Regulatory T cells and Th1/Th2 in peripheral blood and their roles in asthmatic children
Bronchial asthma (asthma), particularly in the young, is a disease associated with an underlying atopic allergic hypersensitivity to one or more allergens. It is one of the most common childhood chronic diseases pathologically characterized by respiratory tract inflammation and airway remodeling (1). A majority of patients with asthma have an atopic background. T helper 2 type (Th2) cells are believed to augment the inflammatory response observed in asthma by expressing multiple cytokines such as interleukin (IL)-4 and IL-5, which play a central role in asthma and allergy (2-4). While interferon-γ (IFN-γ) is also a cytokine secreted by Th1. As Th1 cells crossregulate Th2 cells in some systems, it was assumed that Th1 cells downmodulated the effects of Th2 cells and thus had a beneficial role in asthma (5). However, it was reported that Th1 cells were themselves pro-inflammatory, and that the development of a Th1-associated inflammatory response could exacerbate asthma (5). In addition, Th cell subsets have also been shown to suppress each other (6). For instance, Th1 cells secrete IFN-γ that inhibits the proliferation of Th2 cells. IL-4, which is produced by Th2 cells, suppresses Th1 development and secretion of IFN-γ by Th1 cells. In immunoregulation, Th1/Th2 dysfunction plays an important role in the pathogenesis of asthma. Likewise, Lancaster et al. demonstrated that acute exercise markedly affects the distribution of both Th1 and Th2 cells (7).
Recent studies suggest that immune tolerance damage is important in the pathogenesis of asthma (8). Numerous animal studies have shown that regulatory T cells (Treg) cells can actively suppress the development of autoimmune and allergic responses in vivo, due to the suppression of both Th1 and Th2 responses (9). Treg is a kind of cells regulating or inhibiting the function of other immune cells, which can not only express cell surface molecules CD4 and CD25, but also express a distinct intranuclear protein Foxp3 considered as a specific marker of Treg (10). Two distinct subsets of Tregs have been described to date, the best established are CD4+ CD25+ Tregs, which emerge from the thymus: natural Tregs (nTreg). The other category of Treg cells also derives from the thymus but acquires its suppressive activity in peripheral tissues: adaptive Tregs (aTreg), which never express Foxp3 (4). However, Foxp3 can act as a silencer of cytokine gene promoters and programs the development and function of CD4+ CD25+ T cells (9). Increasing evidence demonstrates that the ability of CD4+ CD25+ T regulatory (Treg) cell to down-regulate immune responses associated with asthma in experimental animal models has recently ignited interest in defining the role of Treg cells in asthma in humans (11-13). Moreover, regulatory T lymphocytes, including CD4+ CD25+ Foxp3+ regulatory T cells, play a central role in suppressing asthma pathogenesis (14). In addition, a number of different Treg populations have been described although the best understood to date are CD4+ Treg. A major CD4+ Treg population are those deriving from the thymus, which constitute a small percentage of the CD4+ T cell population in humans in the periphery (15).
Existing experiments found that Foxp3-mutant mice were associated with the presence of allergic airway inflammation, markedly increased IgE and eosinophils and Th1/Th2 cytokine imbalance (16). Fontenot et al. (17) found that the number of in vivo CD4+ CD25+ Treg in Foxp3-mutant and Foxp3-deletion mice was decreased. Studies on the association between Treg and asthma have focused on children with established asthma (18) and a majority of cases of asthma are diagnosed in early childhood (13). Till now, the interactions between various T cell subsets and cytokines are still at the stage of exploration and research. This study hopes to analyze the association between various T cell subsets and severity of asthma and control of its symptoms through detecting the changes in the proportion of various T cell subsets in peripheral blood of children with asthma, with the purpose of providing clinical evidence for clinical diagnosis and prognostic judgment of asthmatic children and further exploring the pathogenesis of asthma.
Materials and methods
Clinical data
A total of 150 asthmatic children admitted to the Nanjing Children’s Hospital affiliated to Nanjing Medical University from March 2009 to March 2010 were included in this study, including 86 males and 64 females aged 8 months to 12 years old with an average age of 5.6 years. Diagnostic criteria are according to the Global Initiative for Asthma (GINA) guidelines (19). The 150 cases of asthmatic children were allocated into the acute phase group (n=94) and remission phase group (n=56). The acute phase group was reassigned into the mild group (n=54) and severe group (n=40). Fifty cases undergoing physical examination were chosen as the control group, including 27 males and 23 females aged 15 months to 15 years old with an average age of 7.5 years, who were all healthy children without allergic diseases or recent respiratory infections. All subjects had no history of malignancies or autoimmune diseases, and received no glucocorticoids or other immunosuppressive agents within the recent four weeks.
