | 1, 2 | 8 |
| Zhao 2017 (22) | Case control study | China | 3,012/109,931 | 32.0/29.5 | 1, 3, 4, 5, 6, 7 | 9 |
1, premature birth <37 weeks; 2, preterm birth <34 weeks; 3, premature rupture of membranes; 4, placental abruption; 5, Cesarean section rate; 6, postpartum hemorrhage; 7, Gestational age at delivery; 8, birth weight. NR, not reported.
The NOS was used to evaluate the quality of 4 case-control studies and 7 cohort studies. All research scores were greater than 7 points, including 7 points for 1 article, 8 points for 5 articles, and 9 points for 5 articles. It was considered that the risk level of the included literature was low, and the quality of the literature was high.
Meta-analysis results
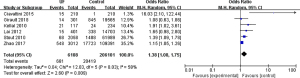
A total of 11 studies reported the risk of premature delivery <37 weeks in pregnant women with hysteromyoma. The results of meta-analysis were OR =1.43, 95% CI: 1.25 to 1.64, P<0.00001, and I2=64%. Five studies reported the risk of premature delivery <34 weeks in pregnant women with hysteromyoma. The results of meta-analysis were OR =1.73, 95% CI: 1.34 to 2.25, P<0.0001, and I2=72%. Six studies reported the risk of uterine fibroids on premature rupture of membranes, OR =1.38, 95% CI: 1.08 to 1.75, P=0.009, and I2=58%. Three studies reported the risk of uterine fibroids for placental abruption, OR =1.60, 95% CI: 1.20 to 2.14, P=0.001, and I2=33%. Five studies reported the effect of hysteromyoma on cesarean section, OR =2.09, 95% CI: 1.69 to 2.58, P<0.00001, and I2=61%. Four studies reported the risk of uterine fibroids on postpartum hemorrhage, OR =2.95, 95% CI: 1.86 to 4.66, P<0.00001, and I2=82%. Five studies reported the effect of hysteromyoma on gestational age at delivery, and the combined results were MD =−0.58, 95% CI: −0.66 to −0.51, P<0.00001, and I2=0%. Three studies reported the effect of uterine fibroids on birth weight, for which the combined results were MD =−117.82, 95% CI: −155.19 to −80.45, P<0.00001, and I2=0%. Uterine fibroids have a significant impact on all obstetric outcome indicators such as preterm birth, as shown in Figures 2-9.
Publication bias assessment
The outcome indicators with more than 10 articles need to be evaluated for publication bias. More than 10 articles of preterm birth <37 weeks reached the indicator. A funnel chart illustrated that most points were within the CI, showing an inverted funnel type. As shown in Figure 10, it was considered that there was no publication bias.
Discussion
Preterm delivery refers to the delivery after 28 weeks of pregnancy but before 37 weeks of gestation. The earlier the preterm baby is born, the lighter their weight will be, the more serious the immature development of various organs will be, and the probability of short- and long-term health problems will be greater. Hysteromyoma is a multiple benign tumor in women aged 30–50 years, affecting about 70–80% of women throughout their life (3,23). Uterine fibroids are mostly asymptomatic, and asymptomatic uterine fibroids are commonly diagnosed through routine prenatal ultrasound, with up to 11% of pregnant women exhibiting uterine fibroids (24). However, the combined results of the literature included in this study showed that the probability of pregnant women experiencing uterine fibroids is about 4%. The reason for this analysis result may be related to the main population included in this study. Most of the people included in this study were from the United States, France, and other countries. Previous studies have shown that the probability of women experiencing hysteromyoma in African countries is 2–3 times that of those in other countries (3,24).
Due to the typical hormonal state and vascular changes throughout pregnancy, patients often worry about the accelerated growth and consequences of leiomyoma during pregnancy. In addition, it is generally believed that a hysteromyoma that distorts the endometrial cavity may impact fertility and lead to adverse reproductive outcomes, such as preterm birth and placental abruption. Many studies have investigated the relationship between hysteromyoma and obstetric outcomes, but the conclusions have remained controversial. This study conducted a meta-analysis of obstetric outcome indicators such as preterm delivery with hysteromyoma by searching the latest published literature. The heterogeneity test results showed no heterogeneity in gestational age, birth weight, and placental abruption at delivery. The fixed effects model was adopted, and other indicators such as preterm birth were heterogeneous. The random effects model was adopted. The results showed that hysteromyoma not only caused preterm birth of <37 weeks or <34 weeks but also had a significant impact on other obstetric outcomes. The rates of cesarean section and postpartum hemorrhage in pregnant women with hysteromyoma were higher, premature rupture of membranes and placental abruption were also caused, and the gestational age and birth weight at delivery were lower. The incidence of low birth weight is also related to premature birth. The birth weight of the group with hysteromyoma was about 118 grams lower than that of the control group.
All English articles included in this study were of high quality, and the sample size of combined patients was large, covering the population of various countries and regions. The results are representative. However, the included studies were retrospective studies, which are uneven in methodology and literature quality, and may have led to some bias in the results.
In conclusion, pregnant women with hysteromyoma will face an increased risk of preterm birth, premature rupture of membranes, placental abruption, cesarean section, postpartum hemorrhage, and delivering a low birth weight baby. However, the mechanism of hysteromyoma increasing the risk of preterm birth is not clear. The analysis of this study will contribute to clinical practice and better design-related future research. Effective management of uterine fibroids during pregnancy requires a better understanding of their growth, differentiation, and cell renewal. We also look forward to more relevant mechanism research to fill the gap in pathophysiology to formulate better future intervention measures to prevent pregnancy complications in women with uterine fibroids.
