
Risk factors for pathological fractures of simple bone cysts of the humerus in children: a retrospective cohort study
Introduction
Simple bone cysts (SBCs) are the most common osteolytic lesions in children, which usually occur in the long bones of the extremities. In approximately 80% of cases, the lesions occur in the proximal humerus and the proximal femur. The main indication for the treatment of SBCs is the risk of pathological fractures (1,2). Clinically, SBCs rarely achieves complete cure, except with wide excision which has a recurrence rate of 30%. Due to the high risk of pathological fractures and the persistent symptoms of pain and lameness, surgery is currently the first choice of clinical treatment for SBCs with lesions located in the weight-bearing part (femoral neck). However, when the lesion is located in the non-bearing part (humerus) and the risk of pathological fracture is uncertain, there are many disputes about the timing of treatment (3,4). All SBCs will heal by themselves, but they will not subside until the bone is mature. During this period, it is often necessary to restrict movement in order to avoid pathological fracture. If clinicians are worried that the disease is too large or children have too much activity and lead to fracture, it is usually preventive aspiration and injection of methylprednisolone or surgical intervention. When pathological fractures occur, the local thin bone cortex makes internal fixation very difficult. External fixation alone usually increases the risk of fracture malunion. Therefore, identifying the risk factors for pathological fractures in children with humeral SBCs is crucial for the development of an appropriate timing of operation and the best prognosis for the patients.
Kaelin and MacEwen presented the cyst index as an easily reproducible method of assessing the mechanical resistance of the cyst wall (5,6). The cyst index relates the area of the cyst to the size of the bone expressed as the square of the diameter of the diaphysis. It is proposed that the cyst index can be used to evaluate the progress of cysts and the risk of pathological fractures, so as to facilitate clinicians to make judgments on whether reoperation is needed. However, a further retrospective analysis by Vasconcellos et al. suggested that the cyst index was not associated with the risk of pathological fractures (7). In view of this, it is imperative to study the risk factors of pathological fractures. This current research retrospectively analyzed 45 children with bone cysts of the humerus and examined the risk of pathological fractures and the timing of surgical intervention. We present the following article in accordance with the STARD reporting checklist (available at https://tp.amegroups.com/article/view/10.21037/tp-22-290/rc).
Methods
Study design
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethical committee of the Shanghai Children’s Hospital (No. 2017R023-F01). Written informed consent for this study was obtained from all the children’s parents.
The following inclusion criteria were applied: (I) children aged 2–15 years old; (II) the lesions were all located in the humerus; and (III) the X-ray films were all typical imaging manifestations of SBCs. The following exclusion criteria were applied: (I) the lesions were located in the femur, tibia, or short bone, etc.; (II) patients had bone cyst lesions without surgery and atypical imaging findings; and (III) patients with incomplete follow-up and imaging data. The patients were divided into a fracture group and a non-fracture group. Fracture group: pathological fracture has occurred or pathological fracture occurs within 6 weeks after the lesion is found. Non-fracture group: no fracture occurred after the focus was found, and no fracture occurred within 6 weeks of the first follow-up. The potential predictors of the risk fractures were tested using a logistic regression model.
Statistical analysis of the relationship between pathological fractures and age, gender, cyst index; and the link between the TEAL and pathological fractures were conducted.
Baseline characteristics
The medical records and imaging data of SBCs patients admitted to the Department of Orthopedics of Shanghai Children’s Hospital from January 2014 to December 2021 were retrospectively analyzed. A total of 46 patients satisfied the inclusion and exclusion criteria. One patient who did not receive X-ray examination before open reduction and internal fixation was excluded. Finally, a total of 45 children with a median age of 9 years (range, 3–13 years) were enrolled in this study, including 35 males and 10 females. One patient who did not receive X-ray examination before open reduction and internal fixation was excluded, and a total of 45 children were analyzed.
Imaging, cyst index, and the TEAL
The X-ray images all showed typical SBC lesions, which were central osteolytic lesions, and larger lesions may thin the bone cortex. Radiographs of pathological fractures showed small septa and occasional tiny fragments (leaf-foliation sign) within the cystic cavity, all of which were lesions of the humerus.
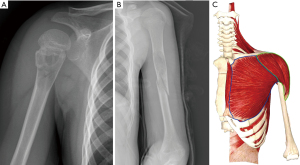
The cyst index is measure using the area of the lesion cyst on the frontal and lateral X-rays. It is obtained by dividing the area by the square of the diameter of the diaphysis by making a trapezoid at the cyst edge. A humeral lesion cyst index of 4 or more is associated with a higher risk of pathological fractures (5) (Figure 1).
As for how to locate the muscle attachment point in the plain, since the plain is the most basic examination, we can only locate the humeral attachment point of the deltoid muscle which is the most obvious in the proximal humerus. If the focus is located near the deltoid muscle attachment point or partially near the deltoid muscle attachment point, referring to the muscle anatomy of the shoulder, we believe that TEAL is located on the bone cortex of the lesion (8,9).