Experiments methods
Reagents and equipments
Fluorescein isothiocyanate (FITC)-labeled mouse anti-human CD4 monoclonal antibody and phycoerythrin (PE)-labeled mouse anti-human CD25 monoclonal antibody as well as its matched isotype control were all purchased from the US BD PharMingen Cooperation. Allophycocyanin (APC)-labeled mouse anti-human Foxp3 monoclonal antibody and Fixation/Perm were purchased from the US eBiosicence Cooperation. PE-CY5 (PC5)-labeled mouse anti-human CD3 monoclonal antibody, PC7-labeled anti-human CD8 monoclonal antibody, FITC-labeled mouse anti-human IFN-γ monoclonal antibody, PE-labeled mouse anti-human IL-4 monoclonal antibody and Fix&Perm were all purchased from the US Backman Cooperation. The irritant agent (Leukocyte Activation Cocktail) was purchased from the US BD PharMingen Cooperation. Red blood cell lysis buffer was 0.83% ammonium chloride and the washing liquid was PBS containing 0.5% fetal calf serum. The flow cytometer (FACSCanto) was purchased from the US BD Cooperation.
Treg detection
Draw 1 mL early morning fasting venous blood and 100 µL whole blood from the children using the heparin anticoagulant tube and add 10 µL CD4-FITC and CD25-PE irritant agent for incubation at 4 °C for 30 min; add 1 mL red blood cell lysis buffer ammonium chloride for 10 min and rinse 3 times in PBS for centrifugation at 1,200 rpm/min for 5 min; add 1 mL Fixation/Perm buffer transmembrane for 45 min, rinse in PBS and afterwards, directly add 10 µL APC-labeled mouse anti-human Foxp3 monoclonal antibody for incubation in a dark place at 4 °C for 30 min. Rinse twice and resuspend cells with 300 µL flow cytometry staining buffer before detection on a FACSCanto flow cytometer. BD FACSDiva software was applied to analyze data and calculate the percentage of Foxp3+ cells in CD4+ cells. A total of 1×104 cells were detected each time for each sample.
Th1/Th2 detection
Draw 100 µL whole blood specimens, dilute the specimens with RPMI 1640 (containing no calf serum-FBS) at a volume ratio of 1:1 and add 10 µL irritant agent for incubation at 37 °C in a 5% CO2 incubator for 4-6 h. After blending, add 10 µL CD3-PC5 and 10 µL CD8-PC7 for incubation protecting form light at room temperature for 15 min; add 100 µL Reagent 1 (namely fixative) in Fix&Perm for incubation protecting form light at room temperature for 15 min; add 3 mL PBS for centrifugation at 1,200 rpm for 5 min, discarding the supernatant. Add 100 µL Reagent 2 Fix&Perm (namely ruptured membrane and hemolysate) into each tube and add 10 µL IFN-γ-FITC and IL-4-PE at the same time into each tube for incubation protecting from light for 15 min. Add 3 mL PBS for centrifugation at 1,200 rpm for 5 min, discarding the supernatant; resuspend cells using 0.5 mL PBS before detection on a FACSCanto flow cytometer.
A total of 1×104 cells were detected each time for each sample.
Statistical analysis
Experimental data were expressed as mean + SD (
Results
Treg and Th1/Th2 detection
Flow cytometry was applied to detect the expression of CD4+CD25+Foxp3+ Treg, CD4+IFN-γ+ Th1 and CD4+IL-4+ Th2 cells (Figure 1,2).