Acknowledgments
Funding: The project was supported by Hainan Province Clinical Medical Center.
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://tp.amegroups.com/article/view/10.21037/tp-22-215/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-215/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Holdsworth-Carson SJ, Zhao D, Cann L, et al. Differences in the cellular composition of small versus large uterine fibroids. Reproduction 2016;152:467-80. [Crossref] [PubMed]
- Jayes FL, Liu B, Feng L, et al. Evidence of biomechanical and collagen heterogeneity in uterine fibroids. PLoS One 2019;14:e0215646. [Crossref] [PubMed]
- Baird DD, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol 2003;188:100-7. [Crossref] [PubMed]
- Parazzini F, Tozzi L, Bianchi S. Pregnancy outcome and uterine fibroids. Best Pract Res Clin Obstet Gynaecol 2016;34:74-84. [Crossref] [PubMed]
- Martin J, Ulrich ND, Duplantis S, et al. Obstetrical Outcomes of Ultrasound Identified Uterine Fibroids in Pregnancy. Am J Perinatol 2016;33:1218-22. [Crossref] [PubMed]
- Hartmann KE, Velez Edwards DR, Savitz DA, et al. Prospective Cohort Study of Uterine Fibroids and Miscarriage Risk. Am J Epidemiol 2017;186:1140-8. [Crossref] [PubMed]
- Chen R, Liu F. Analysis of adverse effects of uterine fibroids on pregnancy outcomes. Nongken Medical 2021;43:103-8.
- Jenabi E, Ebrahimzadeh Zagami S. The association between uterine leiomyoma and placenta abruption: A meta-analysis. J Matern Fetal Neonatal Med 2017;30:2742-6. [Crossref] [PubMed]
- Jenabi E, Fereidooni B. The uterine leiomyoma and placenta previa: a meta-analysis. J Matern Fetal Neonatal Med 2019;32:1200-4. [Crossref] [PubMed]
- Sundermann AC, Velez Edwards DR, Bray MJ, et al. Leiomyomas in Pregnancy and Spontaneous Abortion: A Systematic Review and Meta-analysis. Obstet Gynecol 2017;130:1065-72. [Crossref] [PubMed]
- Jenabi E, Khazaei S. The effect of uterine leiomyoma on the risk of malpresentation and cesarean: a meta-analysis. J Matern Fetal Neonatal Med 2018;31:87-92. [Crossref] [PubMed]
- Blitz MJ, Rochelson B, Augustine S, et al. Uterine fibroids at routine second-trimester ultrasound survey and risk of sonographic short cervix. J Matern Fetal Neonatal Med 2016;29:3454-60. [Crossref] [PubMed]
- Cagan M, Tanacan A, Donmez HG, et al. The Effect of Small Size Uterine Fibroids on Pregnancy Outcomes in High-risk Pregnancies. Rev Bras Ginecol Obstet 2020;42:535-9. [Crossref] [PubMed]
- Ciavattini A, Clemente N, Delli Carpini G, et al. Number and size of uterine fibroids and obstetric outcomes. J Matern Fetal Neonatal Med 2015;28:484-8. [Crossref] [PubMed]
- Egbe TO, Badjang TG, Tchounzou R, et al. Uterine fibroids in pregnancy: prevalence, clinical presentation, associated factors and outcomes at the Limbe and Buea Regional Hospitals, Cameroon: a cross-sectional study. BMC Res Notes 2018;11:889. [Crossref] [PubMed]
- Girault A, Le Ray C, Chapron C, et al. Leiomyomatous uterus and preterm birth: an exposed/unexposed monocentric cohort study. Am J Obstet Gynecol 2018;219:410.e1-7. [Crossref] [PubMed]
- Kellal I, Haddouchi NE, Lecuyer AI, et al. Leiomyoma during pregnancy: which complications?. Gynecol Obstet Fertil 2010;38:569-75. [Crossref] [PubMed]
- Lai J, Caughey AB, Qidwai GI, et al. Neonatal outcomes in women with sonographically identified uterine leiomyomata. J Matern Fetal Neonatal Med 2012;25:710-3. [Crossref] [PubMed]
- Murata T, Kyozuka H, Endo Y, et al. Preterm Deliveries in Women with Uterine Myomas: The Japan Environment and Children's Study. Int J Environ Res Public Health 2021;18:2246. [Crossref] [PubMed]
- Stout MJ, Odibo AO, Graseck AS, et al. Leiomyomas at routine second-trimester ultrasound examination and adverse obstetric outcomes. Obstet Gynecol 2010;116:1056-63. [Crossref] [PubMed]
- Sundermann AC, Aldridge TD, Hartmann KE, et al. Uterine fibroids and risk of preterm birth by clinical subtypes: a prospective cohort study. BMC Pregnancy Childbirth 2021;21:560. [Crossref] [PubMed]
- Zhao R, Wang X, Zou L, et al. Adverse obstetric outcomes in pregnant women with uterine fibroids in China: A multicenter survey involving 112,403 deliveries. PLoS One 2017;12:e0187821. [Crossref] [PubMed]
- Grube M, Neis F, Brucker SY, et al. Uterine Fibroids - Current Trends and Strategies. Surg Technol Int 2019;34:257-63. [PubMed]
- Laughlin SK, Baird DD, Savitz DA, et al. Prevalence of uterine leiomyomas in the first trimester of pregnancy: an ultrasound-screening study. Obstet Gynecol 2009;113:630-5. [Crossref] [PubMed]