Calculation of the cyst index
A total of 5 researchers, including 2 pediatric orthopedists, 2 radiologists, and 1 intern, calculated the cyst index and determined whether the TEAL was attached to the cortical bone of the lesion. If the error was greater than 0.1, the case warranted recalculation, and the average of the results was taken as the cyst index of the case. All researchers shared the same opinion on the TEAL.
Statistical analysis
The SPSS22.0 software was used to organize and analyze the data, and the results of the cyst index on the frontal and lateral radiographs were assessed using t-tests. A P value <0.05 was considered statistically significant. For non-normally distributed measurement data such as age, gender, cyst index, and TEAL, the median and interquartile range [M (P25, P75)] were used to represent the variables, and the variables were analyzed by binary logistic regression to draw the characteristics of the subjects. Binary logistic method: forward selection. The difference was statistically significant with P<0.05.
Results
In this study cohort, there were 10 cases in the non-fracture group and 35 cases in the fracture group. There was no significant difference in the cyst index between the 2 groups, as measured by 2 radiograph angles (5.16±2.06 vs. 5.17±05, P>0.05). Binary logistic regression analysis was used to assess that the relationship between age, gender, cyst index (over 4 points or less), and the presence or absence of the TEAL. There was a relationship between risk of fracture and muscle attachment point [odds ratio (OR) =21.423, 95% confidence interval (CI): 2.409–190.539; P=0.006] (Table 1). In addition, most of the cases in the fracture group were greenstick fractures (Figure 2A). Examination of the medical history revealed that the trauma mechanism was caused by mild violence during shoulder extension and abduction. Radiographs revealed a bone cyst at the proximal humerus and a pathological fracture. When there is no muscle attachment point at the lesion, the pathological fracture tended to be a dislocation fracture (Figure 2B), and the trauma was usually caused by direct violence.
Table 1
| Risk factor | B | Ward (χ2) | P value | Exp(B) | 95% CI |
|---|---|---|---|---|---|
| Age | 0.012 | 0.917 | 0.338 | 1.012 | 0.988–1.037 |
| Sex | −1.324 | 1.976 | 0.16 | 0.266 | 0.042–1.685 |
| Cyst index | 0.062 | 0.08 | 0.777 | 1.064 | 0.693–1.634 |
| TEAL | 3.064 | 7.553 | 0.006 | 21.423 | 2.409–190.539 |
The relationship between pathological fractures and age, gender, and cyst index. B, the regression coefficient; 95% CI, 95% confidence interval; TEAL, tendon insertion site of ectopectoralis and anconeus lateralis.
Discussion
Bone cysts are benign lesions at the epiphysis. Such lesions will gradually separate with age, and the cyst may eventually heal itself and be replaced by normal bone tissue (10). Assessing the risk of pathological fracture is the most important part of clinical treatment and an important determining factor of surgical intervention (11).
Kaelin and MacEwen first proposed the concept of a cyst index and pointed out that determining the exact timing of the risk of pathological fractures is crucial for surgical intervention. They found that fracture risk did not correlate with cyst length and size, but rather had a significant correlation with cyst index (5). However, Vasconcellos et al. believed that the cyst index could not predict the risk of pathological fractures, and suggested that when measuring the lesion area, there was a huge difference between the anterior and lateral radiographs, and there were obvious errors between different operators. Thus, they concluded that it is not possible to accurately measure the actual size of the cyst (7). Pireau et al. (12) showed that T1-weighted magnetic resonance imaging (MRI) was the best detection method for observing cyst area, cyst diameter, and cortical bone thickness, and agreed with Kaelin and MacEwen. Moreover, he concluded that there was no significant difference in cyst area between frontal and lateral radiographs (12).
Based on previous research, the relationship between pathological fractures and cyst index, age, and gender remains controversial. As a new factor, the relationship between the TEAL and pathological fractures has rarely been examined. Therefore, the relationship between pathological fractures and age, gender, cyst index, and the TEAL was analyzed in this investigation to explore the risk factors of pathological fractures. The results indicated that the occurrence of pathological fractures was not correlated with cyst index, age, nor gender, but was correlated with the TEAL at the lesion. Applying the cyst index to our patient group did not prove to be an accurate predictor of pathological fractures. The study suggested that a cyst index cannot be used as a predictor of fracture risk in patients, while lesions located in the TEAL are an independent risk factor for pathological fractures. Moreover, this report demonstrated that most of the patients in the cohort suffered from mild trauma during abduction and extension of the shoulder joint, and most of the pathological fractures were located in the TEAL. Some scholars have reported shoulder pain in teenage women after swimming (13). We speculate that the local cortical bone at the lesion was thinned and weakened, and the muscle attachment points of the pectoralis major and the lateral head of the triceps were in the cortex of the bone. At the same level, greenstick fractures occur when thin cortical bone is interacted by forces of opposite vectors. Given the high recurrence rate of SBCs, and incomplete surgical curettage of the cyst wall in larger lesions being the main factor for recurrence (14), our results may give clinicians alternative treatment options. When the lesion is large and the bone cortex of the lesion is not located in the TEAL, the traditional surgical method cannot completely remove the cyst wall without significant surgical trauma. Patients can be given multiple hormones, autologous bone marrow injections, synthetic bone grafts, and other treatment methods (15) without worrying about the risk of pathological fractures during the course of treatment. As for locating the muscle attachment point in the plain film. We could only locate the humerus attachment point of the deltoid muscle, which is the most obvious proximal humerus. Proximal to the muscle attachment point (Figure 2C), referring to the muscle anatomy of the shoulder, we observe that the TEAL is located on the cortical bone of the lesion.