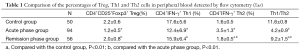
Comparison of CD4+CD25+Foxp3+ Treg levels in different groups
The percentage of CD4+CD25+Foxp3+ Treg in CD4+ T cells was (1.5+0.9)% in peripheral blood of asthmatic children, significantly lower than that in the control group [(2.2+0.6)%] (t=6.086, P<0.01). The percentage of CD4+CD25+Foxp3+ Treg in CD4+ T cells in peripheral blood of asthmatic children was significantly lower in the acute phase group than the remission phase group and control group (t=6.979, t=9.884; P<0.01); the difference between the remission phase group and the control group was statistically insignificant (P>0.05) (Table 1). The percentage of CD4+CD25+Foxp3+ Treg in CD4+ T cells was (0.9±0.5)% in peripheral blood of asthmatic children in the severe group, significantly lower than that in the mild group [(1.3+0.7)%], t=3.595, P<0.01.
Full table
Comparison of Th1/Th2 levels in different groups
Classification of Th subsets in asthmatic children was remarkably changed compared to the control group. The percentage of CD4+IFN-γ+ Th1 in peripheral blood of asthmatic children was lower in the acute phase group than the remission phase group (t=3.146, P<0.01) and the control group (t=4.884, P<0.01); the percentage of CD4+IL-4+ Th2 in asthmatic children was higher in the acute phase group than the remission phase group and control group (t=11.384, 12.34; P<0.01); therefore, the Th1/Th2 ratio in peripheral blood of asthmatic children was significantly lower in the acute phase group than the remission phase group and control group (t=22.635, 50.565; P<0.01), suggesting obvious imbalance in Th subsets of asthmatic children in the acute phase group. The results between the remission phase group and control group showed that there was also statistical significant difference in CD4+IL-4+ Th2 and the ratio of Th1/Th2 (t=2.056, 10.427; P<0.01) (Table 1). The ratio of Th1/Th2 in peripheral blood of asthmatic children was statistically lower in the severe group than the mild group (3.4+0.4 vs. 6.9+1.5), t=14.07, P<0.01.
Changes in Treg and the Th1/Th2 ratio in asthmatic children and its association with asthma
Spearman correlation analysis showed that the Treg level in peripheral blood was negatively correlated with severity of asthma in asthmatic children (r=-0.737, P<0.01) and the ratio of Th1/Th2 was also negatively correlated with the severity of asthma (r=-0.615, P<0.01), but the level of Treg was positively correlated with the ratio of Th1/Th2 (r=0.856, P<0.01). Namely, the lower the Treg level and Th1/Th2 ratio in peripheral blood were in asthmatic children, the more severe asthma became.
Discussion
With the rapid development of immunology, a large number of studies have demonstrated the onset of asthma is related with immune dysfunction (8). In chronic allergic airway inflammation, there are a variety of inflammatory cells, inflammatory mediators and cytokines involved in the inflammatory process. T lymphocytes and its secretion of various cytokines play an important role in this process. As the research progresses, the effect of T helper cells (Th1/Th2) and Treg on asthma has been paid more and more attention, becoming a new way of shedding light on revealing the pathogenesis of asthma.
Cross-regulation and mutual inhibition exhibit between Th1 and Th2 cells through secretion of cytokines (20). Th1 cells can secret IL-2 and IFN-γ and induce cellular immunity, so they are also important effector cells in type IV allergic reaction and can suppress the excessive immune response mediated by Th2 cells. Th2 cells can secret IL-4 and IL-5. IL-4 can promote mast cell growth and synthesis of IgE; IL-5 can not only induce eosinophilic precursor proliferation and differentiation, but also induce chemotaxis and activation of mature eosinophils (21). Existing studies have found that imbalance of the Th1/Th2 ratio plays a key role in the pathogenesis of asthma (22). The results of this study indicated that, compared with the control group and remission phase group, the acute phase group had a significantly lower Th1 level while a significantly increased Th2 level and thus a markedly decreased Th1/Th2 ratio in peripheral blood, prompting that research on Th cell subsets shall play an important role in clinical diagnosis and judgment of prognosis in asthmatic children.
Treg is a group of T cells with immunosuppressive effect found in recent years, which plays an important role in maintaining autotolerance and inhibiting the occurrence and development of autoimmune diseases (23). The majority of Treg are CD4+ T cells with a high expression of CD25 and Foxp3 (24), which can control autoimmune diseases through regulating peripheral immune tolerance (25). The mechanism of Treg in the pathogenesis of asthma still remains undefined. Gao et al. (26) observed that CD4+CD25+ Treg was significantly lower in the spleen of a mouse model of asthma than that in normal mice, and its number and inhibitory function were weakened or hyporeactive, considering that the reduced number and inhibitory function of Treg or hyporesponsiveness might account for one of the causes for bronchial asthma. Jaffar et al. (27) have indicated that CD4+ CD25+ Treg can strongly inhibit the formation of Th2 promoting eosinophilic airway inflammation in vivo and airway aggregation of Th2-induced eosinophils. Taylor et al. (28) have also speculated that Treg cells can inhibit IL-4, IL-5 and IL-13 produced by Th2 cells through secreting IL-10 and TGF-β, thereby reducing the generation of IgE; suppressing the inflammation-causing effect of eosinophils, basophils and mast cells can inhibit allergic inflammation directly. However, experimental results of Shi et al. (29) found that the number of blood CD4+CD25+ Treg was significantly increased at the acute attack phase in patients with allergic asthma, but not increased in those at the stable phase of asthma or with non-asthmatic allergy, or normal population, and the inhibitory effect of CD4+CD25+ Treg on Th1 and Th2 did not differ. This study found that the Treg level in peripheral blood of children was significantly lower in the asthma group than the normal control group, suggesting in vivo presence of Treg cell immunity imbalance in children with asthma and low expression of CD4+ CD25+ Treg cells, thus unable to inhibit activation and proliferation of CD4+ T cells and CD8+ T cells effectively. At the same time, the research also showed that the Treg level in peripheral blood of asthmatic children was significantly lower in the acute phase than the remission phase group and normal control group, but the difference was statistically insignificant between the remission phase group and the normal control group, supporting the hypothesis that reduced suppression of immune function or hyporesponsiveness caused by decreased number of Treg may account for one of the pathogeneses leading to bronchial asthma, and also indicating remission of symptoms in children with asthma might be associated with in vivo restoration of the Treg level.
The relationship of Th1/Th2 and Treg levels with severity of asthma in asthmatic children has rarely been reported. This study showed that among children at the asthma attack phase, the Treg level and Th1/Th2 ratio in peripheral blood were significantly lower in the severe group than the mild group, and with exacerbation of the disease, the Treg level and Th1/Th2 ratio were both significantly decreased. In addition, the Treg level and Th1/Th2 ratio maintained strong consistency during the development of asthma. The possible mechanism: with exacerbation of asthma, allergen stimulation to the body increased, resulting in a reduced percentage of Treg in peripheral blood and impaired immunomodulatory function, which further caused massive activation and proliferation of Th2 cells, inhibited Th1 cells and led to Th1/Th2 imbalance, thus further increasing the secretion of IgE antibody and generating a large number of inflammation-causing factors to mediate an asthma attack (30,31).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Du J, Tao WH, Zuo Y, et al. Effect of signal transducer and activators of transcription 5 on airway inflammation of rats with asthma. Journal of Xinxiang Medical College 2008;25:346-8.
- Robinson DS. Regulatory T cells and asthma. Clin Exp Allergy 2009;39:1314-23. [PubMed]
- Larché M, Robinson DS, Kay AB. The role of T lymphocytes in the pathogenesis of asthma. J Allergy Clin Immunol 2003;111:450-63. [PubMed]
- Yüksek M, Erol F, Güloğlu D, et al. Regulatory T cell levels in children with asthma. Turk J Pediatr 2011;53:532-6. [PubMed]