In clinical work, X-ray is often the most basic examination method. Due to the excessive radiation of CT, MRI is more accurate and has no radiation (12,16), but it needs to be examined under sedation and the waiting time is too long (3–4 weeks), which will delay the best treatment opportunity of patients. Therefore, it is the most efficient way to judge the risk of pathological fracture through the most basic examination.
Conclusions
The results of this study will aid clinicians in making a preliminary treatment plan after assessing the risk of pathological fractures in patients with SBC.
There were certain limitations to this investigation, including the small number of cases, and the inability to precisely locate the attachment point of the tendon. Nevertheless, these limitations were also identified in previous study of fracture risk related to SBC (17).
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist Available at https://tp.amegroups.com/article/view/10.21037/tp-22-290/rc
Data Sharing Statement: Available at https://tp.amegroups.com/article/view/10.21037/tp-22-290/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tp.amegroups.com/article/view/10.21037/tp-22-290/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the ethical committee of the Shanghai Children’s Hospital (No. 2017R023-F01). Written informed consent for this study was obtained from all the children’s parents.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zambo I, Veselý K. WHO classification of tumours of soft tissue and bone 2013: the main changes compared to the 3rd edition. Cesk Patol 2014;50:64-70.
- Pichon N, Negrier AC, Genah I, et al. Tumeurs osseuses bénignes de la hanche. Available online: https://www.sciencedirect.com/science/article/abs/pii/S1878622719300931
- Teoh KH, Watts AC, Chee YH, et al. Predictive factors for recurrence of simple bone cyst of the proximal humerus. J Orthop Surg (Hong Kong) 2010;18:215-9. [Crossref] [PubMed]
- Darwish AE, Hasan BZ, Elgebery AO, et al. The Clinical and Radiological Outcome of Stages 1 and 2 Enneking Benign Bone Lesions with Pathological Fracture. Injury 2021;52:2920-5. [Crossref] [PubMed]
- Kaelin AJ, MacEwen GD. Unicameral bone cysts. Natural history and the risk of fracture. Int Orthop 1989;13:275-82. [Crossref] [PubMed]
- Cha SM, Shin HD, Kim KC, et al. Flexible intramedullary nailing in simple bone cysts of the proximal humerus: prospective study for high-risk cases of pathologic fracture. J Pediatr Orthop B 2013;22:475-80. [Crossref] [PubMed]
- Vasconcellos DA, Yandow SM, Grace AM, et al. Cyst index: a nonpredictor of simple bone cyst fracture. J Pediatr Orthop 2007;27:307-10. [Crossref] [PubMed]
- Cho H, Lee HY, Gil YC, et al. Topographical anatomy of the radial nerve and its muscular branches related to surface landmarks. Clin Anat 2013;26:862-9. [PubMed]
- Petchprapa CN, Vaswani D, Garwood E, et al. The smoke sign: a secondary sign of unsuspected acute pectoralis major tendon injury on routine shoulder MRI. Skeletal Radiol. 2021;50:1873-80. [Crossref] [PubMed]
- Mascard E, Gomez-Brouchet A, Lambot K. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res 2015;101:S119-27. [Crossref] [PubMed]
- Zhang KX, Chai W, Zhao JJ, et al. Comparison of three treatment methods for simple bone cyst in children. BMC Musculoskelet Disord 2021;22:73. [Crossref] [PubMed]
- Pireau N, De Gheldere A, Mainard-Simard L, et al. Fracture risk in unicameral bone cyst. Is magnetic resonance imaging a better predictor than plain radiography? Acta Orthop Belg 2011;77:230-8. [PubMed]
- Savic M, Lee A, Hook A. Clinical presentation of an adolescent female synchronized swimmer with a simple bone cyst in the proximal humerus: a case report. J Can Chiropr Assoc 2019;63:171-7. [PubMed]
- Flont P, Malecki K, Niewola A, et al. Predictive characteristic of simple bone cyst treated with curettage and bone grafting. BMC Musculoskelet Disord 2015;16:350. [Crossref] [PubMed]
- Nunziato C, Williams J, Williams R. Synthetic Bone Graft Substitute for Treatment of Unicameral Bone Cysts. J Pediatr Orthop 2021;41:e60-6. [Crossref] [PubMed]
- Hong J, Cabe GD, Tedrow JR, et al. Failure of trabecular bone with simulated lytic defects can be predicted non-invasively by structural analysis. J Orthop Res 2004;22:479-86. [Crossref] [PubMed]
- Ahn JI, Park JS. Pathological fractures secondary to unicameral bone cysts. Int Orthop 1994;18:20-2. [Crossref] [PubMed]