- Akbari O, Stock P, DeKruyff RH, et al. Role of regulatory T cells in allergy and asthma. Curr Opin Immunol 2003;15:627-33. [PubMed]
- Corthay A. How do regulatory T cells work? Scand J Immunol 2009;70:326-36. [PubMed]
- Lancaster GI, Halson SL, Khan Q, et al. Effects of acute exhaustive exercise and chronic exercise training on type 1 and type 2 T lymphocytes. Exerc Immunol Rev 2004;10:91-106. [PubMed]
- Smit JJ, Boon L, Lukacs NW. Respiratory virus-induced regulation of asthma-like responses in mice depends upon CD8 T cells and interferon-gamma production. Am J Pathol 2007;171:1944-51. [PubMed]
- Taylor A, Verhagen J, Akdis CA, et al. T regulatory cells and allergy. Microbes Infect 2005;7:1049-55. [PubMed]
- Finotto S. T-cell regulation in asthmatic diseases. Chem Immunol Allergy 2008;94:83-92. [PubMed]
- Kearley J, Barker JE, Robinson DS, et al. Resolution of airway inflammation and hyperreactivity after in vivo transfer of CD4+CD25+ regulatory T cells is interleukin 10 dependent. J Exp Med 2005;202:1539-47. [PubMed]
- Strickland DH, Stumbles PA, Zosky GR, et al. Reversal of airway hyperresponsiveness by induction of airway mucosal CD4+CD25+ regulatory T cells. J Exp Med 2006;203:2649-60. [PubMed]
- Ly NP, Ruiz-Perez B, McLoughlin RM, et al. Characterization of regulatory T cells in urban newborns. Clin Mol Allergy 2009;7:8. [PubMed]
- Lowder T, Dugger K, Deshane J, et al. Repeated bouts of aerobic exercise enhance regulatory T cell responses in a murine asthma model. Brain Behav Immun 2010;24:153-9. [PubMed]
- Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol 2004;22:531-62. [PubMed]
- Lin W, Truong N, Grossman WJ, et al. Allergic dysregulation and hyperimmunoglobulinemia E in Foxp3 mutant mice. J Allergy Clin Immunol 2005;116:1106-15. [PubMed]
- Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol 2003;4:330-6. [PubMed]
- Hartl D, Koller B, Mehlhorn AT, et al. Quantitative and functional impairment of pulmonary CD4+CD25hi regulatory T cells in pediatric asthma. J Allergy Clin Immunol 2007;119:1258-66. [PubMed]
- Global Initiative for Asthma. Pocket guide for asthma management and prevention. NIH Publication No. 02-3659, Updated 2005.
- Capron M, Woerly G, Kayaba H, et al. Invited lecture: role of membrane receptors in the release of T helper 1 and 2 cytokines by eosinophils. Int Arch Allergy Immunol 2001;124:223-6. [PubMed]
- Shi HZ, Xiao CQ, Zhong D, et al. Effect of inhaled interleukin-5 on airway hyperreactivity and eosinophilia in asthmatics. Am J Respir Crit Care Med 1998;157:204-9. [PubMed]
- Jiang YH, Wang YQ, Sun KZ. Polarization and immune regulation of TH cells in children with bronchial asthma. Zhongguo Dang Dai Er Ke Za Zhi 2006;8:379-81. [PubMed]
- Manni JA, Guilleron C, Araujo HA. Lymphocyte imbalance in autoimmunity. Medicina (B Aires) 1989;49:105-8. [PubMed]
- Hanaki K, Momo A, Oku T, et al. Semiconductor quantum dot/albumin complex is a long-life and highly photostable endosome marker. Biochem Biophys Res Commun 2003;302:496-501. [PubMed]
- Li YY, Feng XB. The researches on CD4+CD25+ Treg in bronchial asthma. Int J Intern Med 2007;34:545-8.
- Gao ZY, Zhang DQ, Xiao JQ, et al. Experimental Study of Relationship Bctween CD4+ /CD25+ Regulatory T Cells and Asthma. Journal of Chinese Microcirculation 2004;8:249-50.
- Jaffar Z, Sivakuru T, Roberts K. CD4+CD25+ T cells regulate airway eosinophilic inflammation by modulating the Th2 cell phenotype. J Immunol 2004;172:3842-9. [PubMed]
- Taylor PA, Noelle RJ, Blazar BR. CD4+CD25+ immune regulatory cells are required for induction of tolerance to alloantigen via costimulatory blockade. J Exp Med 2001;193:1311-8. [PubMed]
- Shi HZ, Li S, Xie ZF, et al. Regulatory CD4+CD25+ T lymphocytes in peripheral blood from patients with atopic asthma. Clin Immunol 2004;113:172-8. [PubMed]
- Huang HR, Liu TT, Wei J, et al. Changes of CD4+CD25+ regulatory T cells and their relation with the allergic physique and the levels of IgE in peripheral blood of asthmatic children. Chin J Clinicians 2004;3:780-4. (Electronic Edition).
- Li M, Song L, Zhang JB, et al. Effect of glucocorticoid on CD4+CD25+ T regulatory cells in asthmatic mice. Zhongguo Dang Dai Er Ke Za Zhi. 2008;10:527-30. [PubMed]


